![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
66 Cards in this Set
- Front
- Back
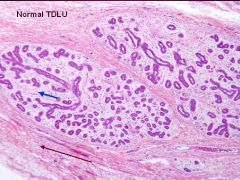
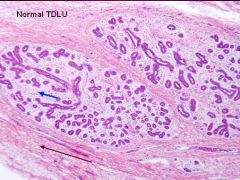
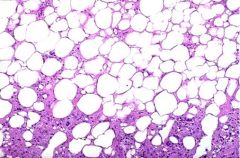
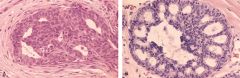
Shown is a normal Terminal Duct Lobular Unit
1. Blue arrow? 2. Brown arrow? Which one is hormonal responsive? |
Blue = Intralobular Stroma
Brown = Interlobular Stroma Hormonal responsive = Intralobular Stroma |
|
|
What does a normal Terminal Ductal Lobular Unit look like?
|
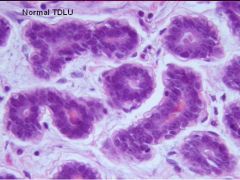
1-2 layers of Epithelial cells surrounded by a layer of Myoepithelial cells
|
|
|
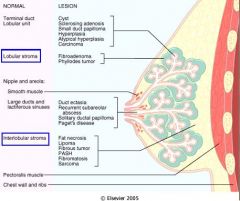
Definition: Dense fibroconnective tissue admixed with Adipose tissue
|
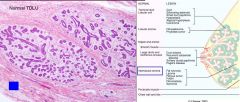
Interlobular Stroma
|
|
|
Definition: An inner ductal epithelium & an outer Myoepithelial layer
|
Functional Secretory Unit = Terminal Duct Lobular Unit
|
|
|
Definition: Loose, delicate, myxomatous stroma that is Hormonally responsive & contains scattered lymphocytes
|

Intralobular Stroma
|
|
|
In a normal breast during which phase of Menstruation are the lobules quiescent (inactive)?
|
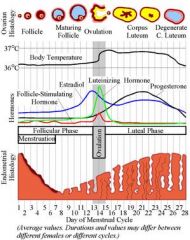
Follicular (proliferative) Phase
|
|
|
In the normal breast, when does the number of acini per lobule increase, epithelial cells vacuolize, and marked lobular stromal edema occurs?
|
After Ovulation
|
|
|
In the normal breast, what 3 things occur after ovulation?
|
1. # of acini per lobule increases
2. vacuolization of epithelial cells 3. marked lobular stromal edema |
|
|
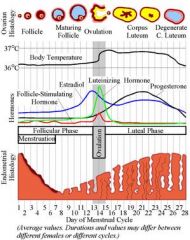
What happens to the breasts during pregnancy?
|
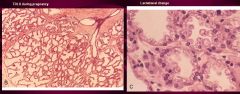
1. Enlarged lobules by increased # of dilated acini
2. true secretory glands form in the lobule 3. secretory vacuoles of lipid material appear 4. after birth, secretion of milk begins |
|
|
In a normal breast, what happens after cessation of lactation?
|
Lobules regress & atrophy
|
|
|
What happens to the breast Post-menopausally?
|
1. Atrohpy of ducts & lobules
2. Shrinkage of Intralobular & Interlobular Stroma 3. Lobular Acini & Stroma may almost totally disappear |
|
|
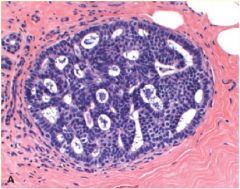
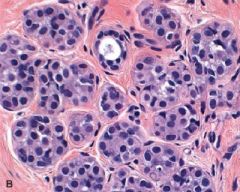
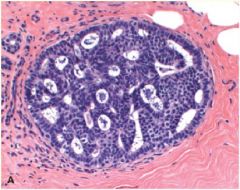
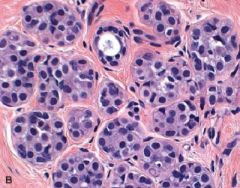
A = normal pre-menopausal breast
B = same as A C = Pregnancy D = Postmenopausal E = Postmenopausal = less dense due to atrophy |
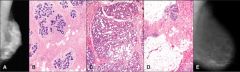
What is shown in A, B, C, D, E?
|
|
|
When does "Acute Mastitis" almost always occur?
