![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
65 Cards in this Set
- Front
- Back
|
Cerebrovascular Disease is what rank in the cause of death in the US?
|
#3
|
|
|
What are the 2 major types of Cerebrovascular Accidents ("stroke")? Which type is more common in the US?
|
1. Deprivation of blood &/or oxygen = infarct
-Thrombosis -Embolism 2. Hemorrhage **Infarcts more common in US |
|
|
After how long of a total loss of oxygen are there irreversible cell changes in the brain?
|
5-6 minutes
**there is selective vulnerability of neurons |
|
|
What are the 2 patterns of Hypoxic-Ischemic injury?
|
1. Global ischemia
2. Focal ischemia |
|
|
Give 5 examples of things that can cause Global Ischemia
|
1. Cardiac arrest
2. Hypotension 3. Suffocation 4. Atmospheric 5. Poisoning |
|
|
What is the severe manifestation of Global Ischemia?
|
Persistent Vegetative State
|
|
|
What is the pathology seen in the Brain after Global Ischemia?
|
1. Diffuse softening
2. Slow autolysis |
|
|
What parts of the adult brain are comparatively vulnerable to hypoxic/ischemic injuries?
|

1. Cerebral Cortex
2. Hippocampus 3. Purkinje cell layer in the Cerebellum |
|
|
Define Watershed areas
|

Territories of the brain where 2 blood supplies meet & the blood supply from the 2 vessels does not overlap
|
|
|
Define Watershed areas
|

Territories of the brain where 2 blood supplies meet & the blood supply from the 2 vessels does not overlap
|
|

-
|

-
|
|

What is this picture showing?
|
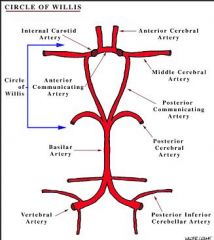
Watershed area between the Anterior Cerebral Artery (ACA) & the Middle Cerebral Artery (MCA)
|
|
|
What are the causes of Focal Ischemia?
|
Occlusions of vessel
1. In situ Thrombosis 2. Vasculitis 3. Hypercoagulable state 4. Arterial dissection 5. CADASIL = Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts & Leukoencephalopathy Embolism |
|
|
What is the most common cause of In situ Thrombosis?
|
Atherosclerosis
|
|
|
What are the most common sites of Atherosclerosis
|

1. Thrombosis of Carotid Bifurcation
2. Middle Cerebral Artery 3. Top & bottom of Basilar Artery |
|
|
Where would an infarct occur producing Focal Ischemia in a Hypercoagulable state?
|
Venous infarction
|
|
|
What are the sources of Emboli in Focal Ischemia?
|
1. Heart
-Mural thrombus post-MI -Heart valves -Atrial Fibrillation 2. Carotid arteries or Aorta 3. Paradoxical via Patent Foramen Ovale 4. Fat, tumor, air |
|
|
What is the #1 general site for emboli to lodge?
|
Middle Cerebral Artery
**generally lodge in branchpoints or stenotic foci |
|
|
What are the gross appearances of Infarcts:
1. 0-6 hours 2. 48 hours 3. 2-10 days 4. 10-21 days |
0-6 hrs = no gross changes
48 hrs = pale, soft, swollen, indistinct gray-white border 2-10 days = friable, demarcation of injury 10-21 days = liquefaction |
|
|
What are the Acute (12-24 hrs) Microscopic changes seen in Ischemic Injury?
|
1. Red neurons
2. Microvacuolization 3. Nuclear Pyknosis = condensation and reduction in the size of a cell or cell nucleus |
|
|
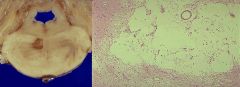
Acute Ischemic injury of Purkinje cells in Cerebellum
1. red neurons 2. have lost nucleoli 3. cells are shrinking |
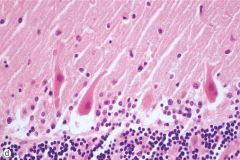
What is this picture showing?
|
|
|
What are the Subacute (24 hrs - 2 wks) Microscopic changes seen in Ischemic injury?
|
1. Necrosis
2. Macrophages 3. Vascular proliferation 4. Gliosis |
|
|
After how long does the Repair phase occur in Ischemic Injury?
|
> 2 wks
|
|
|
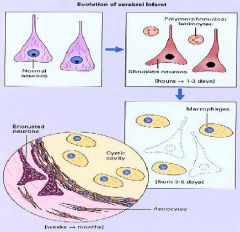
End-result of a Focal Infarct
|
What is this picture showing?
|
|
|
What is a Pale infarct?
|
Usually due to a platelet thrombus that develops over a disrupted plaque
Infarct in which little or no bleeding into tissue spaces occurs when the blood supply is obstructed Treat with Anticoagulation |
|
|
What are Hemorrhagic Infarcts? What are they usually the consequence of?
|
An infarct that is red because of the infiltration of blood from collateral vessels into the necrotic area
Embolism |
|
|
Which type of infarct do you want to avoid Anticoagulatives as a treatment - Pale or Hemorrhagic?
|
Hemorrhagic
|
|
|
Hemorrhagic infarct
-arrow denotes an occluded vessel in the MCA distribution -Petechial hemorrhages |

