![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
List & describe the major components of Bone
|
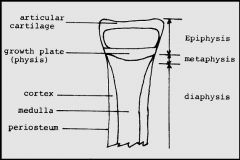
1. Epiphysis = end of long bone that is originally separated from the main bone by a layer of cartilage but later becomes united to the main bone through ossification
2. Metaphysis = zone of growth between Epiphysis & Diaphysis during development of a bone 3. Diaphysis = shaft of the long bone -rigid outer shell of compact bone (Cortex) surrounding central Medullary area filled with thin bone trabeculae & hematopoietic marrow |
|
|
List & describe the major components of Bone
|

1. Epiphysis = end of long bone that is originally separated from the main bone by a layer of cartilage but later becomes united to the main bone through ossification
2. Metaphysis = zone of growth between Epiphysis & Diaphysis during development of a bone 3. Diaphysis = shaft of the long bone -rigid outer shell of compact bone (Cortex) surrounding central Medullary area filled with thin bone trabeculae & hematopoietic marrow |
|
|
Describe the Zones in the Epiphyseal Plate
|

1. Resting Zone = not much goes on but Chondrocytes are alive
2. Proliferating Zone = where all the cell division occurs in the Growth Plate 3. Hypertrophic Zone = chondrocytes enlarge & secrete EC matrix -Longitudinal & Transverse Septa -Longitudinal Septa projects down into the Metaphysis |
|
|
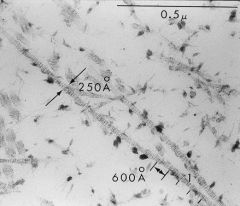
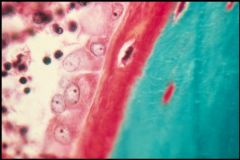
Cartilage Matrix
-Fibrils = Collage type II -Proteoglycan granules = black dots b/w the fibrils -Water |
What is seen here?
|
|
|
Mineralization occuring almost exclusively in the Longitudinal Septa = deposition of Calcium Hydroxyapatite
|
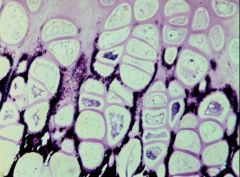
What is this picture showing?
|
|
|
Describe the process of Mineralization
|

In Proliferative Zone there are Matrix Vesicles on the lateral edges of Chondrocytes
-Matrix Vesicles bud off and are distributed into the newly forming matrix; become entrapped between collagen fibrils -deposition of Calcium Hydroxyapatite |
|
|
Describe Matrix Vesicles
|
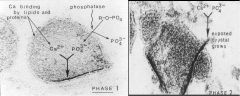
-On the membrane are lipids & proteins that are Ca+ binding
-once the vesicle gets close to the mineralization front, there is increase in Alkaline Phosphatase = hydrolyzed Phosphate + Ca accumulate in the center of the vesicle -> precipitation of Hydroxyapatite -Hydroxyapatite Crystals break through the outer membrane of Vesicles & extend into EC space -exposed crystal grows |
|

What is seen here?
|

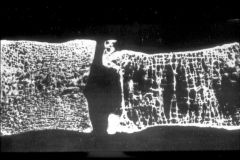
Longitudinal Septum under EM
|
|
|
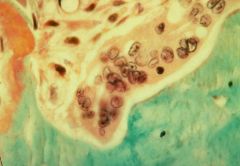
Edge of Trabeculum of Bone & Marrow (lining it are Osteoblasts
-Green = Calcium -Red = Osteoid = Type I Collagen -> becomes mineralized by deposition of Calcium Hydroxyapatite |
What is this picture showing?
|
|
|
Bone Matrix that has been decalcified -> Collagen I Fibers
|
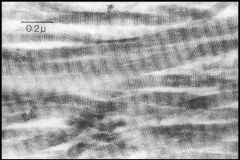
What is seen here?
|
|
|
What is the cause of Scurvy?
|
deficiency of Ascorbic Acid (Vitamin C)
|
|
|
What is the pathogenesis of Vitamin C deficiency?
|
Vitamin C is necessary for the Hydroxylation of Proline & Lysine in Collagen synthesis
-Hydroxylations sites are anchors for cross-linking of alpha-chains -deficiency leads to Collagen with reduced tensile strength |
|
|
What are the clinical manifestations of Scurvy?
|
1. Swollen gums
2. Subperiosteal hemorrhage 3. bleeding into joint spaces 4. Purpura & petechiae 5. impaired wound healing |
|
|
Vitamin C deficiency = Scurvy
-weak blood vessels due to Collagen defect -hemorrhage under the periosteum of the calverium |
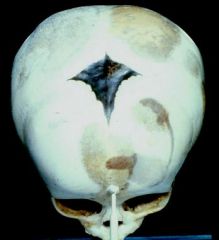
What would cause this?
|
|
|
Scurvy
-Growth Plate with disordered cellular array = chondrocytes are very close to eachother b/c of deficiency of synthesis & secretion of Collagen Type II -accumulation of blood vessels underneath the Growth Plate |
What is the cause of this?
|
|
|
What is the cause of Rickets & Osteomalacia?
|
Vitamin D deficiency
|
|
|
What is the pathophysiology of Vitamin D deficiency?
|
Vitamin D deficiency -> decreased Ca++ absorption in gut -> decreased Calcification of Osteoid matrix
|
|
|
What are the clinical manifestations of Rickets?
|

