![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
Explain how the Liver is attached to the GI tract
|
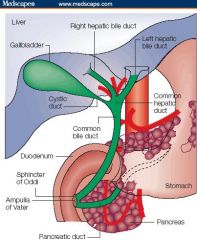
-Liver is connected to the Duodenum by the extrahepatic bile ducts
-Hepatic ducts drain the bile from the liver, forming the Common Bile Duct -Common Bile Duct is laterally attached to the Gall Bladder by the Cystic Duct -terminal portion of the Common Bile Duct passes thru the head of the pancreas & prior to entering the duodenum is confluent with the Main Pancreatic Duct at the Papilla of Vater |
|
|
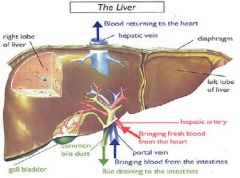
Describe the blood supply of the Liver
|
Liver had DUAL blood supply
-2/3 arrives from the Portal Vein -1/3 arrives from the Hepatic Artery |
|
|
Describe how blood flows through the liver
|
1. Portal Vein and Hepatic Artery form several branches which terminate in the Portal Tracts
2. Portal Vein & Hepatic Artery empty blood into Sinusoids of the Hepatic Acinus 3. Sinusoidal blood drains into the Terminal Hepatic Venule 4. Terminal Hepatic Venule -> Hepatic Vein -> IVC |
|
|
What comprises the Portal Tract?
|
1. Bile Ducts
2. Portal Vein 3. Hepatic Artery |
|
|
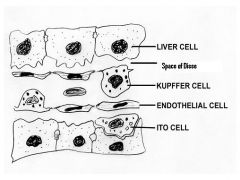
Describe the Sinusoids of the Liver
|
-Modified capillaries that form the vascular spaces of the Acinus
-Fenestrated Endothelial Cells = lined with a discontinuous basement membrane that separates the lumen from the perisinusoidal Space of Disse |
|
|
Describe Kupffer Cells
|
-fixed Macrophages located in the spaces of Disse
-phagocytic & participate in the uptake of particulate material from circulation (ie - take up fragments of destroyed RBC's in hemolytic anemia) |
|
|
Describe liver Stellate Cells (Ito cells or Lipocytes)
|
Fat-storing mesenchymal cells known to be an important storage site for Vitamin A
-in Cirrhosis they transform into collagen-producing myofibroblasts |
|
|
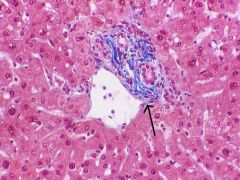
Left = Portal Tract
Right = Terminal Hepatic Venule (Central Vein) |
What is shown at the left?
Right? |
|
|
What is the "Limiting Plate"?
|
Interface between the connective tissue of the Portal Tracts and the periportal Hepatocytes
|
|
|
Describe Bile Canaliculi
|

Bile-filled narrow spaces formed between adjacent hepatocytes
|
|
Fill in the blanks
|
-
|
|
|
What % of Cardiac Output does the Liver receive?
|
25%
*Hepatic Artery brings in 30-40% of blood *Portal Vein brings in 60-70% |
|
|
Describe the "Hepatic Lobule"
|
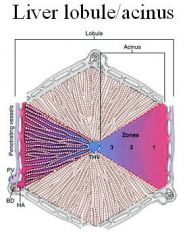
Liver cells are arranged around the Terminal Hepatic Venule (Central Vein)
|
|
|
Describe the "Hepatic Acinus"
|
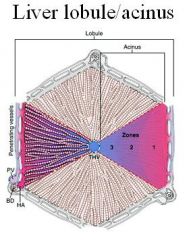
Portal Tracts are the centers of the functional hepatic units
-blood enters into the center of the unit & flows toward the periphery to finally reach the THV |
|
|
Describe what happens in Cholestasis
|

Bile Canaliculi become dilated
|
|
|
Discuss the Metabolic functions of the Liver
|
Hepatocytes process almost all nutrients entering the body thru the GI tract
-Carbohydrate, Amino acid, & fat metabolism |
|
|
Discuss the Secretory function of the Liver
|
Synthesizes almost all blood plasma proteins, lipoproteins, and glycoproteins
|
|
|
Discuss the Storage function of the Liver
|
-Store energy and metabolites, predominately in the form of lipids and carbohydrates
-Store Vitamins (folic acid, B12, vitamin A), Oligominerals (Copper & Iron) |
|
|
Discuss the Excretory function of the Liver
|
Excretes Bile, Bilirubin, & lipids (cholesterol) into the GI tract
|
|
|
Which LFT's are used to assess the Hepatic Secretory function?
