![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
What are the general functions of the skin?
|
- Barrier protection
- Thermoregulation - Sensation - Immunologic defense |
|
|
What is the outermost layer of the skin? What is it derived from?
|
Epidermis - derived from ectoderm
|
|
|
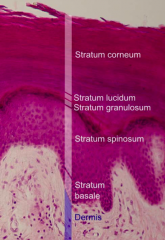
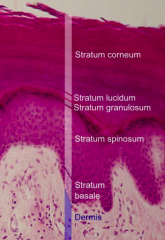
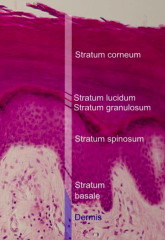
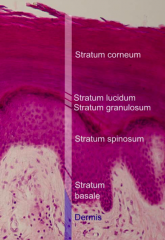
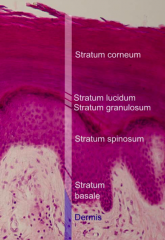
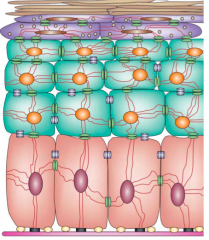
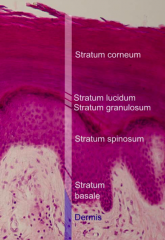
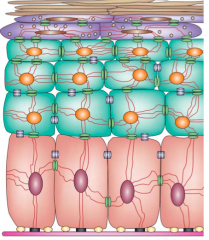
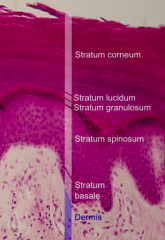
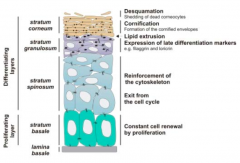
What are the layers of the Epidermis from outer to inner?
|
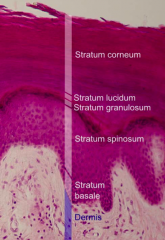
- Stratum Corneum / Cornified Layer
(Stratum Lucidum / Translucent Layer - only in palms and soles) - Stratum Granulosum / Granular Layer - Stratum Spinosum / Spinous Layer - Stratum Basale / Basal Layer |
|
|
What is the deepest layer of the epidermis?
|
Stratum Basale / Basal Layer
|
|
|
What is the Stratum Basale attached to?
|
Basement membrane
|
|
What kind of cells are found in the Stratum Basale? Functions?
|
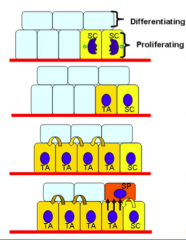
- Keratinocyte stem cells (SC) responsible for maintenance of epidermis - divides into a daughter stem cell and a transient amplifying cell (TA)
- TA cell undergoes cell divisions before separating from BM and moves up to join Stratum Spinosum - Also contains melanocytes - produce melanin (pigment) |
|
What kind of cells are found in the Stratum Spinosum? Functions?
|
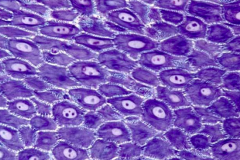
- Most of the keratinocytes of skin - differentiating and synthesizing keratin
- Langerhans cells - antigen-presenting cells localized to skin |
|
|
What kind of junctions occur between the keratinocytes in the Stratum Spinosum?
|
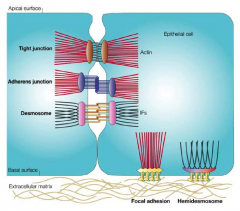
Keratinocytes held together by desmosomes (also gap junctions, adherens junctions, and tight junctions help w/ communication and adhesion)
|
|
|
What is the function of Desmosomes?
|
Connect keratinocytes and their keratin intermediate filament network
|
|
|
In most parts of the body, what makes up most of the epidermis?
|
Stratum Spinosum
|
|
|
What are Keratins? Types?
|
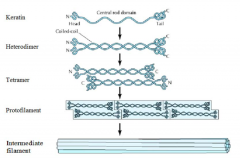
- α-helical proteins that make up intermediate filaments of skin
- Type I (acidic) and Type II (basic) |
|
|
How do keratins form intermediate filaments?
|

