![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
List the Hereditary & Congenital Hyperbilirubinemias that have UNCONJUGATED Bilirubin
|
1. Hemolytic anemia
2. Gilbert Syndrome 3. Crigler-Najjar Syndrome 4. Physiologic jaundice of neonates |
|
|
Hereditary & Congenital Hyperbilirubinemias that have CONJUGATED Hyperbilirubinemias
|
1. Dubin-Johnson Syndrome
2. Rotor Syndrome 3. Biliary obstruction: atresia, cysts, AAT deficiency |
|
|
What is the cause of Gilbert Syndrome?
|
Autosomal Dominant condition in which there is a mutation in the gene encoding UDP-glucuronyl transferase (UGT) activity along with decreased bilirubin uptake
-results in decreased UGT activity and a resultant Unconjugated Hyperbilirubinemia |
|
|
Syndrome that is associated with jaundice that appears with minor stress, exercise, or fasting; usually asymptomatic & no treatment is required
|
Gilbert Syndrome = decreased UGT activity & decreased Bilirubin uptake by Liver
|
|
|
What is the ONLY Hereditary Hyperbilirubinemia that causes Liver changes
|
Dubin-Johnson Syndrome -> Black Liver
|
|
|
Describe Crigler-Najjar Syndrome Type 1
|
Autosomal recessive condition resulting in absent UGT activity & Unconjugated Hyperbilirubinemia
-early death from Kernicterus, damage to the Basal Ganglia |
|
|
Describe Crigler-Najjar Syndrome Type 2
What is the treatment? |
AUtosomal dominant condition resulting in decreased UGT activity & Unconjugated Bilirubinemia
-milder than Type 1; jaundice Phenobarbitol |
|
|
Explain Physiologic Jaundice of Neonates
|
Transient Unconjugated Hyperbilirubinemia due to immaturity of the liver
-due to increased Bilirubin production & a relative deficiency of Glucuronyl Transferase in the immature liver |
|
|
What is the cause of Dubin-Johnson Syndrome?
|
Autosomal recessive condition resulting from defective bilirubin TRANSPORT protein out of the liver
|
|
|
What are the clinical manifestations of Dubin-Johnson Syndrome?
|
1. Intermittent Jaundice
2. RUQ & epigastric pain 3. CONJUGATED HYPERBILIRUBINEMIA 4. mildly elevated LFT's 5. BLACK LIVER |
|
|
Conjugated Hyperbilirubinemia + Black Liver
|
Dubin-Johnson Syndrome
|
|
|
Syndrome that is similar to Dubin-Johnson Syndrome but abnormal black pigment is not present
|
Rotor Syndrome
|
|
|
Dubin-Johnson Syndrome = causes Black Liver
|
What Hereditary Hyperbilirubinemia caused this?
|
|
|
After what % of Liver functional capacity is lost do symptoms of Hepatic Failure appear?
|
80-90%
|
|
|
What is the difference between Acute & Chronic Liver Failure?
|
Acute = sudden onset that may cause death in a few days or weeks; associated with massive hepatic necrosis following viral infection, adverse drug reaction, or ingestion of toxins
Chronic = develops over a period of years & is typically associated with Cirrhosis |
|
|
Describe "Hepatorenal Syndrome"
|
-sudden functional renal failure (w/out underlying kidney disease) in a patient with end-stage liver failure
-renal failure is caused by hypoperfusion of the kidneys -if patient dies, kidneys can be transplanted into another person & will function normally |
|
|
Describe Hepatic Encephalopathy
|
-due to entry of AMMONIA from the portal vein into the systemic circulation
-under normal circumstances the substances generated by the nitrogen-producing bacteria in the intestine are removed from the Portal Venous blood by the liver -In patients with Cirrhosis, the venous blood from Portal System bypasses liver and enter Systemic Circulation -Ammonia gets to brain -> Coma |
|
|
What are the signs/symptoms of Hepatorenal Syndrome?