|
1. Serum Albumin = synthesized constantly & has half-life of ~ 3 wks = takes time to develop Hypoalbuminemia
2. Coagulation proteins = use Prothrombin Time (PT) to assess liver fxn loss |
|
|
Which LFT's are used to assess the Excretory functions of the Liver?
|
1. Bilirubin = conjugated bilirubin that cannot be excreted into the Intestine accumulates in the blood and can be measured as Direct Bilirubin
2. Alkaline Phosphatase = found along the liver cell membrane lining the intercellular canaliculi 3. Gamma-glutamyl transpeptidase = primarily a hepatic enzyme (vs. Alk Phos) = marker of liver cell injury (esp. alcohol-induced injury) |
|
|
What are elevated levels of Alkaline Phosphatase typical of?
|
Obstructive Jaundice
*Alk Phos is found along the liver cell membrane lining the Intercellular Canaliculi |
|
|
What lab tests are used to assess Liver Cell injury?
|
1. Aspartate Amino-transferase (AST)
2. Alanine Amino-transferase (ALT) **cytoplasmic enzymes released into circulation upon liver cell injury **not liver specific but liver is major source of these plasma enzymes |
|
|
What are the 3 most common causes of Fatty Liver?
|
1. Obesity
2. Diabetes 3. Alcohol |
|
|
List some reversible changes that occur in Liver injury
|
1. Hydropic change
2. Ballooning & feathery degeneration |
|
|
What is glycogen accumulation in the Liver most commonly due to?
|
Diabetes
|
|
|
What would cause Hemosiderin accumulation in the Liver?
|
Hemochromatosis
Multiple blood transfusions |
|
|
What is Centrolobular Necrosis?
|
necrosis in Zone 3 = part furthest away from Portal Tract but close to the Terminal Hepatic Venule = last part to receive blood
|
|
|
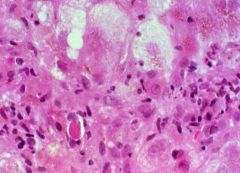
Macrovesicular Fatty Liver
-Fatty change due to Chronic Alcoholism -Mallory Hyaline is also present |
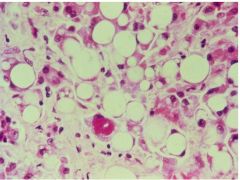
What is seen here?
|
|
|
Alcohol-induced hepatitis
-fatty change -focal liver cell necrosis -infiltrates of neutrophils -Mallory Hyaline |
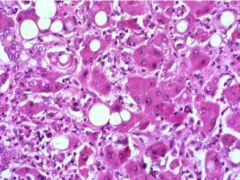
What is seen here?
|
|
|
Viral Hepatitis
-Apoptotic cells = Councilman bodies -Lymphocyte infiltration |
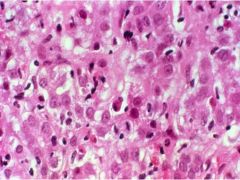
What is seen here?
|
|
|
Viral Hepatitis
-Vacuolar degeneration -Councilman body -inflammatory lymphocytes |
What is seen here?
|
|
|
List the signs & symptoms of Liver Disease
|
Constitutional (nonspecific)
1. Anorexia 2. Nausea 3. Weight loss Jaundice -dark urine -Acholic (pale) stools Bleeding -hematemesis (blood in vomit) -Hematochezia (blood in stool) Hormonal problems -amenorrhea, gynecomastia, impotence, spider nevi, palmar erythema |
|
|
What are the 3 possible signs of Portal HTN?
|
1. Esophageal varices
2. Hemorrhoids 3. Caput Medusa |
|
|
What are the 3 consequences of Portal Hypertension
|
1. Ascites = accumulation of serous fluid in abdominal cavity
2. Generalized edema = Anasarca 3. Hemorrhoids, Caput Medusa, Esophageal Varices |
|
|
Discuss the Pathogenesis of Ascites in Cirrhosis
|
1. Portal HTN = increased hydrostatic pressure leads to transudation of fluid into abdominal cavity
2. Hypoalbuminemia = liver cannot produce adequate albumin 3. Lymphatic Overflow 4. Hyperaldosteronism = aldosterone is released in response to volume regulatory sensors = conserves Na+ & H2O = water overflows into abdominal cavity |
|
|
What are the signs & symptoms of Biliary disease?
