![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
125 Cards in this Set
- Front
- Back
|
What is the earliest sign of jaundice? |
Scleral icterus
|
|
|
Jaundice shows up when bilirubin is usually more than _______.
|
2.5 mg/dL
|
|
|
After conjugated bilirubin in bile enters the environment of bacteria in the gut, what happens to the molecule?
|
CB is converted into urobilinogen
|
|
|
What makes stool brown?
|
Urobilin
|
|
|
After urobilinogen has been made in the gut, where does it go?
|
Stool. Some is reabsorbed into the blood and filtered into the kidney making the urine yellow.
|
|
|
These are causes of jaundice and involve the marrow, spleen and macrophages. What are they? What happens?
|
(1) Extravascular hemolysis (excessive of RBCs in reticuloendothelial system)
(2) Ineffective erythropoiesis (death of RBCs in marrow) High levels of UCB overwhelm the conjugating ability of the liver. |
|
|
What color is the urine in extravascular hemolysis and ineffective erythropoiesis? And why?
|
Dark urine.
Large amounts of unconjugated bilirubin gets conjugated and dumped into bile. This means high amounts of urobilinogen that will get reabsorbed, coloring the urine. |
|
|
In extravascular hemolysis or ineffective erythropoiesis there is increased risk for ___________________.
|
pigmented bilirubin gallstones
|
|
|
What is physiologic jaundice of the newborn?
|
Newborn liver has transiently low uridine glucuronidyl transferase activity (UGT). This increases unconjugated bilirubin.
|
|
|
What is kernicterus?
|
A sequence where unconjugated bilirubin deposits in the basal ganglia of babies, leading to neurological deficits and death. Kernicterus is a concern in a child with high UCB.
|
|
|
Treatment of physiologic jaundice of the newborn? How does it work?
|
Phototherapy. Makes UCB water soluble.
|
|
|
What is Gilbert syndrome?
|
Due to mildly low UGT activity; AR. Increased UCB during fasting or stress (e.g., infection) otherwise, not clinically significant.
|
|
|
What is Crigler-Najjar syndrome?
|
Absence of UGT. Increased UCB with kernicterus. Usually fatal.
("Crigler-Najjar sounds like more of a crook than Gilbert ie more severe") |
|
|
What is Dubin-Johnson syndrome?
|
Deficiency of bilirubin canalicular transport protein; AR. Not clinically significant. Increases CB.
|
|
|
A surgeon finds a pitch dark liver in a patient. What is this?
|
Dubin-Johnson syndrome ("Dubious looking liver")
|
|
|
What is Rotor syndrome?
|
Same as Dubin Johnson however the liver is not black.
|
|
|
Biliary tract obstruction is a cause of jaundice. It is associated with what?
|
(1) Gallstones
(2) Pancreatic carcinoma (3) Cholangiocarcinoma (4) Parasites (5) Liver fluke (clonorchis sinensis) |
|
|
Laboratory findings in obstructive jaundice?
|
Elevated CB, decreased urine urobilinogen, increased alkaline phosphatase.
|
|
|
Clinical features of obstructive jaundice?
|
Dark urine (CB) and pale stool. Pruritus due to bile salts in blood. Hypercholesterolemia with xanthomas. Steatorrhea with malabsorption of fat-soluble vitamins (ADEK).
|
|
|
What happens in viral hepatitis? Lab findings? Clinical?
|
Inflammation disrupts hepatocytes and small bile ductules. Increase in both CB and UCB. Dark urine due to increased urine bilirubin; urine urobilinogen is normal or decreased.
|
|
|
Viral hepatitis is inflammation of _____________.
|
liver parenchyma
|
|
|
Viral hepatitis is usually due to?
|
(1) Hepatitis alphabet soup
(2) Other: EBV, CMV |
|
|
Hepatitis virus causes ___________ which may progress to ____________.
|
acute hepatitis; chronic hepatitis
|
|
|
Clinical features of acute hepatitis?
|

(1) Jaundice (mixed CB and UCB)
(2) Dark urine (CB) (3) Fever (4) Malaise (5) Nausea (6) Elevated liver enzymes (ALT more than AST) (7) Symptoms last less than 6 months |
|
|
What is the mechanism of destruction of hepatocytes in acute viral hepatitis?
