![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
What is the normal location of the Pituitary Gland?
|
within the Sella Turcica, a concavity of the Sphenoid Bone, whoch forms part of the base of the skull
|
|
|
Which part of the Pituitary is the "producer"? "Storehouse"?
|
Producer = Anterior
Storehouse = Posterior |
|
Label
|
-
|
|
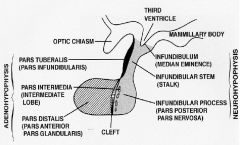
Label
|
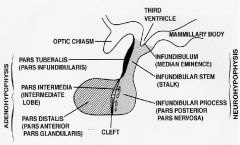
-
|
|
|
What part of the Pituitary is connected to the Infundibulum (Median Eminence) via a stalk?
|
Posterior Pituitary
|
|
|
Explain why the Posterior Lobe is considered a "storehouse"
|
Hormones are made in the Hypothalamus & travel down to the Posterior Pituitary via axons & are stored until released
|
|
|
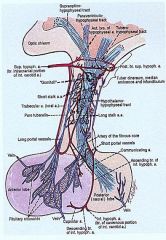
Describe the circulation of the Posterior Lobe
|
receives circulation via an Artery & has direct release of hormones into a Vein
|
|
|
Describe the circulation of the Anterior Pituitary
|
receives blood from the Portal Venous System
|
|
|
If blood supply to the Pituitary is compromised, which lobe gets hit the hardest? Why?
|
Anterior b/c it receives venous blood
|
|
|
What anatomical structures are in proximity to the Pituitary?
|
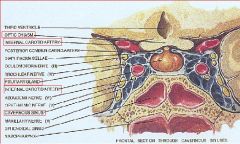
1. Optic Chiasm
2. Hypothalamus 3. Internal Carotid Arteries (Cavernous Sinus) 4. Sphenoid Sinus |
|
|
What happens if the Pituitary compresses the central portion of the optic chiasm?
|

