![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
274 Cards in this Set
- Front
- Back
|
What are the requirements for immunogenecity? |
Foreignness Molecular Size Chemical Complexity Degradability and interaction with the host's MHC |
|
|
True or False An immunogen is an antigen? |
True |
|
|
Which of the following is most likely to induce the greatest adaptive immune response in a 25 year old male? A. 250,000 Da plasma protein from the same 25 year old man B. 150,000 Da Toxin produced by a bacterium C. 500 Da Plasma Protein from a chimpanzee D. 400 Da cholesterol molecule from a female. |
B. 150,000 Da Toxin produced by a bacterium
|
|
|
What is the part of the antigen that is bound by the antigen binding site of a B cell receptor |
Epitope |
|
|
True or False: All antigens are immunogens |
False |
|
|
What are the fates of antigens that enter the body via blood, skin, or mucosa? |
enter into blood- carried to spleen where it interacts with APCs which stimulates B and T cells enter into skin- become lodged in epidermal, dermal, or subcutaneous tissue which induces the inflammatory response. Antigen becomes trapped by APCs and is transported to lymph nodes. This stimulates the B and T cells enter into mucosa- become lodged in MALT, interacts with macrophages and lymphocytes, stimulates b cells to produce antibodies |
|
|
The primary lymphoid organs are those in which A. Adaptive immune responses are usually intiated B. Filtration devices remove foreign matter C. Large Numbers of circulating leukocytes make contact with one another D. Lymphocytes undergo their development. |
D. Lymphocytes undergo their development |
|
|
Lymph node question: why can't someone who has had lymph nodes removed on the left side of their body not get blood draws or vaccines in the left side? |
getting a vaccine in the arm lacking lymph nodes means less likelihood for the antigen to interact with B cells to facilitate a response during a later infection. This also means an area without lymph nodes would be more prone to infection which drawing blood and immunizations can cause. More susceptibility lymphedema |
|
|
Secondary Lymphatic Organs Include |
Spleen Lymph nodes Tonsils Appendix Peyer's Patches Lymphoid aggregates of mucosal tissue - mucosa associated lymphoid tissue (MALT) - gut " " (GALT) - Bronchus " " (BALT) - Skin " " (SALT) |
|
|
_______ lymphatic organs are essential for lymphocyte development, whereas _______ lymphatic organs act as traps for foreign microbes and as sites for activation of lymphocytes |
Primary Secondary |
|
|
What are some of the benefits of acute phase proteins? |
Increased iron binding increased coagulation Increased complement proteins Increased opsonins Increased cell recruitment |
|
|
During inflammation which of the following occurs? Increased vascular permeability Recruitment of cells Increased blood flow All of the above A and B only |
All of the Above be reminded that if she said "increased blood velocity" instead of blood flow then that would not be correct |
|
|
What are the hallmark signs of inflammation |
redness pain swelling heat |
|
|
What are some benefits of acute phase proteins |
increased iron binding increased coagulation increased complement proteins increased opsonins increased cell recruitment |
|
|
A person has been born with a mutation that results in a deficiency in the production of MHC1 by all of their cells. How might this deficiency affect a person immunologically? |
Loss of interaction between kIR and MHC1 results in avtivation of NK cells- Cell death of the host No cytotoxic T cell activation Immunocompromised due to loss of development of cytotoxic T cells Death of the individual |
|
|
Early in an infection the body produces a variety of "acute phase proteins" to ramp up an immune response. What sort of benefits do these acute phase proteins provide and what sort of effect would an inability to induce the production of these proteins have on an individual? |
Reduced ability to respond to infection innately and early, leading to reduced recruitment, activation of adaptive cells, etc.. Greater susceptibility, increased extreme infections Loss of coagulation Increased free iron for microbes |
|
|
In what ways can a phagocyte attach to a microbe? |
Pattern Recognition receptors bind directly to PAMPS Pseudopodia attach to microbe Through use of Opsonins (IgG and complement protein C3b) NETs (Neutrophils may use this) |
|
|
Which cell acts as a sentinel and is also involved in the developmental pathways of B and T cell? |
Dendritic Cells |
|
|
Name 3 types of APCs |
Dendritic Cells Macrophages B Cells |
|
|
during a hospital stay a catheter was placed into the urethra of a 70 year old male who subsequently developed a urinary bladder infection. One of the factors that most likely contributed to the establishment of the infection was: A. Introduction of microbes into the urethra during placement of the catheter B. Placement of the catheter bypassed the protective measures of the urinary tract C. Sweat and sebaceous secretions D. All of the Above E. A and B only |
E. A and b only |
|
|
Which of the following is involved in recognition of intracellular pathogens in innate immune cells? A. Toll-Like Receptors B. Antibody C. NOD-like receptors D. Complement |
C. NOD-like receptors |
|
|
Digestion of microbes during phagocytosis involves: |
both hydrolytic/antimicrobial destruction and oxidative/nitrosative stress that result in microbial death Also involves acidification and iron sequestration |
|
|
LPS in the blood will be a bad thing..... why? |
LPS binding protein interacts with LPS and associates it with CD14 and ultimately TLR4 on macrophages and other innate cells Interaction with TLR4 results in espression of inflammatory cytokines Uncrontrolled inflammation can lead to shock and possibly death. |
|
|
What is immunity? |
