![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
What are the (3) major functions of the cardiovascular system?
|
1) Rapid transport of O2 & nutrients while removing CO2 (H+) waste
2) Control system: distribute hormones to tissues 3) Regulate body temp |
|
|
What is the basic organization of the cardiovascular system?
|
Heart: Right ventricle (RV) & left ventricle (LV) are essentially the pumps being filled by the right atrium (RA) & left atrium (LA)
Pulmonary & systemic circulation: RV pumps deoxygenated blood through pulmonary arteries to lungs. O2 diffuses into blood and CO2 diffuses out and exhaled. Oxygenated blood returns to LA via pulmonary veins followed by the LV pumping out to systemic circulation |
|
|
Why must the output from the left heart be approximately equal to that of the right heart?
|
In order to maintain 5L of output from the left we must also bring in 5L. If we brought in more then then heart would eventually start to expand w/ blood. If we brought in less then the output on the left would also have to decrease as not as much blood would be present
|
|
|
What is systole and diastole?
|
Systole - is the contraction phase
Diastole - is the relaxation phase |
|
|
What is included in the pulmonary circulation?
What is included in the systemic circulation? |
Pulmonary circulation is from RV to lungs and back to LA
Systemic circulation is from LV through major arteries & repeated branching eventually giving rise to capillaries and then through veins and back to the RA |
|
|
What is a portal system?
What are the (3) major portal systems? |
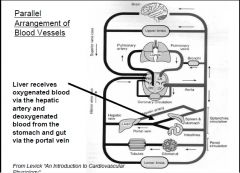
Portal systems don't follow a parallel arrangement, such that some organs are connected in series w/ another organ so they receive venous outflow from that organ
1) Liver - direct arterial supply from hepatic artery but ~70% of supply comes from hepatic portal vein (from gut & spleen - adv. being digestive products processed further in liver) 2) Kidney - Afferent arterioles supply glomeruli and efferent take it away which supply kidney tubules 3) Hypothalamus to pituitary gland w/ functions to transport hypothalamic hormones to pituitary |
|
|
Define cardiac output?
What does venous return mean? |
Cardiac output (CO) - volume of blood ejected from one ventricle per minute
Venous return (VR) is the volume of blood returning to the RA from vena cava or to LA from pulmonary vein per minute |
|
|
What is stroke volume (SV) and how is it calculated?
What is the ~ CO from the LV & RV of a healthy 20 year old male weighing 70kg? What is the ~ SV of a "normal" 70kg male w/ an average HR of 72? |
Stroke volume (SV) is the volume of blood ejected (from either ventricle) per heart beat
SV = CO/HR LV & RV CO will be 5L or a "normal" person SV = 5000ml/72bpm SV = ~70ml |
|
|
What is the law of flow?
What is Darcy's (or Bulk) Law of Flow? |
Flow (F) is a volume of fluid transferred per unit time
(F) = ΔP/R (resistance) |
|
|
How does Darcy's Law of Flow explain the pressure changes seen across the circulation?
|
Darcy's Law of Flow states flow is equal to ΔP/R (resistance). Blood flow is inversely proportional to resistance which is related to diameter of blood vessels. Total cross sectional area is equal to cross sectional area of one vessel times the # of vessels. We know capillaries have the largest total area b/c of the # of capillaries throughout our system. The increased area decreases the P & R but we see little change in ΔP. However, the total pressure and resistance throughout all capillaries will equal that which is expelled from the heart. Thus flow will also decrease per capillary b/c ΔP & R are both small
However, the greatest pressure drop will be through the arterioles! |
|
|
What are the (5) different classes of blood vessels and how is their morphology is suited for various functions?
|
1) Elastic (aorta)- distensible, able to handle high pressures, prevent being overstretched and able to recoil
2) Conduit (muscular arteries) - smooth muscle can contract or relax to alter vessel diameter 3) Resistance (arterioles) - sites of highest resistance, richly innervated by SNS, areas where blood flow to organ is regulated, pulsatile flow is smoothed out to constant flow 4) Exchange (capillaries) - exchange of nutrients and waste products 5) Capacitance (venules, peripheral & central veins) - veins can alter diameter to increase pressure, venules can still exchange nutrients and waste products |
