![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
|
When do congenital defects usually arise?
|
Arise during embryogenesis. Usually weeks 3-8.
|
|
|
Congenital defects are seen in about _________ of live births.
|
1%
|
|
|
Most defects that are formed in embryogenesis are ______.
|
sporadic
|
|
|
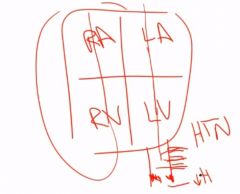
A congenital heart defect often results in ______________.
|
shunting between left and right circulations
|
|
|
What is a VSD?
|
Defect in the septum that divides the right and left ventricles.
|
|
|
This is the most common congenital heart defect.
|
VSD
|
|

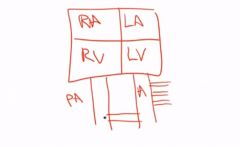
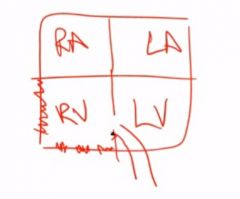
What heart defect is associated with this?
|
VSD
|
|
|
What can a VSD lead to, if it's severe enough? Consequences?
|
Eisenmenger's syndrome:
Blood flows into right ventricle (L-->R shunt) and into the pulmonary vasculature. In time, pulmonary hypertension develops. This reverses the shunt. Blue blood enters the left ventricle producing cyanosis. Right ventricular hypertrophy Cyanosis may cause polycythemia. Clubbing due to cyanosis |
|
|
What determines when a VSD presents?
|
(1) Size of defect determines extent of shunting
(2) Age at presentation |
|
|
VSD defects that are small often are ___________.
|
asymptomatic
|
|
|
Treatment of VSD?
|
(1) Surgical closure
(2) Small defects may close spontaneously |
|
|
What is the MC type of ASD?
|
Most common type is ostium secundum
|
|
|
Bonus: Triple marker for Down syndrome?
|
(1) AFP decreased
(2) hCG increased (3) Urine estriol decreased |
|
|
A person with Down syndrome would have what heart defect?
|
ASD; Ostium primum type.
|
|
|
You auscultate a person with Down syndrome. You hear a split S2. What is going on and why a split S2?
|
ASD.
The extra blood volume coming from the RA will cause a delayed closure of the pulmonic valve. |
|
|
A lazy down syndrome patient is known to have DVT. All of a sudden he develops a hemiparesis and complains of loss of sensation in the face. What might be going on?
|
Paradoxical embolus via ASD to lodge in MCA.
|
|
|
What is PDA?
|
Patent ductus arteriosus. Failure of it to close.
|
|
|
PDA is associated with?
|
Congenital rubella
|
|
|
Consequences of PDA?
|
Like in ASD, blood will flood the pulmonary circuit causing pulmonary HTN. It will reverse the shunt. Deoxygenated blood is now in the systemic circuit and goes to the LOWER extremities (later in life).
|
|
|
A baby is born. On auscultation you hear a holosystolic 'machine-like' murmur. What might be going on?
|
PDA
|
|
|
PDA is ___________ (symptomatic/asymptomatic) at birth.
|
asymptomatic
|
|
|
Treatment of PDA?
|
Indomethacin. Decreases PGE2, resulting in PDA closure.
("Prostaglandin E is necessary to kEEEEEEEEEP it open") |
|
|
How many problems do we have in tetralogy of fallot?
|
Four
|
|
|
What defects are there in tetralogy of fallot?
|
(1) Stenosis of RV outflow tract
(2) RV hypertrophy (3) VSD (4) Aorta that overrides the VSD |
|
|
What shunt are babies with tetralogy of fallot born with?
|
R-->L
Early cyanosis is seen in these babies. |
|
|
The extremities of a child becomes blue during exercise. What do we call this and what could the child do to alleviate this?
|
Cyanotic spell
Squat down to increase systemic bp and reverse the shunt temporarily. |
|
|
This is the MC cyanotic CHD.
|
Tetralogy of fallot
|
|