Skeletal deformities = due to disruption of mineralization at Epiphyseal plates
-Craniotabes = soft skull bones -Rachitic Rosary = overgrowth of costochondral joint -Pigeon breast = outward protrusion of sternum -Lumbar lordosis = spinal curvature -Bowing of the legs |
|
|
List the 3 ways of pathogenesis of Rickets
|
1. Dietary deficiency of Vitamin D3
2. impaired absorption of Ca+ & PO4 3. impaired tubular reabsorption of PO4 **growing bones can't get enough Ca++ or PO4 to support mineralization -> bones become soft & flexible |
|
|
Top = Pigeon Breast = Pectus Carinatum
Bottom = Rachitic Rosary = Costochondral thickening due to enlargement of the Growth Plate Vitamin D deficiency = Rickets |

What are the names of these abnormalities & what is the cause?
|
|
|
Section through a Ricketic rib
-Cartilaginous & bony part of the Costochondral junction -tremendous thickening of the Growth Plate & primarily the Hypertrophic Zone |
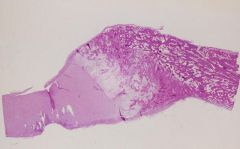
What is seen here? What is the cause?
|
|
|
Rickets growth plate
-only see the Hypertrophic Zone throughout the entire length of the Growth Plate |
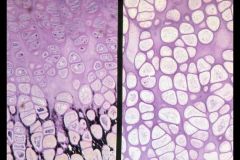
Left is normal, what is the right?
|
|
|
List 5 possible causes of Osteomalacia
|
1. impaired absorption of Vitamin D due to Sprue, persistent mild diarrhea, or inadequate intake
2. dietary deficiency of Ca++ or PO4 3. Hyperphosphaturia in Vitamin D resistant rickets 4. Aluminum toxicity 5. Malignant tumors = Oncogenic Osteomalacia |
|
|
Diseases characterized by DECREASED MINERALIZATION OF NEWLY FORMED BONE, usually caused by deficiency or abnormal metabolism of Vitamin D
|
Rickets = in children
Osteomalacia = in adults |
|
|
Osteomalacia
-hypomineralization of bones = Osteopenia -INCREASED ALKALINE PHOSPHATASE |

Diagnosis?
|
|
|
What are the typical lab findings in Osteomalacia?
|
1. normal to low Ca++ & Phosphorus
2. Increased ALK PHOS |
|
|
Osteomalacia
-trabeculae have core of calcified bone, but are surrounded by coat of unmineralized osteoid -Osteoblasts are lining the bone surfaces -Alkaline Phosphatase is coming from Osteoblasts |
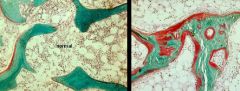
What is the picture on the Right showing?
|
|
|
Pseudofractures in Osteomalacia
-not fractures but are translucent, poorly calcified linear zones -PAINFUL Tx = Vitamin D + Calcium |