Bitemporal Hemianopsia
|
|
|
What may happen if a Pituitary Tumor compresses the 3rd Ventricle?
|
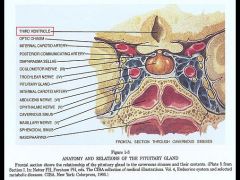
Hydrocephalus
|
|
|
What may happen if a Pituitary Tumor compresses the Cavernous Sinus?
|
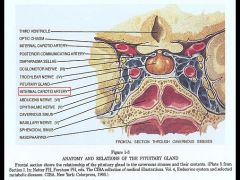
Internal Carotid Artery compression
|
|
|
What is the embryological origin of the Anterior Lobe?
|
Oral Ectoderm (Stomodeum) -> Rathke's Pouch -> Anterior lobe
|
|
|
What is the embryological origin of the Posterior Lobe?
|
Neuroectoderm (Diencephalon)
|
|
|
During what embryological time period does the Pituitary begin to form?
|
3-8 weeks
|
|
|
Describe the embryological formation of the Pituitary
|
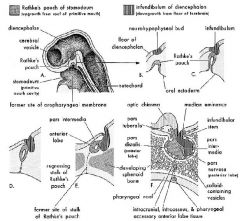
At about 3-5 weeks, Rathke's Pouch buds upwards into the cranial cavity
At the same time Neuroectoderm is coming down from the floor of the Diencephalon (developing Hypothalamus) to meet the tissue of Rathke's Pouch |
|
|
From what Hypothalamic nucleus is Vasopressin (ADH) synthesized?
Oxytocin? |
ADH = Supraoptic
Oxytocin = Paraventricular |
|
|
List the 7 hormones released from the Anterior Pituitary & also name the stimulators for each
|
1. TSH <- TRH
2. LH <- GnRH, Estrogen 3. FSH <- GnRH, Estrogen 4. ACTH <- CRF 5. MSH <- CRF 6. GH <- GHRH 7. Prolactin <- TRH |
|
|
What does the histology of the Posterior Pituitary contain?
|
1. Glia = Pituicytes
2. Axons from Hypothalamus (Herring bodies = nerve terminals from which ADH & Oxytocin are released) |
|
|
What are the 5 cell types in the Anterior Lobe?
|
1. Somatotrophs GH
2. Lactotrophs = Prolactin 3. Corticotrophs = ACTH, POMC, MSH 4. Thyrotrophs = TSH 5. Gonadotrophs = FSH & LH |
|
|
T or F: The majority of Pituitary tumors are associated with the MEN type 1 symdrome
|
False = most are sporadic
|
|
|
What is the most common tumor type of the Pituitary?
|
Adenoma = benign & most are composed of a single cell type & secrete only 1 hormone
|
|
|
What is the gross pathology associated with Pituitary Adenomas?
|
1. Soft, well circumscribed
2. possible compression of adjacent structures 3. possible local invasion 4. Pituitary Apoplexy = bleeding within the gland |
|
|
What is the microscopic pathology seen in Pituitary Adenomas?
|
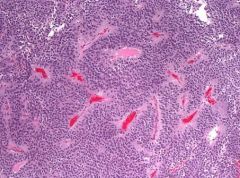
1. Sheets of Monotonous cells
2. sparse intervening Connective Tissue |
|
|
What is the #1 type of Hyperfunctioning Pituitary Adenoma & accounts for 30% of Adenomas?
|
Prolactinoma
|
|
|
What are the main clinical features of Prolactinomas?
|
Female of reproductive age = Amenorrhea & Galactorrhea
Men = loss of libido & infertility |
|
|
Why do Prolactinomas cause Amenorrhea in women?
|
Prolactin inhibits GnRH release -> decreased LH & FSH
|
|
|
In what people are Prolactinoma's more easily diagnosed?
|
women age 20-40
|
|
|
What are the lab findings associated with Prolactinoma's
|
1. increased Prolactin
2. decreased FSH & LH due to feedback inhibition by Prolactin on GnRH |
|
|
In what people are Prolactinoma's usually larger?
|
Older age = post-menopausal women don't notice amenorrhea
|
|
|
What is the treatment for Prolactinoma's?
|
Bromocriptine & Cabergoline = Dopamine agonists
**Dopamine from Hypothalamus inhibits Prolactin secretion from Anterior Pituitary |
|
|
2nd most common Pituitary Adenoma with Hyperfunction
|
Growth Hormone Adenoma
|
|
|
What gene do 40% of Growth Hormone Adenoma's express?
|
gsp oncogene (GTPase deficiency)
|
|
|
What is the treatment for Growth Hormone Adenomas?
|
Octreotide = mimics Somatostatin to inhibit GH secretion
|
|
|
What are the clinical manifestations of Growth Hormone Adenoma's?
|
1. Children = gigantism
2. Adults = Acromegaly |
|
|
What are 2 pharmacologic agents that interfere with Dopamine secretion & could mimic a Prolactinoma?
|
Methyl-dopa = increased alpha-2 receptor-mediated inhibition of SNS
Reserpine = blocks the storage of NE & Dopamine in secretory vesicles |
|
|
What are the clinical features of Gigantism?
|
Tall stature & long extremities due to the fact that Epiphyseal Plates have not closed yet
|
|
|
What are the clinical features of Acromegaly?
|
-Prominent Jaw
-Flat, broad forehead -Enlarged hands & feet **Epiphyseal plates have closed = increased LATERAL bone growth but not linear |
|
|
What are associated findings in Growth Hormone Adenoma's?
|
1. Diabetes Mellitus = GH stimulates gluconeogenesis
2. Muscle weakness 3. Hypertension 4. Congestive Heart Failure 5. Organomegaly |
|
|
What do Corticotroph Adenoma's cause?
|
Cushing Disease due to excess ACTH secretion resulting in Hypercortisolism
|
|
|