|
Apoptosis
|
|
|
How is chronic hepatitis defined?
|
(1) Symptoms that last more than 6 months with appropriate serologic markers
|
|
|
In chronic hepatitis there is a risk for progression to what?
|
Cirrhosis
|
|
|
In chronic inflammation the inflammation predominantly involves what?
|
|
|
|
HAV is commonly acquired by __________.
|
travelers
|
|
|
HEV is classically acquired from _____________ or ___________.
|
contaminated water; undercooked seafood
|
|
|
These hepatitis viruses produce acute hepatitis but with no chronic state.
|
Hepatitis A and E
|
|
|
Immunization is only available for hepatitis ______ (A/E) virus.
|
HAV only
|
|
|
In the case of HAV or HEV infection, what antibodies marks active infection and what marks protection against recurrent infections?
|
Anti-virus IgM marks active infection, Anti-virus IgG is protective (indicates prior infection or immunization)
|
|
|
HEV is associated with fulminant hepatitis in one circumstance. What is it?
|
When a pregnant woman gets infected with HEV she can get liver failure with massive liver necrosis.
|
|
|
These viruses are transmitted fecal-orally.
|
Hepatitis A and E virus
(fAEcal transmission) |
|
|
Hepatitis B virus is transmitted ________________.
|
parenterally (IV drug abuse, unprotected intercourse, childbirth.
|
|
|
HBV results in acute hepatitis. Chronic disease occurs in _____% of cases.
|
20%
|
|
|
What is the key marker of infection with HBV?
|
HBsAg
|
|
|
This is the first serologic marker to rise during the acute phase of infection with HBV.
|

HBsAg
|
|
|
When does hepatitis B surface antigen disappear?
|
When the patient resolves the infection
|
|
|
What defines a chronic hepatitis B state?
|
If HBsAg is present for more than 6 months.
|
|
|
The key marker of "acute battle" in hepatitis B infection is what?
|
IgM against the core (for the first 6 months)
("The core is the core of the matter") |
|
|
What is the major antibody our body uses to defeat hepatitis B?
|
IgM (against the core)
|
|
|
Describe the window phase. What is it?
|
A phase that appears after the acute phase when IgM has hammered away at the hepatitis B virus for long enough for it to be eradicated.
Now HBsAg is not present and HBeAg is not present. Virus DNA is also absent. The only thing serologically present is IgM. |
|
|
What antibody is produced during the resolved phase of hepatitis B infection?
|
IgG against the core, however, it is not protective.
|
|
|
What is the "sign of victory" against hepatitis B?
|
IgG against HBsAg
|
|
|
The presence of IgG against HBsAg indicates that ________.
|
YOU HAVE WON THE BATTLE (immunization)
|
|
|
What do we give to immunize people against hepatitis B?
|
HBsAg
|
|
|
What indicates infectivity in a hepatitis B infection?
|
Envelope antigen (HBeAg)
(E for eeeeeeenfectious) |
|
|
Envelope antigen (HBV) is present during what phases?
|
Acute phase and maybe chronic phase.
|
|
|
Transmission of HCV is _________.
|
parenterally (e.g., IVDA, unprotected intercourse, needle stick)
|
|
|
What is the risk for acquiring HCV from blood products?
|
Almost nonexistent due to screening of the blood supply.
|
|
|
True or false: HCV often progresses to chronic disease.
|
True.
|
|
|
What serologic marker will confirm infection with HCV?
|
HCV-RNA
|
|
|
During recovery, what serologic markers will go down (HCV)?
|
RNA. Decreasing RNA indicates recovery.
|
|
|
Persistence of RNA in HCV indicates what?
|
Chronic disease
|
|
|
Hepatitis D is unable to ____________.
|
infect by itself
|
|
|
HDV requires _______ for infection.
|
HBV
|
|
|
HDV can become superinfected after an HBV infection is established, or it can co-infect with HBV, what is worse?
|
Superinfection
("Super bad") |
|
|
What is cirrhosis?
|

End-stage liver damage characterized by disruption of normal hepatic parenchyma by bands of fibrosis and regenerative nodules of hepatocytes.