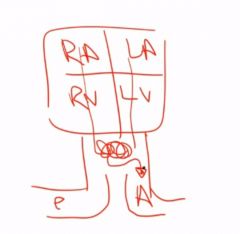
What is this?
|
A typical heart shape seen on X-ray in babies with tetralogy of fallot.
|
|
|
What is transposition of the great vessels?
|
A CHD where the pulmonary artery arises from the LV and aorta arises from the RV.
|
|
|
A mother has maternal diabetes. What is the child at risk for?
|
Transposition of the great vessels
|
|
|
What is the major problem in transposition of the great vessels?
|
Two separate circuits
|
|
|
You decide to close the PDA in a child with transposition of the great vessels. Why is this wrong?
|
PDA is the only connection that allow mixing of blood between the two independent circuits.
|
|
|
How does transposition of the great vessels present?
|
Presents with early cyanosis (like tetralogy, however, tetralogy is the MCC).
|
|
|
What is truncus arteriosus? What is it due to?
|
When you have one large trunk (vessel) arising from both ventricles.
It is due to the truncus failing to divide. |
|
|
How does truncus arteriosus present?
|
With early cyanosis.
Deoxygenated blood from the RV mixes with the oxygenated blood from the left ventricle before the independent circuits separate. |
|
|
What is tricuspid atresia?
|
Tricuspid valve orifice fails to develop (atresia means failure to form the lumen of a tube)
|
|
|
Features of tricuspid atresia?
|
(1) Early cyanosis
(2) RV hypoplasia |
|
|
What is coarctation of the aorta?
|

Narrowing of the aorta
|
|
|
How is coarctation of the aorta divided?
|
(1) Infantile form
(2) Adult form |
|
|
The infantile form of coarctation of the aorta is associated with what?
|
PDA
|
|
|
In the infantile form, where does the coarctation occur?
|
Distal to the aortic arch but proximal to the PDA.
|
|
|
Why would a baby with coarctation of the aorta present with lower extremity cyanosis?
|
Because coarctation causes a distally lower blood pressure than normal. This coupled with an intact PDA which is often seen in this context, allows for some blood from the RV and pulmonary trunk to mix and go to the extremities.
|
|
|
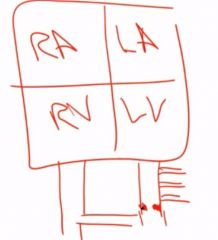
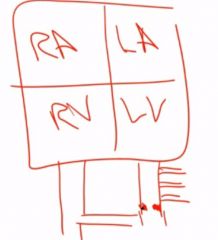
Bonus: How can you easily remember chromosomal number i turner and down syndrome?
|
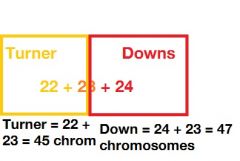
|
|
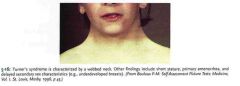
What heart defect is associated with this patients syndrome?
|
Infantile form of coarctation of the aorta
|
|
|
True or false: The adult form of coarctation of the aorta is associated with PDA.
|
False, it is not associated with a PDA.
|
|
|
How does the adult form of coarctation of the aorta present?
|
Presents as HTN in the upper extremities and hypotension with weak pulses in the lower extremities.
|
|
|
When is adult coarctation of the aorta classically discovered?
|
During adulthood.
|
|
|
Adults with coarctation of aorta are at risk for what types of aneurysm?
|
(1) Berry aneurysms
|
|
|
A man with pain in buttocks and calves when walking is found to have coarctation of the aorta. What other heart defects may this man have? The man is at risk for what complication due to this?
|
Bicuspid valve.
Bicuspid aortic valve increases risk and hastens disease onset of aortic stenosis (two valves has to do the work of three). AS is caused by age-related degenerative calcific changes of the valve ("wear and tear"). |
|
|
What might develop in a patient with coarctation of the aorta?
|
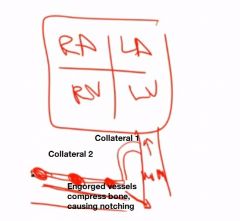
Collateral circulation can develop across intercostal arteries. Engorged arteries cause notching of ribs on x-ray.
|
|
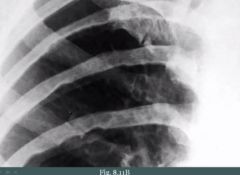
What congenital heart defect may this patient have?
|
We see notching of the ribs, suggesting engorged vessels due to coarctation of the aorta.
|
|
|
What may happen to the aorta in coarctation of the aorta?
|
Valve ring and aorta may dilate. Risk for dissection.
|