- Heterodimerization of type I (acidic) and type II (basic) keratins
- Two heterodimers form a tetramer - Further organized into intermediate filaments |
|
|
What is the function of the keratin intermediate filaments?
|
Connect to desmosomes and hemidesmosomes to form the cytoskeleton network of the epidermis
|
|
|
What is the layer superficial to the Stratum Spinosum?
|
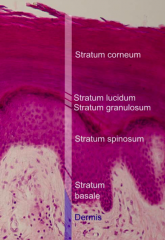
Stratum Granulosum
|
|
|
What is found in the Stratum Granulosum?
|
- Flattened keratinocytes - losing nucleus and organelles
- Keratohyaline granules and Lamellar granules |
|
|
What is in the Keratohyalin granules? Function?
|
- Filaggrin
- Involucrin - Loricrin - Important for formation of cornified envelope |
|
|
What is in the Lamellar granules? Function?
|
- AKA Odland bodies
- Ceramides - Cholesterol - Fatty Acids - Hydrolytic Enzymes - Present in upper layer of Stratum Spinosum, but not secreted until granular layer - Form lipid barrier of cornified layer; hydrolytic enzymes promote desquamation of the cornified layer |
|
|
What is the layer superficial to the Stratum Granulosum?
|
- In palms and soles: Stratum Lucidum
- All others: Stratum Corneum |
|
|
What is found in the Stratum Corneum?
|
Corneocytes: lack nucleus and organelles (dead)
|
|
|
What holds the Corneocytes together in the Stratum Corneum?
|
- Corneodesmosomes
- Filaggrin (from Keratohyalin granules) - Lipids (from Lamellar granules) |
|
|
What is the thickness of the Stratum Corneum?
|
Variable:
- None: oral, genital, and ocular mucosa - Thinnest: face, genitalia - Thickest: palms, soles |
|
|
What is the primary barrier of the epidermis?
|
Stratum Corneum
|
|
|
What is keratinization and how long does it last?
|
- Process of keratinocyte migration and maturation
- Avg. 28 days: - Stratum basale to stratum corneum - 14 days - Stratum corneum to shedding - 14 days |
|
|
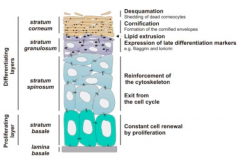
Where does cell renewal and proliferation of keratinocytes occur?
|
Stratum Basale
|
|
|
Where doe cells exit from cell cycle and act to reinforce the cytoskeleton?
|
Stratum Spinosum
|
|
|
Where do cells express late differentiation markers (eg fillagrin and loricrin) and extrude lipids?
|
Stratum Granulosum
|
|
|
Where do cells cornify (form cornified envelopes) and desquamate (shed dead corneocytes0?
|
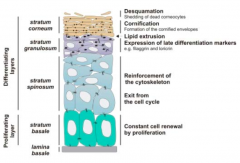
Stratum Corneum
|
|
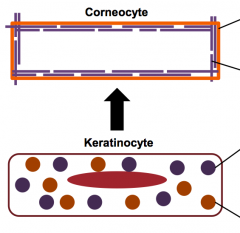
What forms the "bricks" and "mortar" of the corneocyte?
|
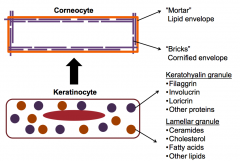
- Mortar: lipid envelope
- Bricks: cornified envelope |
|
|
What are the steps of keratinization / cornification?
|
1. Differentiation of stem cells into keratinocytes and separation from BM
2. Keratinocyte migrates to skin surface and flattens out, losing its water content 3. Lamellar granules and keratohyaline granules start to form 4. Keratinocyte becomes anucleate w/in cornified envelope 5. Shed during process of desquamation |
|
|
What are some disorders of the epidermis?
|
- Pemphigus Vulgaris
- Ichthyosis Vulgaris |
|
|
How do you get Pemphigus Vulgaris? Who is most likely to get it?
|
- Acquired
- Autoimmune disease - Rare, but mainly affects elderly |
|
|
What causes Pemphigus Vulgaris?
|