What is the etiologic agent? |
Lactation period
S. aureus or Streptococci |
|
|
A woman presents with a UNILATERAL, ERYTHEMATOUS PAINFUL, ABSCESS in her left breast. History is positive for BREAST-FEEDING. Dx? Treatment?
|
Dx = Acute Mastitis due to S. aureus or Streptococci infection
Treatment = Antibiotics & complete drainage of milk |
|
|
Benign breast inflammation that has a strong association with Smoking?
|
Periductal Mastitis = Subareolar Abscess
|
|
|
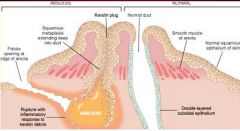
Periductal Mastitis = Subareolar Abscess
Smoking |
What is seen here?
What does it have a strong association with? |
|
|
Describe the pathogenesis of Periductal Mastitis
|
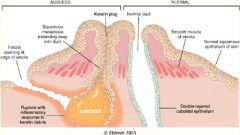
Squamous Metaplasia of Lactiferous Ducts -> Keratin trapped within duct -> dilation -> rupture -> intense inflammatory response
|
|
|
What is the clinical presentation of Periductal Mastitis? What is the treatment?
|
Painful erythematous subareolar mass
Surgical Excision |
|
|
Breast inflammation that usually occurs in older age (50-60) & has a greenish-brown, thick cheesy nipple secretion
|
Mammary Duct Ectasia = Plasma Cell Mastitis
|
|
|
Describe the pathogenesis of Mammary Duct Ectasia
|
1. Inspissation (thickening) of breast secretions
2. dilation of ducts 3. periductal & interstitial chronic granulomatous inflammatory reaction |
|
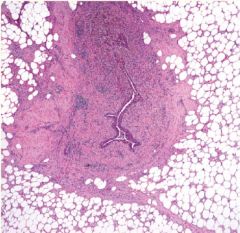
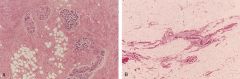
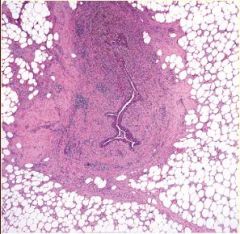
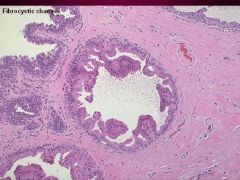
What pathology is this?
|
Mammary Duct Ectasia = Plasma Cell Mastitis
|
|
|
Breast inflammation that often follows trauma or surgery and may possibly be confused with Breast CA as a palpable mass or mammographic calcification
|
Fat Necrosis
|
|
|
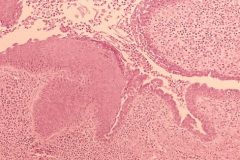
Describe the pathology seen in Breast Fat Necrosis
|
1. Necrotic fat cells surrounded by lipid-filled macrophages & intense neutrophilic infiltration
2. Fibroblastic proliferation, vascularization, lymphocytes & foamy lipid-laden macrophages 3. Calcification 4. Scar tissue |
|
|
Trauma ("seat-belt injury") or surgery
Fat Necrosis |
What is usually the cause of this?
|
|
|
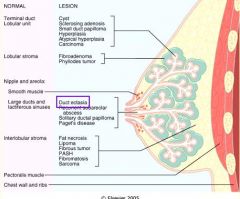
List the 3 Benign Epithelial Breast lesions
|
1. Non-proliferative breast changes = Fibrocystic Changes
2. Proliferative breast disease without atypia 3. Proliferative breast disease with Atypia |
|
|
What is the single most common breast disorder/mass in women <50 yoa?