What is seen here?
|
|
|
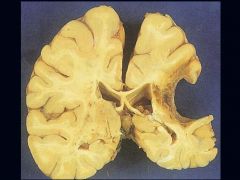
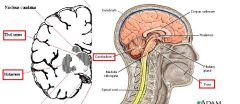
Lacunar Infarct
-most commonly due to HTN or Diabetes -cystic areas of microinfarction <15 mm in diameter -caused by Hyaline Arteriosclerosis |

What is seen here?
|
|
|
What are Lacunar Infarcts? What are they due to?
|
Cystic areas of microinfarction less than 15 mm in diameter
Hyaline Arteriosclerosis due to: -HTN (most common) -Diabetes **pic is Lacunar Infarct of Pons |
|
|
What are 4 consequences of Infarcts?
|
1. Destruction of vital areas
2. Massive edema & death 3. Permanent neurological deficits 4. Multiple small infarcts may lead to dementia |
|
|
What are the 4 locations of Hemorrhage?
|
1. Intraparenchymal
2. Subarachnoid 3. Subdural 4. Epidural |
|
|
What is the #1 cause of Intraparenchymal Hemorrhage? What is the pathogenesis?
|
Hypertension
Acclerated atherosclerosis -> increased fragility -> Charcot-Bouchard aneurysms -> necrosis |
|
|
Hypertensive Hemorrhages
|

What is shown here?
|
|
|
What are the most common sites of Intraparenchymal Hemorrhage?
|
1. Putamen
2. Thalamus 3. Pons 4. Cerebellum 5. others |
|
|
What is a Subarachnoid Hemorrhage? What is the most frequent cause?
|
Bleeding between the pia mater and the arachnoid of the brain
Berry Aneurysm rupture *can also be due to: -extension into ventricular system -vascular malformation -coagulopathy -tumors |
|
|
Subarachnoid Hemorrhage
-there is no Dura on the brain -blood is directly on the surface of the brain |
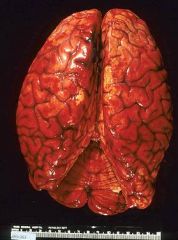
What is seen here?
|
|
|
What disorders have increased #'s of Berry Aneurysms?
|
1. AD Polycystic Kidney Disease
2. NF1 3. Marfan Syndrome 4. Ehlers-Danlos, IV 5. Fibromuscular Dysplasia of Extracranial Arteries |
|
|
What are the risk factors for Berry Aneurysm?
|
Smoking & HTN
|
|
|
What is the pathology of Berry Aneurysms?
|
Thin walled outpouching at arterial branchpoints
Neck portion is devoid of muscle or elastica |
|
|
What is the most common location for Berry Aneurysms to occur?
|
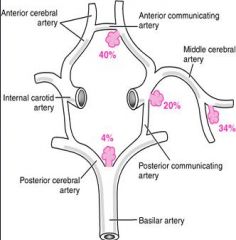
Anterior circulation is most common
|
|
|
Berry Aneurysm
|

