![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
Describe a Fracture after 2 days
|
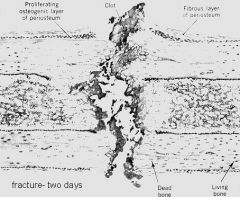
1. Blood Clot is formed
- good b/c blood has lots of Growth Factors to enhance repair & healing 2. At periphery & Endosteum, there is marked proliferation of Osteoblasts 3. There is no overt Callus formation (Callus = new bone) |
|
|
Describe a Fracture after 1 week
|
1. Primary Callus forms at broken ends of bone
2. Outside is Cartilage & is a sign that repair is due to Endochondral formation = indirect bone formation from a "cartilage model" 3. Endosteum is usually linked by Callus, bone |
|
|
Describe Fractures month-years post fracture
|

1. Osteoclasts dissolve the temporary bone & Osteoblasts lay new bone
2. The action of Osteoblasts maximally resist fracture at the same location; if you bend the bone it will rarely fracture in the same place |
|
|
Autosomal Dominant mutation in Fibroblast Growth Factor Receptor 3 (FGFR3) that causes impaired proliferation of Cartilage at the Growth Plate
|
Achondroplasia
|
|
|
Achondroplasia = bone is short but broad at the Epiphysis
-narrow Epiphyseal Plates & Bony sealing off of the area between the Epiphyseal Plate & Metaphysis |

What is this picture showing?
|
|
|
Achondroplasia
-Growth Plate is disordered, cells are not in a regular array -Activation of FGF#3 inhibits Cartilage synthesis at the Epiphyseal Growth Plate, resulting in decreased Endochondral Bone formation & premature ossification of Growth Plates |
What is seen here?
|
|
|
Achondroplasia = mutation in FGFR3
-short & thick Long bones -Cranial & vertebral bones are spared = relatively large head & trunk |

What is the cause?
|
|
|
Autosomal dominant disease resulting in defective synthesis of Collagen type I & insufficient Bone Matrix synthesis
|
Osteogenesis Imperfecta
|
|
|
Pathogenesis: A reduction in Bone Matrix, which alouth fully calcified, results in fragile bones that are more prone to fracture
|
Osteogenesis Imperfecta
|
|
|
Osteogenesis Imperfecta = abnormal synthesis of Collagen I
|

What is the cause of this?
|
|
|
What are the clinical features of Osteogenesis Imperfecta?
|
1. Generalized Osteopenia (brittle bones) = recurrent fractures & skeletal deformity
2. Blue Sclera 3. Early tooth loss 4. Joint Hypermobility 5. Deafness = due to involvement of teh bones of Inner & Middle ear |
|
|
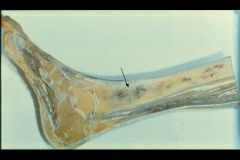
Osteogenesis Imperfecta
-bones are calcified but hypodense b/c they are thin -bent tibia shows fracture |

What is the cause of this?
|
|
|
Osteogenesis Imperfecta
-Cortex is very thin -Bone Trabeculae are thin, widely spaced, & fragile looking |
What is seen here?
|
|
|
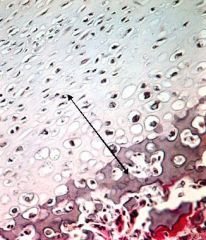
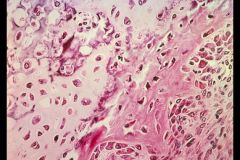
Osteogenesis Imperfecta
-Osteocytes are very close together = indicates insufficient Matrix synthesis -Osteoblasts can't secrete enough Collagen I -Blue staining shows that it is fully Calcified = not due to improper calcification |
What is seen here?
|
|
|
Osteogenesis Imperfecta
-there is no impairment of Endochondral bone formation -if you see a fracture site, you see excessive Cartilage formation since Collagen II is not impaired |
What is seen here?
|
|
|
Osteogenesis Imperfecta post-fracture
-Cortex is thin -can be mistaken for Osteosarcoma |

What is seen here?
|
|
|
Hereditary disease with decreased Osteoclast function leading to decreased resorption & thick sclerotic bones
|
Osteopetrosis
|
|
|
What is the pathogenesis of Osteopetrosis?
|
Impaired Osteoclastic resorption of bone leads to excessive bone formation
|
|
|
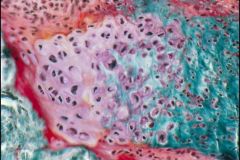
Osteopetrosis
-Anemia, Thrombocytopenia = due to Trabeculae crowding out Bone Marrow |
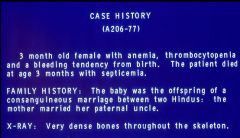
Diagnosis?
|
|
|
Osteopetrosis = dysfuction of Osteoclast activity
-"Erlenmyer Flask"-shaped deformity |