|
1. Oliguria
2. increased BUN 3. increased Creatinie 4. concentrated Urine & Hyperosmolar 5. unresponsive to Diuretic therapy |
|
|
Define Cirrhosis
|
End-stage liver disease characterized by:
1. loss of normal architecture 2. widespread fibrosis, bridging from portal to portal or Centrolobular to Portal zones, and encircling parts of liver parenchyma 3. Nodular transformation of the parenchyma |
|
|
List 7 causes of Cirrhosis
|
1. Alcohol
2. Viral Hepatitis 3. Biliary diseases 4. Hemochromatosis 5. AAT deficiency 6. Wilson Disease 7. Cryptogenic cirrhosis (15%) |
|
|
What are the clinical manifestations of Cirrhosis?
|
1. Portan HTN = Ascites, Splenomegaly, Varices (esophageal & hemorrhoidal)
2. Metabolic disorders 3. Bleeding tendency 4. Hepatic encephalopaty = due to ammonia 5. Hepatorenal Syndrome = due to decrease kidney perfusion |
|
|
What are the lab findings in Cirrhosis?
|
1. prolonged PT
2. Hypoalbuminemia 3. Hyperbilirubinemia 4. increased ALT, AST, ALP |
|
|
What is a complication of Cirrhosis?
|
Liver Cell Carcinoma = Hepatocellular Carcinoma
|
|
|
What is the mechanism of fibrosis in Cirrhosis?
|
produced by Ito cells (Stellate cells)
|
|
|
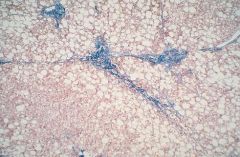
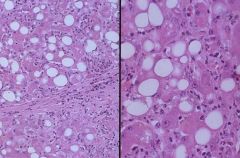
Cirrhosis
|

What is this picture showing?
|
|
|
Cirrhosis
-nodularity |

What is this picture showing?
|
|
|
Cirrhosis
-nodularity |
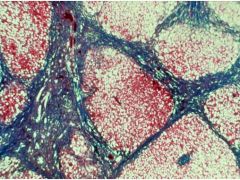
What is this picture showing?
|
|
|
What is the definition of Ascites?
|
Accumulation of fluid in the abdominal cavity
|
|
|
When is Ascites detectable?
|
> 500 ml
|
|
|
Discuss the pathogenesis of Ascites in Cirrhosis
|
1. Portal HTN = increase in portal vein hydrostatic pressure
2. Hypoalbuminemia = liver does not synthesize albumin = decreased oncotic pressure 3. Secondary Hyperaldosteronism = decreased CO activates renin-angiotensin-aldosterone system; liver is unable to metabolize Aldosterone |
|
|
What does it mean if PMN's are found in the serous fluid in Ascites? What if RBC's are found?
|
PMN = infection
RBC = tumor (hepatocellular carcinoma, ovarian CA, pancreas) |
|
|
List the virus families associated with each of the Hepatitis Viruses
|
A = PicornAvirus
B = Hepadnavirus C = Flavivirus E = Calicivirus |
|
|
Aside from Hepatotrophic viruses, what other viruses can cause Viral Hepatitis?
|
Yellow Fever
Epstein-Barr virus Herpes Simplex Cytomegalovirus |
|
|
What Viral Hepatitis' are transmitted fecal-orally?
|
A & E
|
|
|
What Viral Hepatitis' are blood-borne viruses?
|
B, C, D
|
|
|
Hepatitis virus that causes a "ground-glass" appearance
|
HBV
|
|
|
Hepatitis viruses associated with Hepatocellular Carcinoma
|
B & C
|
|
|
What are the microscopid changes associated with Acute Viral Hepatitis?