|
|
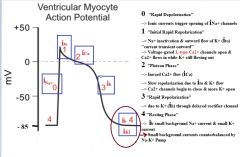
Explain the ventricular myocyte cell action potential?
|
|
|
|
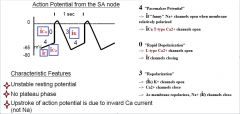
Explain the SA node action potential?
|
|
|
|
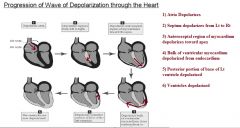
Explain how the wave of depolarization spreads throughout the heart?
|
|
|
|
What are the (2) advantages and (1) disadvantage of the delayed conduction at the AV node?
|
Advantages:
1) Allows time for atria to contract before ventricles contract...thus more blood can be pushed into ventricles 2) Atrial tachyarrhythmias may not be transmitted to the ventricles...safeguarding the ventricles Disadvantages: 1) Low safety factor for transmission (can lead to conduction blocks) |
|
|
Why is the SA node the pacemaker of the heart?
|
SA node -> 60-75 bpm
AV node -> 50 bpm Bundle of His -> 40 bpm Purkinje fibres -> 15 bpm SA node action potential forces all the other pacemaker cells to fire during SA action potential, in turn never allowing those cells to take over control unless something happens to the SA node |
|
|
How does the PNS decrease HR?
|
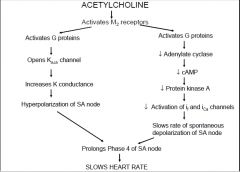
PNS:
The vagus nerve postganglionic fibers are within the myocardium itself and release Ach which binds M2 receptors. |
|
|
How does the SNS increase HR?
|
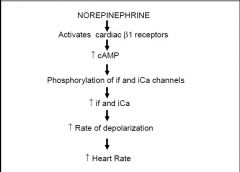
|
|
|
What is a dipole?
How do dipoles generated across the surface of the heart produce waveforms of ECG's? |
A dipole is a separation of positive and negative charges
At rest the outside of the heart is positively charged (inside is negative). Electrodes on the skin will record no potential differences. When the muscle depolarizes a portion of it becomes more negative due to depolarization. The skin electrodes will record a positive ECG deflection when the wave of depolarization is moving in the direction of the +'ve electrode of a specific lead. It will also record a negative ECG deflection when the wave is moving away from a particular lead, such as a -'ve lead electrode, while the depolarization is still in the +'ve direction. |
|
|
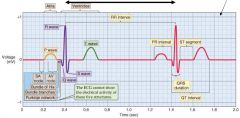
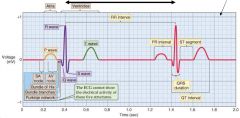
Describe the typical bipolar Lead II ECG waveform? (waves, intervals, segments and electrical state)
|
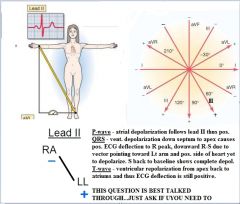
This question is best talked through. Just can't put all that on one card!!!! Let me know if you wanna talk this through!!!
|
|
|
Correlate a typical ECG wave form w/ a cardiac action potential? (QRS, T wave)
|
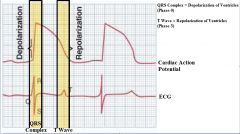
|
|
|
What is meant by electrical vectors in an ECG? (what does it represent, dipole, where does it point?
|
In an ECG, electrical vectors (arrows) represent potential differences, length (size of arrow), and orientation (position arrow is pointing) of a dipole on the surface of the heart.
The vector always points to the positive pole (of dipole) and its length is a measure of the size in potential differnce. |
|
|
What are the electrode placements & polarities of both bipolar and augmented limb leads?
|
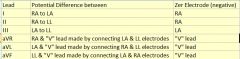
|
|
|
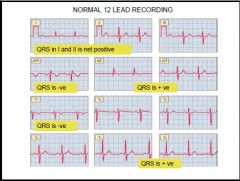
Why does the ECG trace look different in each of the 12 leads?
|
The ECG trace is recording the electrical potential difference on the outside of the heart, which establishes an electrical vector. This vector when going toward the pos. electrode of any given lead will give a pos. deflection. If the vector is going toward the neg. electrode of any given lead it will give a neg. deflection.
Thus each lead will have a slightly different trace due to the electrical vector and its relation to that lead, pointing more toward the negative or positive electrode of each lead. |
|
Calculate:
HR? Duration of atrial depolarization? AV conduction time? Duration of ventricular depolarization? |
HR: 57 bpm [60/(26 x 0.04)]
Duration of atrial dep.: 0.12s [3 x 0.04 (P-wave)] AV conduction: 0.16s [4 x 0.04 (P-R interval] Duration of ventricular dep.: 0.08s [2 x 0.04 (QRS complex)] |
|
|
How do we measure HR on an ECG?
What is the HR for NSR (normal sinus rhythm)? What is the HR for Bradycardia & Tachycardia? |
# of small boxes between R-R interval times 26 = seconds per beat...60 sec / seconds per beat
NSR: 60 - 99 bpm Tachycardia: >100 bpm Bradycardia: <60 bpm |
|

