![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
What does arteriosclerosis mean (the word itself)?
|
arterio - artery
sclerosis - hardening |
|
|
What three pathologic patterns to atherosclerosis are there?
|
(1) Atherosclerosis
(2) Arteriolosclerosis (3) Mönckeberg medial sclerosis |
|
|
In atherosclerosis we get a thickening of the __________ of the blood vessel wall. It usually occurs in what sized vessels?
|
intima
Usually occurs in medium- and large-sized blood vessels. |
|
|
Arteriolosclerosis usually occurs in what sized vessels?
|
small blood vessels
|
|
|
What happens in Mönckeberg medial sclerosis?
|
Calcification of the media of a blood vessel.
|
|
|
How does Mönckeberg medial sclerosis present?
|
It doesn't. It is clinically nonsignificant unless it is associated with atherosclerosis. Seen as incidental finding on X-ray or mammography.
|
|
|
What is atherosclerosis?
|
Intimal plaque that disrupts blood flow.
|
|
|
The plaque in atherosclerosis consists of what?
|
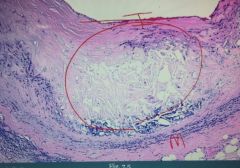
Mostly consists of a necrotic lipid core (key component is cholesterol). It has a fibromuscular cap. Core can often undergo dystrophic calcification
Inside the circle on the picture we see expansion of the intima with a necrotic lipid core. |
|
|
Pathognomonic lesion of atherosclerosis is __________.
|
fibrous cap
|
|
|
What is increased in patients with disrupted plaques?
|
CRP
|
|
|
Sites of atherosclerosis in descending order.
|
(1) Abdominal aorta (MC site)
(2) Coronary artery (3) Popliteal artery (4) Internal carotid artery |
|
|
Risk factors for atherosclerosis are divided how?
|
Modifiable and nonmodifiable risk factors.
|
|
|
Modifiable risk factors for atherosclerosis include [...]
|
(1) HTN
(2) Hypercholesterolemia (3) Smoking (4) Diabetes |
|
|
Nonmodifiable risk factors for atherosclerosis?
|
(1) Age
(2) Gender (increased risk in males) (3) Genetics (family history is highly predictive of risk) |
|
|
What is the pathogenesis of atherosclerosis?
|
1. Endothelial cell damage (e.g. HTN, tobacco, homocysteine, ox. LDL)
2. Lipids enter the intima and gets oxidized. 3. Macrophages/lipids adhere to dmged endothelium 4. Macrophages eat ox. LDL and release cytokines that cause hyperplasia of SMC 5. SMC also take up cholesterol. They secrete cytokines that produce ECM (collagen, proteoglycans, elastin) |
|
|
What is a precursor lesion to atherosclerosis?
|
Fatty streak
|
|
|
Fibromuscular cap is due to what?
|
Inflammation and healing with deposition of collagen and proliferation of smooth muscle cells.
|
|
|
What role does atherosclerosis play in disease in the Western world?
|
It accounts for MORE THAN 50% of disease in the Western world
|
|
|
Give some examples of atherosclerosis in different arteries and how they present.
|
(1) Stenosis of e.g. popliteal artery with peripheral vascular disease
(2) Angina (coronary artery) (3) Ischemic bowel disease (mesenteric aa.) |
|
|
You usually don't get symptoms of atherosclerosis until you have more than _____ % of stenosis.
|
70%
|
|
|
Except for stenosis, what is another complication of atherosclerosis?
|
Plaque rupture with thrombosis. This happens at it's "neck". It would expose necrotic lipid core, activating coagulation cascade.
|
|
|
Plaque rupture with thrombosis may result in what?
|
(1) Myocardial infarction (coronary artery)
(2) Stroke (middle cerebral artery) |
|
|
Aside from stenosis and plaque rupture, what is another complication of atherosclerosis?
|
Plaque rupture with embolization (part of plaque embolizes). Results in atherosclerotic embolus.
|
|
|
The hallmark of atherosclerotic emboli is what?
|
Cholesterol clefts in emboli
|
|
|
List the complications of atherosclerosis.
|
(1) Stenosis with ischemia
(2) Plaque rupture with thrombosis (3) Plaque rupture with embolization (4) Weakening of vessel wall |
|
|
Weakening of vessel wall in atherosclerosis results in what? Why?
|
Aneurysm (e.g., abdominal aorta).
Because atherosclerosis represents a diffusion barrier to oxygen. The wall becomes weak (it is dependent on oxygen as everything else). |
|
|
Arteriolosclerosis is what?
|
Narrowing of small arterioles
|
|
|
Arteriolosclerosis is divided into what?
|
(1) Hyaline type
(2) Hyperplastic type |
|
|
What happens in hyaline arteriolosclerosis? How does it look in microscope?
|
Proteins leaking into the wall of the vessel. This produces vascular thickening. Seen as pink hyaline on microscopy.
|
|
|
What people get hyaline arteriolosclerosis?
|
(1) Those with long-standing benign HTN (high bp forces protein into wall)
(2) Diabetics (non-enzymatic glycosylation of basement membrane, this makes it leaky, protein leaks in) |
|
|
What is a consequence of hyaline arteriolosclerosis? (general)
|
Reduced vessel-caliber and end-organ ischemia.
|
|
|
Hyaline arteriolosclerosis classically produces what?
|
Glomerular scarring (arteriolonephrosclerosis). Ischemia will scar glomeruli. This is why patients with DM get chronic renal failure, the glomeruli get scarred.
|
|
|
Hyaline arteriolosclerosis in the kidney may progress to what?
|
Chronic Renal Failure (CRF)
|
|
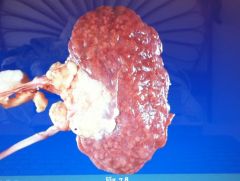
The patient had diabetes. Describe the gross appearance of the organ.
|
We see scarring on the kidney from long-standing hyaline arteriolosclerosis. (arteriolonephrosclerosis)
|
|
|
What does hyperplastic arteriolosclerosis involve?
|
Involves thickening of vessel wall by hyperplasia of smooth muscle.
|
|
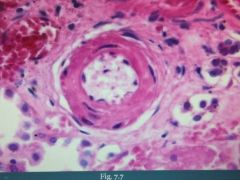
What is this?
|
Hyperplastic arteriolosclerosis. Note the 'onion-skin' appearance.
|
|
|
Hyperplastic arteriolosclerosis is due to what?
|
Malignant hypertension. SMC respond to super high bp by hyperplasia.
|
|
|
What does hyperplastic arteriolosclerosis lead to? (general)
|
Results in reduced vessel caliber with end-organ ischemia.
|
|
|
Malignant HTN may lead to ___________ of the vessel wall.
|
fibrinoid necrosis
|
|
|
Malignant HTN classically causes what?
|
Fibrinoid necrosis with acute renal failure with 'flea-bitten' appearance
|
|
|
Mönckeberg medial calcific sclerosis is _____________ (mildly/non) obstructive.
|
non
|
|
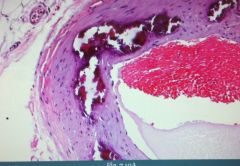
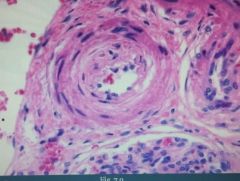
What is this?
|
Mönckeberg medial calcific sclerosis.
|