What is seen here? What is the treatment?
|
|
|
What are the clinical manifestations of Osteomalacia?
|
1. Bone pain
2. fractures of veterbrae, hips, wrist |
|
|
Decreased bone mass, resulting in thin, fragile bones that are susceptible to fracture
|
Osteoporosis
|
|
|
What are the clinical features of Osteoporosis?
|
1. Compression fractures of Vertebral bodies = shortened stature & kyphosis
2. Bone Pain & fractures 3. Back pain |
|
|
List the risk factors for developing Osteoporosis
|
1. Hereditary = defective Vitamin D receptor gene
2. Loss of ovarian endocrine function = Estrogen deficiency 3. Diet deficient in Calcium, Vitamin D 4. Smoking 5. prolonged Steroid therapy 6. inactivity or weightlessness (astronauts) |
|
|
Why does Estrogen deficiency predispose to Osteoporosis?
|
Estrogen inhibits production of Osteoclasts; enhances Osteoblasts
|
|
|
Right = Osteoporotic Vertebral body -> leads to compression fracture
|
What is this picture showing?
|
|
|
What are the lab findings associated with Osteoporosis?
|
Normal Calcium, Phosphorus, & Alkaline Phosphatase
**compared to Osteomalacia, which has elevated Alk Phos |
|
|
Osteoporosis
|
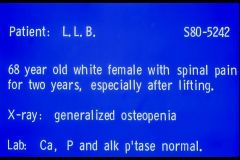
Dx?
|
|
|
Osteoporosis = bone trabeculum is thin
|
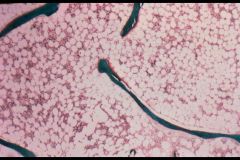
What is seen here?
|
|
|
What are treatments for Osteoporosis?
|
1. Estrogen replacement (still be evaluated)
2. Bisphosphonates = anti-osteoclast agents to inhibit bone resorption 3. Ca & Vitamin D |
|
|
Localized disorder of bone remodeling, resulting in excessive bone resorption followed by disorganized bone replacement, producing thickened but weak bone that is susceptible to deformity & fracture
|
Paget's disease
|
|
|
What are the clinical manifestations of Paget's disease?
|
1. Bone pain
2. Bone growth = increase in hat size |
|
|
Abnormal bone architecture caused by increase in both Osteoblastic & Osteoclastic activity
|
Paget's Disease
|
|
|
Paget's disease = Hyperostosis Frontalis Interna
|

This is the Calverium. What is the disease?
|
|
|
Paget's disease
-increased Alk Phos -normal Calcium & Phosphorus |
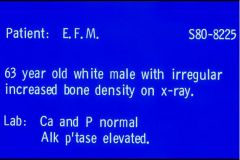
Diagnosis?
|
|
|
Paget's disease
-Osteoclasts are resorbing -Osteoblasts are putting more Osteoid (red) back in = reason for increased Alk Phos |
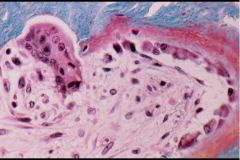
What is this picture showing?
|
|
|
Paramyxovirus, measles, or RSV infection = Paget's Disease
-Osteoclast is seen that is enlarged with more nuclei than normal |
What is the proposed etiology of this disease?
|
|
|
Paget's disease
-tremendous overgrowth of bone with more Osteoid (red) due to Osteoblastic activity -thickening of bone Trabeculae with reduction in marrow space |

What bone condition is seen here?
|
|
|
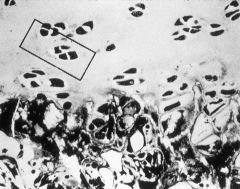
Mosaic Cement lines = Paget's disease
-mixed osteoblastic & osteoclastic activity leads to new bone formation |

What is the name for this? What is the disease?
|
|
|
What are the complications of Paget's Disease?
|
1. High-output Cardiac Failure = due to increased bone vascularity resulting from numberous AV shunts within the marrow
2. Fractures = although bone is thick, it lacks strength 3. Hearing loss = due to narrowing of the auditory foramen 4. Osteogenic Sarcoma in older age |
|
|
A 6-year-old girl is brought in complaining of joint pain. Further inspection reveals a thin, malnourished girl with hemarthrosis, multiple purpura, & ginvival swelling & bleeding. Her mother tells you that she has not been eating a well-balanced diet due to financial situations. Dx?
|
Scurvy = Vitamin C deficiency
results in inability to Hydroxylate Lysine & Proline resides on Collagen (are used for Cross-linking to make fibrils) |
|
|
A 5-year-old boy is brought in concerned of Skeletal abnormalities: protrusion of the sternum, thinning of the occipital & parietal bones resulting in a squared appearance of the head, & rachitic rosary. Dx?
|
Rickets = Vitamin D deficiency = decreased Ca+ absorption = decreased calcification of the Osteoid Matrix
|
|
|
A 74-year-old man presents with the following:
-bone pain in left thigh -bilateral hearing loss -increase in hat size -Lab: increased ALP Dx? What 2 things may this put him at risk for? |
Paget's disease
Osteosarcoma High-output cardiac failure |