What is the cause of this?
|
|
|
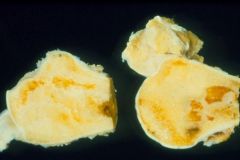
Osteopetrosis
-projections of dense bone down into the Metaphysis |
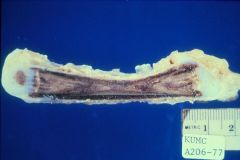
What is the cause of this pathology?
|
|
|
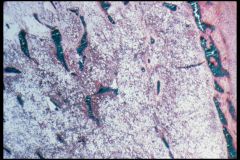
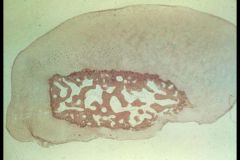
Osteopetrosis
-persistence of lots of Cartilage in the matrix of Medullary Bone -lack of Trabeculae or Hematopoietic marrow |
What is seen here?
|
|
|
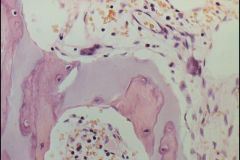
Osteopetrosis
-marked thickening of Trabeculae -> crowds out Bone Marrow -Manifested by Anemia, Thrombocytopenia |

What is this?
|
|
|
What is the Etiology of Fibrodysplasia Ossificans Progressiva (FOP)? Pathogenesis?
|
Etiology: mutated genes for Bone Morphogenetic Proteins (BMP's)
Pathogenesis: in childhood, Osteoprogenitor cells of muscle begin progressive Endochondral Bone formation, in one muscle group after another |
|
|
Fibrodysplasia Ossificans Progressiva (FOP)
Overexpression of Bone Morphogenetic Proteins in muscle -Osteoprogenitor cells of muscle, which normally wait for a fracture to occur so they can make a callus, go haywire & make bone in muscles |

This girl has a piece of bone in her Sternocleidomastoid muscle...what is the name of the disease? What is the cause?
|
|
|
Fibrodysplasia Ossificans Progressiva
|

What disease is this?
|
|
|
Fibrodysplasia Ossificans Progressiva
-cannot surgically resect b/c it would cause more reactive bone formation |
This is seen in muscle. What disease?
|
|
|
Fibrodysplasia Ossificans Progressiva
|

What end-stage disease is this?
|
|
|
What are the most common causes of Hypertrophic Osteoarthropathy?
|
1. Bronchogenic Carcinoma = paraneoplastic syndrome
2. Chronic lung diseases 3. Cyanotic congenital heart disease 4. Inflammatory Bowel Disease |
|
|
Avascular Necrosis = ischemic necrosis of bone & bone marrow
|

What pathology is seen here?
|
|
|
What are the most common causes of Avascular Necrosis?
|
1. Steroid use
2. Sickle Cell anemia 3. Caisson disease = decompression syndrome |
|
|
Advanced Avascular Necrosis
-pitted surface & cartilage disappears in places -painful lesion |
What is seen here?
|
|
|
Joint Mouse in Avascular Necrosis
-cartilage that was covering it regenerates & grows all around the outside -> causes difficulty in Articulation -> joints make a squeaky sound when bended |
What is seen here?
|
|
|
Osteomyelitis
-Staphylococcus Aureus = MCC -E. coli, Klebsiella, Salmonella |
What is seen here? What are the most common causes?
|
|
|
Osteomyelitis
-Marrow space fills up with PMN's -PMN's enzymatically destroy the bone |
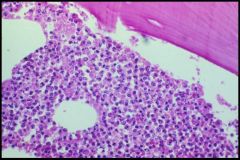
What is seen here?
|
|
|
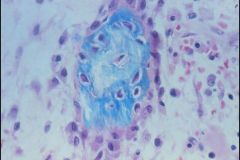
Sequestrum in Osteomyelitis = necrotic bone due to compression of vasculature by Pyogenic Exudate
|
What is seen here?
|
|
|
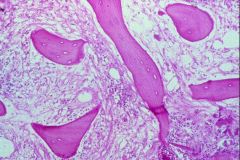
Involucrum surrounding the Sequestrum
-Involucrum = Reactive Bone Formation in the periosteum = has Lamellar appearance |
What is seen here?
|
|
|
Osteomyelitis
-Gelatinous inflammatory infiltrate in the medullary space = Sequestrum -along the outside is new bone formation = Involucrum |
What is seen here?
|
|
|
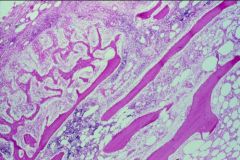
Osteomyelitis of the Phalanx
-infection has broken thru the bone, into the joint & has moved onto the next joint -if infection hits the Growth Plate, it'll stop the growth of long bones = important in children |

What is happening here?
|
|
|
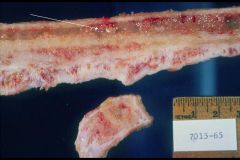
Osteomyelitis that has drained to the outside
-predisposes to Squamous Cell CA of the skin |

What is this picture showing?
|
|
|
Brodie's Abscess = surrounding wall of granulation tissue of inactive inflammation
-post-osteomyelitis |

What is seen here?
|