Surface of the liver should be totally smooth. |
|
|
What is the hallmark of cirrhosis?
|
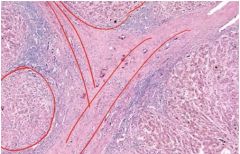
Bands of fibrosis separating regenerating nodules of hepatocytes.
|
|
|
What mediates fibrosis in cirrhosis? How?
|
Fibrosis is mediated by TGF-beta from stellate cells.
|
|
|
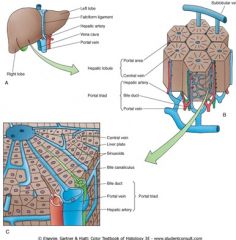
Where are stellate cells located?
|
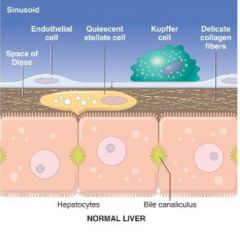
They lie beneath the endothelial cells that line the sinusoids.
|
|
|
One category of findings in the end-stage liver damage in cirrhosis is portal HTN. What clinical findings based on this could you observe?
|
(1) Ascites (fluid in peritoneal cavity)
(2) Congestive splenomegaly/hypersplenism (when it consumes PLTs) (3) Portosystemic shunts - Esophageal varices - Hemorrhoids - Caput medusae (4) Hepatorenal syndrome - Rapidly developing renal failure in the context of cirrhosis. |
|
|
Loss of liver function leads to loss of the ability to ___________ . List some clinical features of this.
|
detoxify
(1) Mental status changes, asterixis, coma - Due to increased ammonia (2) Gynecomastia (liver plays important role in removing estrogen from the blood), spider angiomata, palmar erythema (3) Jaundice |
|
|
Describe manifestations of decreased protein synthesis (which would occur in cirrhosis).
|
(1) Hypoalbuminemia
- Edema (2) Coagulopathy - Can't activate vitamin K through epoxide reductase, can't produce coagulation factors |
|
|
In cirrhosis, what would rise, PT or PTT?
|
Both, however the PT is used to follow the degree of deficiency. This is same as for warfarin therapy, which affects epoxide reductase.
|
|
|
__________-related liver disease can lead to cirrhosis.
|
Alcohol
|
|
|
A man with cirrhosis has a putrid breath. What is the cause?
|
This is fetor hepaticus. Shunting allows thiols from portal blood (from the gut) to go directly to the lungs.
|
|
|
What is alcohol-related liver disease?
|
Damage to hepatic parenchyma due to consumption of alcohol.
|
|
|
This is the MCC of liver disease in the West.
|
Alcohol
|
|
|
Alcohol-related liver disease can present with three patterns of injury, what are they?
|
(1) Fatty liver
(2) Alcoholic hepatitis (3) Cirrhosis |
|
|
What is fatty liver? What is the result?
|
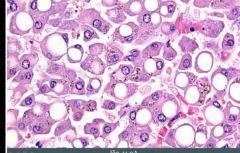
Accumulation of fat in hepatocytes (due to alcohol). Result is a heavy, greasy liver; resolves with abstinence.
|
|
|
What is alcoholic hepatitis? What mediates the damage?
|
Direct chemical injury to hepatocytes; generally seen with binge drinking (fyllefest). Acetylaldehyde mediates the damage.
|
|
|
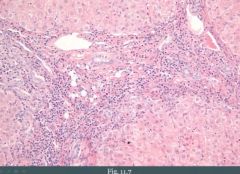
Key finding(s) in alcoholic hepatitis include?
|
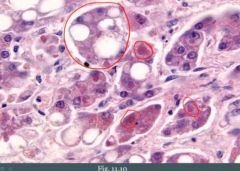
(1) Swelling or ballooning of hepatocytes with necrosis and inflammation
(2) Mallory bodies (red encircled) |
|
|
What are mallory bodies?
|
Damaged intermediary filaments within hepatocytes (alcoholic hepatitis)
|
|
|
Presentation of alcoholic hepatitis?
|
(1) Painful hepatomegaly and elevated liver enzymes (AST > ALT)
(2) May result in death ("toAST with alcohol") |
|
|
Alcohol damages what intracellular organelle? This leads to a preferential increase in what serum marker?
|
Mitochondria.