|
1. Subcostal & RUQ pain
2. Biliary colic & fever 3. Jaundice 4. Murphy sign = tender gallbladder on taking deep breath 5. Courvoisier sign = palpable distended gallbladder |
|
|
What are the 3 forms of Jaundice?
|
1. Hemolytic
2. Hepatocellular 3. Obstructive |
|
|
Define Jaundice
|
yellow discoloration of the skin, sclera (icterus) & mucous membranes due to increased levels of BILIRUBIN in circulation
|
|
|
Describe how Bilirubin is formed
|
1. release of Heme from RBC
2. Heme -> Biliverdin -> Bilirubin (macrophage in spleen & liver) 3. Bilirubin is bound to Albumin = Unconjugated or Indirect Bilirubin 4. Conjugation of Bilirubin to Glucuronic Acid by UGT in Hepatocytes 5. Excretion of water-soluble Bilirubin Glucuronides = Conjugated or Direct Bilirubin 6. Deconjugation of some Direct Bilirubin by intestinal bacteria to Urobilinogen = 80% is excreted in feces together with Conjugated Bilirubin 7. Recirculation of Urobilinogen in Enterohepatic cycle; small amount is excreted in urine |
|
|
What enzyme performs Bilirubin conjugation?
|
Uridine Diphosphate-Glucuronosyl Transferase (UGT1A1)
|
|
|
What 2 things would cause increased production of Bilirubin?
|
1. Hemolysis
2. Hematomas |
|
|
What syndrome has reduced hepatic uptake of Bilirubin?
|
Gilbert Syndrome
|
|
|
What conditions have reduced conjugation of Bilirubin resulting in Jaundice?
|
1. Physiologic in Neonates
2. Gilbert Syndrome (some) 3. Crigler-Najjar Syndrome (deficiency of Glucuronosyl Transferase) 4. Hepatitis (viral or drug-induced) |
|
|
What conditions have reduced excretion of Bilirubin leading to Jaundice?
|
1. Dubin-Johnson syndrome
2. Rotor syndrome 3. Hepatitis (viral or drug-induced) **result in Conjugated Hyperbilirubinemia |
|
|
List 6 causes of Extrahepatic Bile Duct Obstruction resulting in Jaundice
|
1. Gallstones
2. Tumors of the Common Bile Duct, Ampulla of Vater, Head of pancreas 3. Primary Sclerosing Cholangitis 4. Strictures due to Surgery 5. Congenital Atresia 5. Parasites = Liver flukes, Ascaris |
|
|
Define Cholestasis
|
condition where Bile cannot flow from the Liver to the Duodenum
|
|
|
What are the signs & symptoms of Cholestasis?
|
1. Jaundice due to Conjugated Bilirubin
2. Pruritis = due to bile acids circulating in the blood 3. Xanthomas = due to cholesterol that is normally excreted in Bile, are taken up by Macrophages 4. Acholic stools (pale stools) = due to absence of bile excretion 5. Dark urine = due to Bilirubin 6. Malabsorption, steatorrhea, Vitamin deficiency (DAKE vitamins) |
|
|
What lab findings are consistent with Cholestasis?
|
1. increased CONJUGATED Bilirutin
2. increased Alkaline PHosphatase 3. increased GGT |
|
|
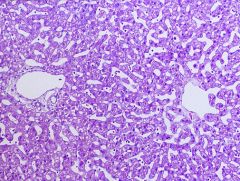
What are the liver biopsy findings consistent with Obstructive Jaundice?
|
1. Bile plugs in Intercellular Canaliculi
2. Bile accumulation in Liver cells -> feathery degenaration -> Bile lakes -> Bile infarcts 3. Uptake of bile by Kupffer cells 4. Bile duct proliferation 5. Portal fibrosis -> Portal-Portal bridging fibrosis -> biliary cirrhosis |
|
|
Obstructive Jaundice
-bile is present in Intercellular Canaliculi |
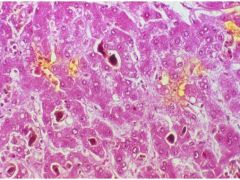
What is this showing?
|