|

Liver cells = hydropic change, bile stasis, apoptosis, necrosis & regeneration
Kupffer cells = reactive changes, increase in number Inflammatory cells = Macrophage, Lymphocytes in portal tracts and lobules |
|
|
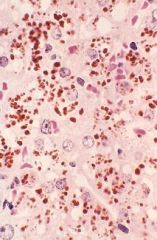
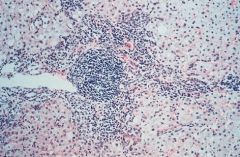
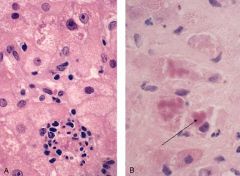
Acute Hepatitis
|
What is seen here?
|
|
|
Acute Viral Hepatitis
-lobular disarray -hepatocyte swelling -apoptotic hepatocytes -lympocytes in portal tracts & lobule |
What is seen here?
|
|
|
What are the microscopid finding in Chronic Hepatitis?
|

Persistent signs of Acute Hepatitis
-lobular disarray, reactive changes, inflammation INFLAMMATION SPILLS INTO THE PARENCHYMA CAUSING "INTERFACE HEPATITIS" = piecemeal necrosis of limiting plate Portal fibrosis -> Bridging Fibrosis -> Cirrhosis |
|
|
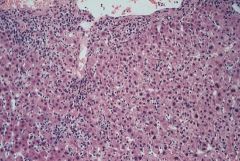
Chronic Active Hepatitis = inflammation has spilled into the Parenchyma
|
What is seen here?
|
|
|
Chronic Persistent Hepatitis = confined to the Portal Tracts
|
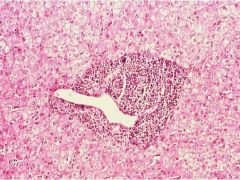
What is this?
|
|
|
Chronic Hepatitis
-Lymphocyte aggregates |
What is seen here?
|
|
|
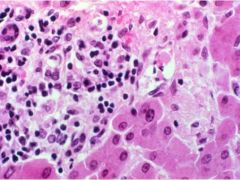
Chronic Active Hepatitis
-Interface Hepatitis = Piecemeal necrosis of LImiting plate |
What is seen here?
|
|
|
Define Fulminant Hepatitis
|
Hepatic Failure with Encephalopathy within 2-3 weeks of onset
|
|
|
What causes Fulminant Hepatitis 60% of the time? 30%?
List 4 rare causes |
60% = Viral Hepatitis = HBV & HCV
30% = Drug-induced & chemical = Tylenol 1. Ischemic necrosis 2. Hepatic Vein obstruction 3. Steatosis syndrome (eg. pregnancy) 4. Malignant tumors |
|
|
Fulminant Hepatitis
|
What is seen here?
|
|
|
Describe Bacterial infections of the liver via the Arterial route
|
Bacteria reach the liver via the Hepatic Artery during SEPSIS or in SEPTIC THROMBOEMBOLI in bacterial endocarditis
-Streptococcus -Staphylococcus aureus -Salmonella |
|
|
Describe Bacterial infections of the liver via Portal Vein route
|
from Appendicitis, Diverticulosis, or Mucosal abscesses
-E. coli -Enteric saprophytes |
|
|
Describe Bacterial infections of the liver via the Ascending Biliary route
|
Bacteria ascending into the liver from the Duodenum are most often Gram Negative
-usually occur in patients who have bile stones or other diseases of the biliary tract |
|
|
Describe Direct Invasion of the liver of Bacterial infections
|
-bacterial infection of the gallbladder may extend to the liver
-transdiaphragmatic infection from the infected peritoneum is a rare complication of severe infection & is usually found in terminally ill patients or those who had extensive surgery |
|
|
Bacterial infection of the liver
|
What is seen here?