What is the pathological condition which caused this ECG?
|

1st Degree AV Block
|
|

Is this NSR?
|

Yes
|
|
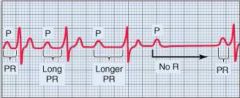
What is the pathological condition which caused this ECG?
|
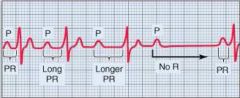
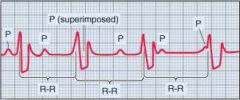
2nd Degree Block: Mobitz Type I
|
|
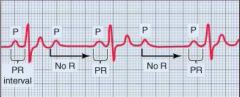
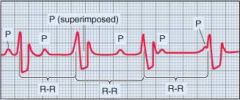
What is the pathological condition which caused this ECG?
|
2nd Degree Block: Mobitz Type II
|
|

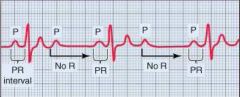
What is the pathological condition which caused this ECG?
|

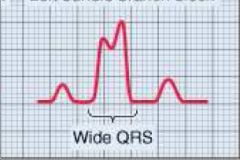
2nd Degree Block: Right Bundle Branch Block
|
|
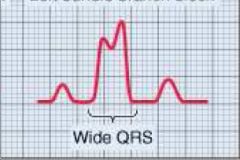
What is the pathological condition which caused this ECG?
|
2nd Degree Block: Left Bundle Branch Block
|
|
What is the pathological condition which caused this ECG?
|
3rd Degree Block: Complete Conduction Block
|
|
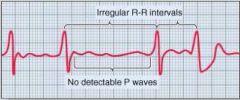
What is the pathological condition which caused this ECG?
|
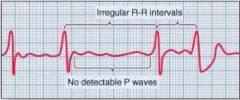
Atrial Fibrillation
|
|