AST. |
|
|
Cirrhosis is a complication of _________________________. How many alcoholics get this complication?
|
chronic alcohol-induced liver damage
Seen in about 10-20% of alcoholics. |
|
|
What is Nonalcoholic Fatty Liver Disease?
|
Fatty change, hepatitis and/or cirrhosis. Develops without exposure to alcohol or other known insult.
|
|
|
Nonalcoholic fatty liver is associated with?
|
Obesity
|
|
|
Nonalcoholic fatty liver disease is a diagnosis of __________.
|
exclusion (you start by making the assumption that the patient is abusing alcohol until proven otherwise)
|
|
|
In nonalcoholic fatty liver disease the __________ (AST/ALT) will be greater than the ___________(AST/ALT).
|
ALT > AST (alcohol not involved)
|
|
|
What is hemochromatosis? What mediates the damage?
|
Excess body iron that deposits in tissues and damages organs. Damage is mediated by generation of free radicals (fenton rxn).
|
|
|
Deposition of iron in tissues is called _____________ (hemosiderosis/hemochromatosis).
|
hemosiderosis. When it causes damage we call it hemochromatosis.
|
|
|
Hemochromatosis can be divided into [...]
|
(1) Primary
(2) Secondary |
|
|
What is primary hemochromatosis due to?
|
Mutations in the HFE gene, most commonly a C282Y mutation (All iron that is absorbed enters the blood)
|
|
|
Secondary hemochromatosis can arise as a complication of?
|
Transfusions
|
|
|
When does hemochromatosis typically present?
|
Late adulthood. Takes time for it to build up.
|
|
|
Classic findings in hemochromatosis?
|
(1) Cirrhosis
(2) Secondary diabetes ("Bronze diabetes") (3) Bronze skin (4) Cardiac arrhythmia (5) Gonadal dysfunction (testicular atrophy) |
|
|
Lab findings in hemochromatosis?
|
Based on an iron overloaded state:
(1) Increased ferritin with decreased TIBC (2) Increased serum iron (3) High percent saturation |
|
|
When you suspect hemochromatosis you perform a _______.
|
biopsy (usually liver)
|
|
|
What do you see on biopsy of a liver affected by hemochromatosis?
|
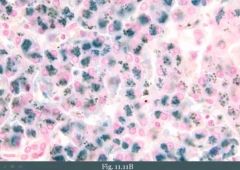
(1) Brown pigment in hepatocytes
We distinguish it from lipofuscin by staining with Prussian blue which stains iron blue. |
|
|
What is lipofuscin?
|
Wear and tear pigment derived from breakdown of peroxidized lipids. Piles up in the lysosomes. Sign of aging.
"The grey hair of the cells" |
|
|
How could you treat patients with hemochromatosis?
|
Phlebotomy
|
|
|
In hemochromatosis there is an increased risk for _______________ in the liver.
|
hepatocellular carcinoma
|
|
|
What is Wilson's disease? (brief, leave out pathogenesis)
|
AR defect (ATP7B gene) in ATP-mediated hepatocyte copper transport. Can lead to cirrhosis. Results in lack of copper transport into bile and lack of copper incorporation into ceruloplasmin.
|
|
|
Describe the pathogenesis of Wilson's disease.
|
Copper builds up in the hepatocytes, leaks into serum and deposits in tissues. Copper-mediated production of hydroxyl radicals lead to tissue damage.
|
|
|
When does Wilson's disease present? How does it present?
|
Childhood.