|
|
|
Protozoa that causes "flask-shaped" ulcers in the Colon & right lobe liver abscesses
|
Entamoeba Histolytica
|
|
|
Trematode (fluke) that is contracted by ingesting fish; causes inflammation of the Biliary Tract & may cause Cholangiocarcinoma
|
Clonorchis sinensis
|
|
|
Trematode with snails as their host, cercariae penetrate skin of humans; causes granulomas, fibrosis, & inflammation of the Portal Vein
|
Schistosoma mansoni & japonicum
|
|
|
This tapeworm is ingested from the excreta of Dogs & Sheep; causes cysts in the liver; rupture of cysts can cause anaphylaxis
|
Echinococcis granulosus
|
|
|
What drug induces Fatty Change?
|
Tetracycline
|
|
|
What drug induces Centrolobular Necrosis?
|
Acetaminophen (Tylenol)
|
|
|
What drug causes massive necrosis of the liver?
|
Halothane
|
|
|
What drugs cause Hepatitis-like changes in the liver?
|
Isoniazid
Methyldopa |
|
|
What drug causes Fibrosis of the liver?
|
Methotrexate
|
|
|
What 2 drugs cause Cholestasis?
|
Chlorpromazine = anti-emetic
Oral Contraceptives |
|
|
What drugs cause Veno-occlusive disease of the liver?
|
Cytotoxic drugs
Pyrrolizidine |
|
|
What drugs cause Thrombosis (Portal or Hepatic vein)?
|
Oral Contraceptives
Estrogens Cytotoxic drugs |
|
|
What drugs cause Peliosis Hepatis (blood-filled cavities in the liver)?
|
Anabolic steroids
Oral Contraceptives |
|
|
List the types of liver disease associated with Alcohol
|
1. Fatty change = >80%; usually asymptomatic, reversible
2. Alcoholic hepatitis = 10-15%; after acute bout of drinking; may be reversible or progress to cirrhosis 3. Cirrhosis = 0-15%; irreversible & lethal if liver is not replaced |
|
|
Explain why Fatty Change occurs with alcohol consumption
|
Substrates of alcohol metabolism are used to synthesize liver Triglyceride (glycerol + 3 fatty acids)
|
|
|
What are the microscopic changes associated with Alcoholic Hepatitis?
|
1. Hepatocyte swelling
2. MALLORY BODIES 3. EVENTUAL FIBROSIS AROUND THE CENTRAL VEIN (TERMINAL HEPATIC VEIN) |
|
|
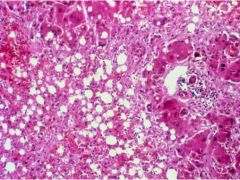
Steatosis due to alcohol consumption
Tender hepatomegaly WITHOUT fever or neutrophilic leukocytosis |
What is this?
What would be the clinical manifestation? |
|
|
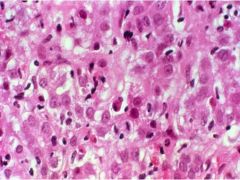
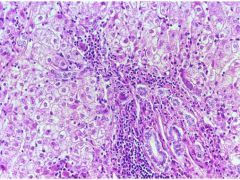
Alcoholic Hepatitis
-Mallory Hyaline -Neutrophils -Necrosis of hepatocytes -collagen deposition -Fatty change |
What is the cause of this?
|
|
|
Alcoholic hepatitis
-hepatocyte swelling -Mallory Hyaline -Neutrophilic infiltration of hepatocytes |
What is shown here?
|
|
|
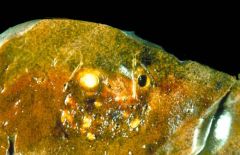
Cirrhosis
-"hobnail" liver appearance |

What is this showing?
|
|
|
Cirrhosis
Alcohol Acetaldehyde stimulates Ito cell to produce fibrous tissue |
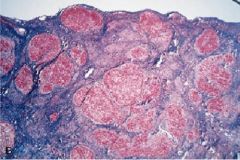
What is seen here? What is the most common cause? What is the mechanism?
|