What is the pathological condition which caused this ECG?
|

Ventricular Fibrillation
|
|
|
What is the Mean Electrical Axis (MEA) of the heart?
|
The net direction of the wave of excitation going through the heart during depolarization
|
|
|
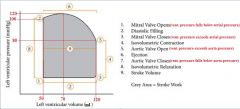
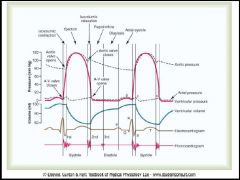
Describe the pressure and volume changes in the sequence of events that occur during one cardiac cycle? (atrial systole & diastole, ventricular systole & diastole)
|
Atrial systole: atrial contraction increases atrial pressure while decreasing volume. Blood being pushed into ventricles and just prior to ventricular systole, this volume of blood is called end-diastolic volume (EDV).
Atrial diastole: atrial relaxation w/ decreased pressures and volumes. Volume increase throughout diastole w/ a slight increase in pressure Ventricular systole: ventricular contraction increases pressures while volume stays the same (isovolumetric contraction) until ventricular pressure overcomes the pulmonary & systemic pressures which then decreases volume in ventricles Ventricular diastole: ventricular relaxation w/ decreased volumes and pressures. Volume increases throughout diastole w/ slight decrease in pressure due to suction exerted by elastic recoil and then a slight increase in pressure. |
|
|
Explain the cardiac pressure-volume loop?
|
|
|
|
What is the mean pressure in the RA & LA?
What is the mean pressure in the RV during systole & diastole? What is the mean pressure in the LV during systole & diastole? What is the mean pressure in the pulmonary arteries during systole & diastole? What is the mean pressue in the Aorta during systole & diastole? |
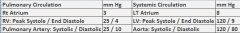
|
|
|
How would an increase in HR affect the cardiac cycle? (systole & diastole)
What is the minimum time required for diastolic filling for adequate EDV that will yield an adequate CO? What is the major factor limiting the maximum useful heart rate? |
Increased HR would: decrease both systole & diastole,
Diastolic filling a minimum of ~0.13s The diastolic interval regulates how much time is given to refilling the heart. Thus if this interval is limited, so will the maximum useful heart rate. |
|
|
What is the central venous pressure (CVP)?
How does this relate to the RA? |
CVP is the amount of blood returning to the heart
RT atrium pressures are generated up into the jugular veins b/c there is no valve separating the two structures |
|
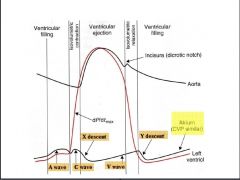
What does the A wave represent?
What does the C wave represent? What does the X descent represent? What does the V wave represent? What does the Y descent represent? |
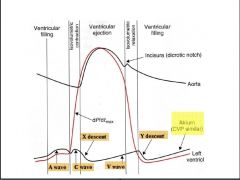
A wave: increase in pressure due to atrial systole
C wave: tricuspid and mitral valves bulge back into atrial chambers...also...expansion of carotid artery pressing on internal jugular during systole X descent: atrial relaxation V wave: atrial filling Y descent: atrial emptying |
|
|
Be able to explain how the cardiac cycle and ECG overlap?
|
|
|
|
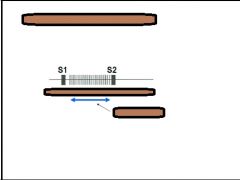
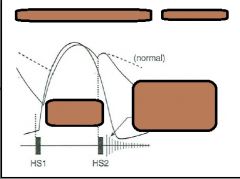
What are the (2) normal heart sounds and what do they represent?
What are the (2) additional heart sounds and what do they represent? |
Normal sounds:
S1 - "lubb" represents closure of A-V valves (tricuspid & mitral) S2 - "dubb" represents closure of semilunar valves (aortic & pulmonary) Additional sounds: S3 - rush of blood through valve into relaxing ventricles during early diastole (common in young) S4 - atrial systole, occurs just before S1 and usually represents stenosis of valve |
|
|
Why is there an S2 splitting?
|
RV has slightly shorter period of isovolumetric contraction than LV. The pulmonary valve opens slightly before the aortic valve. The aortic valve closes slightly before the pulmonary valve b/c of greater pressures downstream. Thus the pulmonary valve opens first and closes last.
It can also be more prominent during inspiration |
|
|
What would cause the S1 sound to be split?
|
Bundle Branch Block
|
|
|
What are the two types of heart murmurs?
|
Incompetence: failure of valve to seal properly such that it becomes leaky allowing blood to regurgitate
Stenosis: open valve is narrowed so that higher pressure gradients are needed to drive blood through |
|
|
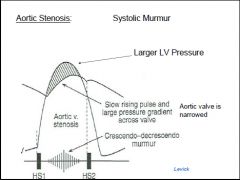
What is aortic stenosis?
|
Aortic stensosis is a "Systolic murmur" and a narrowing of the arotic valve heard during the ejection phase of ventricular systole
|
|
|
What is a Mitral incompetence?
|
Mitral incompetence is a "Pan systolic murmur" where ventricular systole causes blood to regurgitate through the mitral valve back into the LA. Resulting in murmur throughout ventricular contraction - called a pansystolic murmur
|
|
|
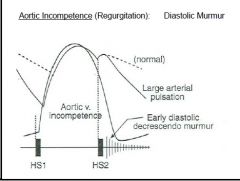
What is an Aortic incompetence?
|
Aortic incompetence is a "Diastolic murmur" of the aortic valve not closing completely allowing blood to regurgitate into ventricle during diastole.
Begins at S2 and last through early part of diastole. Increases pulse pressure. |
|
|
What is Mitral stenosis?
|
Mitral stenosis is a "Diastolic murmur" where blood is forced through narrowed mitral valve during ventricular diastole
|
|
|
What is Benign systolic murmur?
|
Benign systolic murmur is turbulence in the ventricular outflow. Its common in youth and during pregnancy, strenuous exercise and anemia
|
|
What type of heart murmur is this?
During the systolic or diastolic phase? |
|
|
What type of heart murmur is this?
|

Mitral or Tricuspid incompetence
"Pan systolic" - steady sound throughout entire contraction |
|
What type of murmur is this?
Does it occur during the systolic or diastolic phase? |
|
|
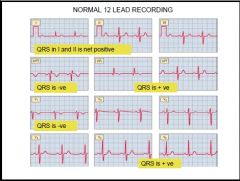
Based on your understanding of the QRS magnitudes of deflection, what is the mean electrical axis?
|
Normal axis ~ 30 deg. when looking at leads 1 & 2
|
|
|
What mean QRS axis would you expect to see in someone w/ Lt. ventricular hypertrophy?
What mean QRS axis would you expect to see in someone w/ Rt. ventricular hypertrophy? What is the normal mean QRS axis range? |
Lt. ventricular hypertrophy: >-30 deg.
Rt. ventricular hypertrophy: >90 deg. Normal: -30 to +90 deg. |
|
|
What are the ECG changes we should expect to see in someone with ischemia, injury and necrosis of cardiac tissue?
|
S-T segment elevation & T wave inversion
|