(1) Cirrhosis (2) Neurologic manifestations (asterixis; liver flap, behavioral changes, dementia, chorea) (3) Kayser-Fleischer ring in cornea (4) Risk for hepatocellular carcinoma |
|
|
A child with parkinson like symptoms (or huntington's disease) what would you think about?
|
Wilson's disease.
|
|
|
Treatment of Wilson's disease?
|
D-penicillamine
|
|
|
Laboratory findings in Wilson's disease?
|
(1) Increased urinary copper
(2) Decreased serum ceruloplasmin - We don't have the ability to load ceruloplasmin with copper, so we won't have too much ceruloplasmin floating in the blood. (3) Increased copper on liver biopsy |
|
|
What is primary biliary cirrhosis? (brief)
|
Autoimmune granulomatous destruction of intrahepatic bile ducts. Etiology unknown, however Anti-mitochondrial antibody is present.
|
|
|
Primary biliary cirrhosis classically arises in?
|
Classically arises in women (average age 40)
|
|
|
Primary biliary cirrhosis is associated with other _____________.
|
autoimmune diseases
|
|
|
How do patients with primary biliary cirrhosis present?
|
With obstructive jaundice.
Cirrhosis is a late complication. |
|
|
What is primary sclerosing cholangitis?
|
Inflammation and fibrosis of intrahepatic and extrahepatic bile ducts.
|
|
|
What does primary sclerosing cholangitis result in which you could observe on microscopy?
|
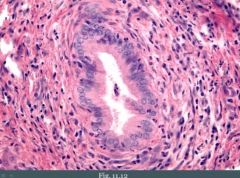
Periductal fibrosis (hence sclerosing) with an 'onion-skin' appearance. Also we could see a 'string-of-pearl'. This is because uninvolved regions of the bile ducts become dilated.
|
|
|
What is the etiology of primary sclerosing cholangitis?
|
Etiology is unknown, however a p-ANCA is often positive.
|
|
|
Primary sclerosing cholangitis is associated with what?
|
Ulcerative colitis
|
|
|
Patients with primary sclerosing cholangitis presents how?
|
With obstructive jaundice.
Cirrhosis is a late complication. There is an increased risk for hepatocellular carcinoma. |
|
|
What is Reye syndrome?
|
Fulminant liver failure and encephalopathy in children with viral illness who take aspirin. Likely related to mitochondrial damage of hepatocytes.
|
|
|
How do patients with Reye syndrome present?
|
(1) Hypoglycemia
(2) Markedly elevated liver enzymes (3) Nausea with vomiting Can progress to coma and death. |
|
|
What is a hepatic adenoma? What is it associated with?
|
Benign tumor of hepatocytes. Associated with oral contraceptive use and it regresses upon cessation. Also associated with use of testosterone.
|
|
|
Complications of a hepatic adenoma?
|
(1) Risk of rupture and intraperitoneal hemorrhage, especially during pregnancy.
|
|
|
Why is there a risk of rupture of hepatic adenomas?
|
Because they are sub-capsular.
|
|
|
Risk factors for hepatocellular carcinoma?
|
(1) Cirrhosis
(2) Chronic hepatitis (3) Aflatoxins derived from Aspergillus |
|
|
Aflatoxins induce what in hepatocytes?
|
p53 mutations
|
|
|
There is a similarity between hepatocellular carcinoma and renal carcinoma. What is it?
|
They both love to invade veins. Hepatocellular carcinoma often invades the hepatic vein, which can lead to Budd-Chiari syndrome (liver infarction secondary to obstruction of this vein).
|
|
|
How does Budd-Chiari syndrome present?
|
Presents with painful hepatomegaly and ascites.
|
|
|
Prognosis of hepatocellular carcinoma? Why?
|
Poor, because they are often detected late because symptoms are often masked by cirrhosis.
|
|
|
This is a useful serum tumor marker for hepatocellular carcinoma.
|
Alpha-fetoprotein
|
|
|
What is more common in the liver, metastasis or primary liver tumors?
|
Metastasis
|
|
|
What are the most common sources of metastasis to the liver?
|
(1) Colon carcinoma
(2) Pancreatic carcinoma (3) Lung & breast |
|
|
What would you see on physical exam of a patient with metastasis to the liver?
|
Metastasis results in multiple nodules in the liver. Clinically this may be detected as hepatomegaly with nodular free edge of the liver (bumps are felt).
|

