![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
10 Cards in this Set
- Front
- Back
|
How are antiarrythmic drugs classified? (4 categories)
|
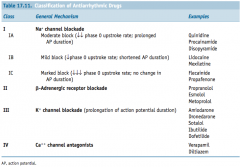
They are commonly classified in four groups, based on their primary electrophysiologic mechanism of action:
1) Class I: Sodium channel blockers (further subdivided in 3 groups based on degree of blockade) 2) Class II: Beta blockers 3) Class III: Potassium channel blockers 4) Class IV: Calcium channel blockers Some drugs don't fit into this schema (eg adenosine and the digoxin) |
|
|
What three mechanisms of arrhythmia do antiarrythmic drugs try to control?
|
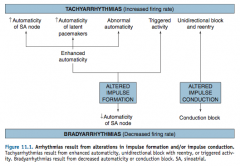
The mechanisms are:
(1) Increased automaticity of pacemaker or non- pacemaker cells, (2) reentrant pathways, and (3) triggered activity. |
|
|
What are the 3 MOAs that anti-arrhythmic drugs work on the cellular level?
|
-effecting the slope of phase 4 depolarization
-effecting the APD -effecting the AP threshold |
|
|
What are the electrophysiological effects of Type 1 drugs (sodium channel blockers)?
|
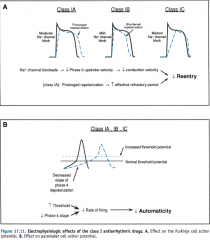
"Type 1 drugs all:
1) Decrease the upstroke velocity of phase 0, slowing conduction velocity and therefore decrease reentry in conducting cells. 2) Decrease the rate of firing in pacemaker cells, directly decreasing automaticity. IA drugs also prolong repolarization of conducting cells, whereas IB decrease repolarization time and IC doesn't affect it. Also the degree of channel blockade decreases as you go down the classes |
|
|
What are the electrophysiological effects of Type II drugs (beta blockers)?
|
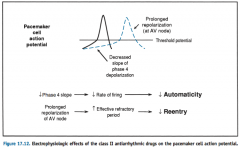
Type II drugs mostly prevent sympathetic stimulation of pacemaker and Purkinje cells, effectively decreasing automaticity.
They also increase the refractory period of AV node cells, decreasing reentry. |
|
|
What are the electrophysiological effects of Type III drugs (potassium channel blockers)?
|
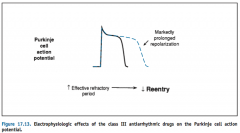
The main effect is significantly prolonging the repolarization of Purkinje and ventricular myocytes.
|
|
|
What are the electrophysiological effects of Type IV drugs (calcium channel blockers)?
|
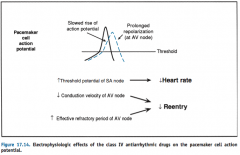
Predominantly acting on nodal tissue they:
1) Decrease the rate of Phase 0 depolarization, and 2) In AV node: increase refractory period, preventing reentry beats. |
|
|
What are two strategies for pharmacologically stopping reentrant beats?
|
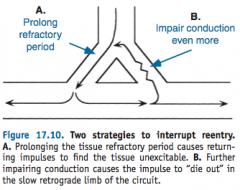
1) Prolonging tissue refractory period so a reentrant impulse attempts to stimulate refractory tissue, and
2) Impairing conduction further so it fails to traverse a retrograde portion of a conduction circuit. |
|
|
What is the mechanism of action for digoxin in controlling arrythmias?
|
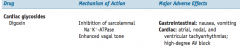
Digoxin increases vagal tone, decreasing conduction velocity and increasing the refractory period at the AV node, aborting reentries.
|
|
|
What are the electrophysiological effects of administered adenosine for controlling arrythmias?
|
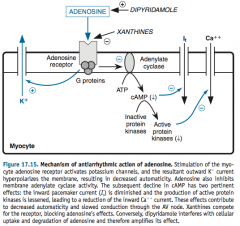
Adenosine has two main effects on nodal cells:
1) Increasing potassium efflux, resulting in hyperpolarized cells and decreasing automaticity. 2) Decreasing inward pacemaker (and Ca++) current, slowing conduction through the AV node. |