|
Fibrocystic Changes
|
|
|
What does Fibrocystic Change feel like on breast examination?
|
"lumpy bumpy" feeling
|
|
|
What is the pathogenesis of Fibrocystic Changes due to?
|
Hormonal imbalances b/w Estrogen & Progesterone
**increased Estrogen &/or decreases Progesterones |
|
|
List the 3 histologic types of Nonproliferative Fibrocystic Changes
|
1. Cysts
2. Fibrosis 3. Adenosis |
|
|
Describe the Cysts in Nonproliferative Fibrocystic Change
|
1. Dilation & unfolding of ducts & lobules -> larger cysts (Blue-dome cysts) -> ill-defined diffuse increase in consistency or discrete nodularities
2. Secretory products w/in cysts calcify -> microcalcifications 3. Cysts lined by a flattened atrophic epithelium or epithelium w/ Apocrine Metaplasia |
|
|
Describe Apocrine Metaplasia
|
seen in Fibrocystic Changes in which there are large polygonal cells with abundant granular, eosinophilic cytoplasm
|
|
|
Describe the pathogenesis of Fibrosis in Fibrocystic Changes
|
Cysts rupture -> chronic inflammation & scarring fibrosis
|
|
|
This is a term used to describe an increase in the # of acinar unites per lobule seen in Fibrocystic changes
|
Adenosis
|
|
|
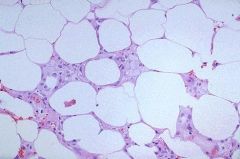
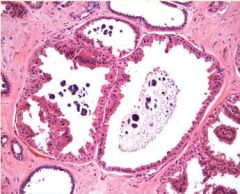
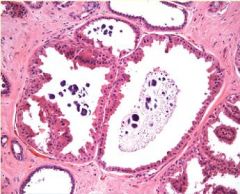
Blue-dome cyst in Fibrocystic Change
|

What pathology is seen here?
|
|
|
Fibrocystic change
-Cysts are visible -fibrosis surrounds the cysts -sometimes the secretions w/in cysts will calcify |
What pathology is this?
|
|
|
Apocrine Metaplasia in Fibrocystic Change = pink/eosinophilic staining cells
|
What pathology is this?
|
|
|
Apocrine Metaplasia in Fibrocystic Change
|
What pathology is seen here?
|
|
|
What characterizes "Proliferative Breast Disease without Atypia"?
|
Proliferation of ductal epithelium &/or stroma without cellular abnormalities
|
|
|
What 3 entities does "Proliferative Breast w/out Atypia" include?
|
1. Moderate or florid epithelial hyperplasia w/out atypia
2. Sclerosing Adenosis 3. Papillomas |
|
|
What 3 entities does "Proliferative Breast w/out Atypia" include?
|
1. Moderate or florid epithelial hyperplasia w/out atypia
2. Sclerosing Adenosis 3. Papillomas |
|
|
Describe "Epithelial Hyperplasia"
|
1. more than 4 cell layers are present
2. Florid, but architecturally & cytologically benign, hyperplasia |
|
|
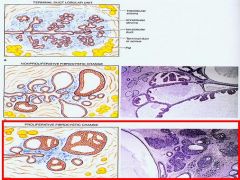
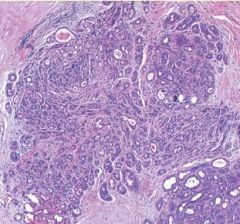
Left = normal
Right = Ductal Hyperplasia w/out Atypia |
Left = ?