Describe Nelson Syndrome
|
-Bilateral adrenalectomy causes enlargement of a preexisting Pituitary Adenoma due to lack of Cortisol negative feedback on ACTH
-Hyperpigmentation due to MSH excess |
|
|
Name for nonfunctional Adenomas but may cause mass effects
|
Null Cell Adenoma
|
|
|
How do Gonadotroph Adenoma's present clinically?
|
Usually do NOT produce distinct clinical syndromes & are usually diagnosed only after they have attained a size that will cause a mass effect
Menstrual abnormalities, infertility & various nonspecific hormonal changes are found in some patients |
|
|
Discuss Pituitary Carcinoma's
|
-Rare
-Nonfunctional -requires demonstration of metastases to distant sites = lymph nodes, bone, liver |
|
|
What percent of the Pituitary has to be lost before Hypopituitarism is encountered?
|
75% loss
|
|
|
What are 3 etiologies of Hypopituitarism?
|
1. tumors
2. ischemic necrosis 3. Empty Sella Syndrome |
|
|
Discuss a Rathke Cleft Cyst
|
Benign cyst that forms in the stalk or Anterior Lobe
- as it enlarges it can compress the normal gland & lead to hypopituitarism |
|
|
List 4 Sellar Tumors that may cause Hypopituitarism
|
1. Adenomas
2. Carcinomas 3. Metastases 4. Rathke Cleft Cyst |
|
|
List 3 Suprasellar tumors that may cause Hypopituitarism
|
1. Gliomas
2. Germinomas 3. Craniopharyngiomas |
|
|
Most common intracranial germ cell tumor
|
Germinoma
|
|
|
1. What is the location of Germinoma's?
2. What is the histology of Germinoma's? 3. Who are most often affected? 4. What lab findings are associated? |
1. Midline, suprasellar, or pineal
2. Germ cells + T cells 3. Japanese men 4. AFP, bHCG, CEA |
|
|
What is a Craniopharyngioma?
|
Benign pituitary tumor derived from Rathke's Pouch remnants
|
|
|
What is the most common cause of Hypopituitarism in children?
|
Craniopharyngioma
|
|
|
How are Craniopharyngiomas manifested in children? Adults?
|
Children = endocrine abnormalities
Adults = visual abnormalities |
|
|
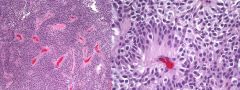
What are the 2 histological variants of Craniopharyngioma?
|
1. Adamantinomatous
2. Papillary |
|
|
Describe the histology of Adamantinomatous Craniopharyngioma's
|
-Stratified squamous epithelium
-Wet keratin -Calcifications -Cholesterol-rich fluid cyst ("motor oil") -Chronic inflammation -fingers extend into adjacent brain |
|
|
Describe Sheehan Syndrome
|
Postpartum Pituitary Necrosis
-massive blood loss at time of delivery causes hypoperfusion of the pituitary that has undergone physiological hyperplasia during pregnancy |
|
|
What conditions could cause Ichemic Necrosis of the Pituitary resulting in Hypopituitarism?
|
1. DIC
2. Sicke cell anemia 3. trauma 4. shock of any origin |
|
|
What is the pathology seen in Ischemic necrosis of the Pituitary?
|
Grossly atrophic = <0.1 gm
Fibrous Scar tissue |
|
|
What is the most common cause of Empty Sella Syndrome?
|
Diaphragmatic hernia
|
|
|
Describe Primary Empty Sella Syndrome
|
Pituitary atrophy is related to a compression by the CSF & Arachnoidea that invaginate into the Sella through a defect in the diaphragm
|
|
|
What are 3 "other" causes of Empty Sella Syndrome?
|
1. Sheehan's syndrome
2. Infarction of adenoma 3. Sellar mass treated by surgery/radiation |
|
|
Describe the mnemonic for the most common causes of Hypopituitarism
|
Invasion by tumors
Injury = head trauma Infarction = postpartum Sheehan syndrome Irradiation Immune diseases = Sarcoidosis; Autoimmune Hypophysitis Infection = basal meningitis, TB Inborn errors of metabolism Idiopathic |
|
|
What congenital defect causes Hypopituitarism from patients not being able to make pituitary hormones?
|
defect in Transcription Factor Pit-1 gene
-defective protein binds DNA but does not activate target genes |
|
|
Invasive Pituitary Adenoma
-patient had 2-year history of dementia & visual impairment |
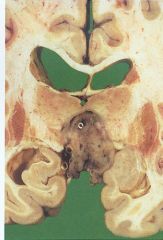
What is seen here?
|
|
|
Pituitary Adenoma
|
What is seen here?
|
|
|
Pituitary Adenoma
|
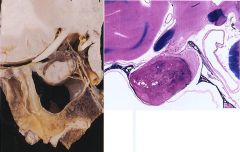
What is seen here?
|
|
|
Rathke Cleft Cyst = benign cyst that forms in the stalk or Anterior lobe
|

What is seen here?
|
|
|
Germinoma = suprasellar tumor
|

What is seen here?
|
|
|
Craniopharyngioma = mass of cysts & solid areas
|

What is seen here?
|
|
|
Adamantinomatous Craniopharyngioma
|
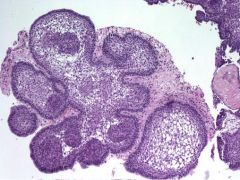
What is seen here?
|
|
|
Papillary Craniopharyngioma
|
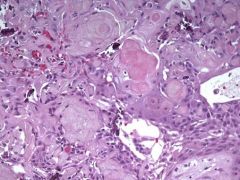
What is seen here?
|
|
|
Empty Sella Syndrome, primary type
|

What is seen here?
|
|
|
Pituitary Apoplexy
|

What is seen here?
|