What is seen here?
|
|
|
What factors increase the likelihood of rupture of Berry Aneurysms?
|
1. size > 10 mm
2. 5th decade of life 3. Women gender 4. increased intracranial pressure |
|
|
What is the clinical manifestation of Berry Aneurysm rupture?
|
1. Sudden onset of severe Occipital headache
2. decribed as "worst headache of my life" |
|
|
What % of people die after their 1st bleed from Berry Aneurysm rupture?
|
25-50%
|
|
|
What are the early complications of Berry Aneurysm rupture? Late?
|
Early = Vasospasm
Late = Meningeal scarring -> hydrocephalus |
|
|
What is an Epidural Hemorrhage?
|
Hemorrhaging from the Middle Meningeal Artery leading to a hematoma in the virtual space b/w the inner aspect of the Cranial bones & the Dura Mater
|
|
|
Temporoparietal skull fracture + tear of the Middle Meningeal Artery
|
Epidural Hemorrhage
|
|
|
Which hemorrhage is a neurological emergency, Epidural or Subdural? Why?
|
Epidural b/c the Middle Meningeal Artery has been torn & is under arterial pressure so the hematoma progresses quickly
|
|
|
Left = Epidural Hematoma
Right = Subdural Hematoma |
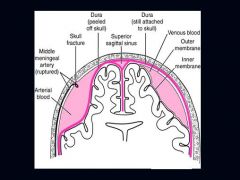
What is seen on the Left? Right?
|
|
|
Epidural Hematoma
Fracture of Temporalparietal skull Middle Meningeal Artery |

What is seen here?
What is the cause? What has ruptured? |
|
|
What is the cause of a Subdural Hematoma?
|
Tearing of "bridging veins" that connect Superficial Cerebral Veins & the Dural Venous Sinuses
|
|
|
What are the manifestations of Subdural Hematomas?
|
Focal, nonfocal, headache, confusion, usually slower in progression than Epidural
Surgical drainage, if needed Usually due to blunt head injuries -car accident -baseball bat |
|
|
What are predisposing factors for Subdural Hematomas?
|
1. Brain atrophy
2. Shaking 3. Whiplash |
|
|
In what people are Subdural Hematomas commonly seen in?
|
1. Blunt trauma
2. Elderly people, especially those who are hospitalized or stay in nursing homes & often fall out of bed 3. Boxers 4. Shaken baby |
|
|
Subdural Hematoma
|

What is seen here?
|
|
|
What are some "other" causes of Hemorrhage?
|
1. Blood dyscrasias
2. Fat emboli 3. Amyloid angiopathy 4. Vascular malformations |
|
|
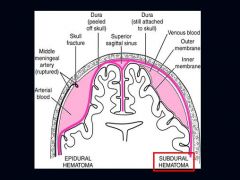
Amyloid Angiopathy
Hemorrhage b/c vessels get brittle |
What is seen here? What could it lead to?
|
|
|
What is Arteriovenous Malformation?
|
Defective malformation of capillaries in a normal part of the brain
-arterial blood enters directly into the veins, usually by way of arteriovenous anastomoses that form at the defective site |
|
|
What gender is more susceptible to Arteriovenous Malformations? What are the complications? Where do they most commonly occur?
|
1. Men
2. Seizures & hemorrhage 3. MCA territory |
|
|
What do Arteriovenous Malformations look like?
|

Tangle of torturous vessels with blood vessels separated by Gliotic brain
|
|
|
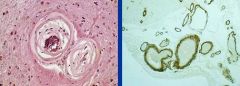
Arteriovenous Malformation
-tortuous arteries & veins which form cortical-subcortical networks of "worm-like" ateriovenous shunts embedded in hemosiderin laden glial tissue |
What is seen here?
|
|
|
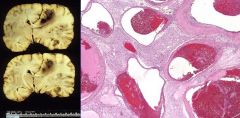
Vascular Malformation characterized by back-to-back hyalinized vessels with foci of hemosiderin
|
Cavernous Angioma
|
|
|
Vascular Malformation characterized by dilated thin-walled vessels separated by normal brain. Most commonly occur in the Pons
|
Capillary Telangiectasia
|
|
|
Where do Capillary Telangiectasia's most commonly occur?
|
Pons
|