Right = ? |
|
|
Epithelial Hyperplasia without Atypia
|
What pathology is seen in both of these pictures?
|
|
|
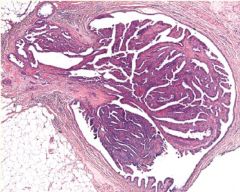
Describe "Sclerosing Adenosis?
|
1. increased # of acinia per Terminal Duct Lobular Units
2. acini are compressed & distorted by the surrounding dense stroma 3. well-circumscribed outer border 4. calfifications are common |
|
|
Sclerosing Adenosis = increased # of acini/TDLU but each acini is still 1-2 layers of epithelium
|
What pathology is this?
|
|
|
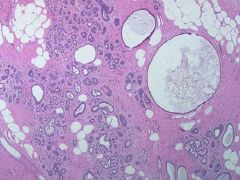
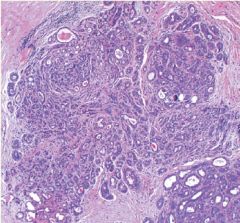
Papilloma in Proliferative Breast Disease w/out Atypia
|
What pathology is this?
|
|
|
What 2 entities does Proliferative Breast Disease WITH Atypia include?
|
1. Atypical Ductal Hyperplasia
2. Atypical Lobular Hyperplasia |
|
|
Benign breast lesion characterized by proliferation of ductal epithelium with cellular and architectural abnormalities
|
Atypical Ductal Hyperplasia seen in Proliferative Breast Disease w/ Atypia
|
|
|
Benign breast lesion that has a monomorphic cell population, regular cell placement, and round lumina. Is qualitatively & quantitively short of ductal carcinoma in-situ
|
Atypical Ductal Hyperplasia
|
|
|
Benign breast lesion characterized by a population of monomorphic small round cells partially filling a lobule
|
Atypical Lobular Hyperplasia
|
|
|
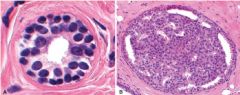
Atypical Ductal Hyperplasia seen in Proliferative Breast Disease w/ Atypia
|
What pathology is this?
|
|
|
Atypical Lobular Hyperplasia
|
What pathology is this?
|
|
|
Benign breast lesion that confers no increased risk of developing invasive breast cancer
|
Non-proliferative Fibrocystic Change
-Cysts -Fibrosis -Adenosis |
|
|
Benign breast lesions that confer a 1.5 - 2 fold increased risk of developing invasive Breast CA
|
Proliferative Breast Disease without Atypia
-Epithelial Hyperplasia w/out Atypia -Sclerosing Adenosis -Papillomas |
|
|
Benign breast lesion that confers a 4-5 fold increased risk of invasive Breast CA
|
Proliferative Breast Disease w/ Atypia
-Atypical Ductal Hyperplasia -Atypical Lobular Hyperplasia **the risk is equal in both breasts |
|
|
What is the rank of Breast CA as a cause of death in women?
|
2nd to Lung CA
|
|
|
T or F: Breast CA is the most common non-skin malignancy of women
|
True
|
|
|
When is breast CA uncommon?
When does incidence peak? Fraction of women who will develop Breast CA in lifetime |
before age of 35
around Menopause 1/9 |
|
|
What is the strongest associated risk factor for Breast CA?
|
+ family history, especially in first-degree relative
|
|
|
BRCA that is associated with hereditary Breast & Ovarian Cancers
|
BRCA-1
|
|
|
BRCA that is associated with a younger age of onset & has a greater incidence of Medullary CA's & higher grade tumors
|
BRCA-1
|
|
|
BRCA that is associated with an older age of onset & an increased CA risk in Male breasts
|
BRCA-2
|
|
|
BRCA that has similar pathology as sporadic carcinomas
|
BRCA-2
|
|
|
List the races who have higher risk factors for Breast CA
|
Caucasians > AA's > Asian > Hispanic
|
|
|
Explain how "hormonal influences" are risk factors for Breast CA
|
Early menarche, late menopause, older age at 1st kid, nulliparity -> increase imbalanced exposure to estrogen -> estrogen receptors -> growth factors secretion -> unregulated cell growth & tumor progression
|
|
|
What environmental factors are risk factors for Breast CA?
|
1. Geographic distribution
2. Dietary fat content 3. Environmental contaminant (organochlorine pesticides) *Smoking is NOT a risk factor |