- Auto-antibodies to desmosomal proteins (Desmoglein 1 and 3)
- Weakened desmosomes leads to intraepidermal blistering |
|
|
What are the clinical features of Pemphigus Vulgaris?
|

- Flaccid, easily ruptured bullae (quickly turn into erosions)
- Oral and mucosal lesions - Nikolsky's sign positive (if you rub on fragile area of skin you can rub skin off - lateral shear pressure causes sloughing) |
|

How do you treat Pemphigus Vulgaris?
|
- Immunosuppressive medications (prednisone, azathioprine and mycophenolate mofetil)
- Rituximab - monoclonal Ab against B cells - used recently too |
|
|
How do you get Ichthyosis Vulgaris? What is the cause?
|

- Autosomal dominant
- Mutation in profillaggrin gene (defective filaggrin protein) - 1 in 250 people |
|
|
What are the clinical features of Ichthyosis Vulgaris?
|
- Ichthyosis means fish scale
- Large scales, especially on extremities, specifically shins - Extremely dry skin - Hyperlinear palms |
|

What other conditions is Ichthyosis Vulgaris associated with?
|
- Atopic dermatitis
- Allergic rhinitis - Food allergies - Asthma |
|

What condition is associated with the following symptoms?
- Flaccid blisters that quickly turn into erosions - Mucosal lesions (mouth, nose, genitals) - Nikolsky's sign (rub on skin causes sloughing) What is the cause and what should you do? |
- Pemphigus Vulgaris
- Caused by auto-antibodies agains Desmoglein 1 and 3 - Tx: immunosuppressive meds (prednisone, azathioprine, mycophenolate mofetil, or rituximab) |
|

What condition is associated with the following symptoms?
- Fish scales (especially on shins) - Extremely dry skin - Hyperlinear palms What is the cause? |
- Ichthyosis Vulgaris
- Mutations in profilaggrin |
|
|
What is the wavelength of UV light?
|
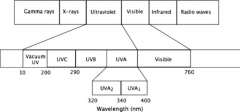
200-400 nm:
- UVC: 200-280 nm - UVB: 280-320 nm - UVA: 320-400 nm (shorter than visible light) |
|
|
What are the characteristics of UVC light?
|
- 200-280 nm
- Absorbed by ozone, very little reaches earth's surface |
|
|
What are the characteristics of UVB light?
|
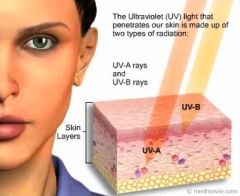
- 280-320 nm
- Penetrates the epidermis and superficial dermis - Primarily responsible for erythema and sunburn |
|
|
What are the characteristics of UVA light?
|
- 320-400 nm
- Penetrates through epidermis and into dermis - Causes tanning and photoaging |
|
|
What types of cancer is UV radiation associated with?
|
- Basal cell carcinoma
- Squamous cell carcinoma - Melanoma |
|
|
What diseases are exacerbated by UV light?
|
- Systemic lupus erythematosus
- Cutaneous porphyrias |
|
|
What are the types of sunscreen? How do they work?
|
- Physical sunscreen: reflects and scatters UV light (ex: titanium dioxide and zinc oxide)
- Chemical sunscreen: absorbs UV light and emits heat (ex: PABA, oxybenzone, avobenzone) |
|
|
What does SPF mean? What does it measure?
|
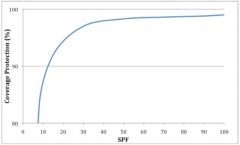
- Sun Protection Factor - measure of protection from UVB exposure
- SPF = MED_protected / MED_unprotected - MED = minimum amount of UVB that causes skin redness at 24 hours |
|
|
What are the characteristics of a good sunscreen?
|
- Broad spectrum
- Water resistant - SPF 30 or greater - 15 minutes prior to sun exposure - 1 oz (shot glass) to cover entire body) |
|
|
How often should you reapply sunscreen?
|
- Every 2 hrs
- More frequently when sweating or swimming |