Mechanisms used by the body as protection against environmental agents that are recognized as foreign to the body - protect from pathogens - eliminate altered self |
|
|
Exposed to trillions of microbeseach day, as you come in contact of _______ barriers you have a reduction ofmicrobes that get into body, anything past those barriers you have the _______ ______ ________which reduces # of microbes and signals for our _______ cells.The recruit _________ cells that have a specific response to microbes who confers long termprotection in the future |
innate innate immune response adaptive adaptive |
|
|
2 Branches of Immunity |
Innate- non specific Adaptive - specific and long term protection |
|
|
WHat can a glitch in the immune system cause? |
autoimmunity, cancer, or chronic inflammation |
|
|
Innate cells |
Defense against any foreign invader nonspecific |
|
|
Innate defenses include: |
body surfaces and internal components: skin, mucus membranes, and cough reflex chemical defense: pH, secreted fatty acid |
|
|
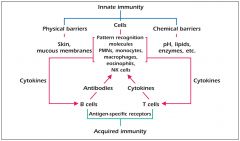
Comparison between innate and adaptive responses |
Innate: no lag period, not antigen specific, no memory development, Immune components are: natural barriers, phagocytes, soluble mediators (complement), pattern recognition molecules (PRM) Adaptive: lag period (at first exposure, at second exposure it is a quicker response), antigen specific, memory development, immune components: Lymphocytes, antigen recognition molecules (b and t cell receptors), secreted molecules (antibody) |
|
|
-Patternrecognition molecules (receptors) (PRM of PRR) are part of the innate response. What do they recognize? |
PAMPS- pathogen associated molecular patterns |
|
|
What are some examples of PAMPS |
Peptidoglycan, LPS, flagellan |
|
|
Other features of the innate response |
complement, fever, interferons, pattern recognition molecules (toll like receptors (sees a series it recognizes) binds to various microbes), phagocytic cells |
|
|
Macrophages |
also part of the innate response Macro-large, Phage- to eat Have receptors that recognize patterns of foreign molecules upon ingestion of microbe it sends signals to other cells (T cells) Example of an antigen presenting cells. |
|
|
Cytokines |
can be found in both innate and adaptive They are hormone like proteins that facilitate communication between cells of the immune system and other cells of the body alert the other responses that there is something foreign in the system |
|
|
Adaptive immunity aka Specific Immunity |
more specialized than innate, specific defense, immunity is acquired by contact with invader and the response is specific to that invader Memory response develops |
|
|
In immunization the initial contact with foreign agent leads to activation of _______and other cells and synthesis of proteins results in acquiring the immunity to withstand subsequent attacks by the same agent. This is the principle behind __________ |
lymphocytes
vaccination |
|
|
What are the three forms of immunization |
Active passive Adoptive |
|
|
Define active immunization and name the two types of it |
administration of antigen: activating your immune response to generate a response & memory Natural: get sick/contract naturally Artificial: Vaccine |
|
|
Define passive immunization and name the two types |
Transfer of specific antibody from an immunized individual to a non-immunized individual. Not producing them on your own/no memory natural- breast feeding, placental transfer Artificial- IgG therapy, cytokine therapy |
|
|
Define adoptive receiving immune cells |
Transfer of immunity by transfer of immune cells ie: transfusion, bone marrow, transplants |
|
|
What are the four requirements for a functional adaptive response?(acquired immune response) |
specificity
adaptiveness discrimination between self and non self memory |
|
|
specificity (acquired immune response) |
the ability to discriminate between different molecular entities |
|
|
Adaptiveness (acquired immune response) |
the ability to respond to previously unseen molecules. aka: diversity or heterogenecity |
|
|
discrimination between self and non self (acquired immune response) |
ability to recognize and respond to molecules that are foreign (non-self) and to avoid making an attack against self. If you bond to self it will become autoimmunity. This discrimination is unique to the adaptive response (not innate) |
|
|
Memory- acquired immune response |
ability to recall previous contact with foreign molecules and to respond to it with a more rapid and larger response aka: Anamnestic response |
|
|
Name the two types of adaptive cells |
T cells B cells |
|
|
Clonal selection theory |
immune response is based on its ability to recognize antigens. For this to work the system eliminates those that recognizes self proteins as foreign. Lymphocytes ( b and t cells) with receptors that bind to self molecules are eliminated early during lymphocyte development - cells that bind to self are programmed to die, the ones that don't can proceed to bind to those that are different so that they can become activated |
|
|
Immune recognition of molecules belonging to self is important to? |
ensure that autoimmunity doesn't occur |
|
|
What is the importance of the clonal selection theory? |
Prevent autoimmunity, self vs. non self recognition following their development. Any cell that binds to self are killed during their development and prior to circulating |
|
|
What are the two branches of adaptive immunity? |
B cell (humoral T cell (cell-mediated) |
|
|
Humoral Immunity is mediated by ________ ______ and secreted by _____ cells after binding of antigens to specific membrane ____ molecules (b cell receptors |
mediated by serum antibodies - secreted by B cells after binding of antigens to specific membrane Ig molecules (b cell receptors) Humoral Immunity is mediated by serum antibodies and secreted by B cells after binding of antigens to specific membrane Ig molecules (b cell receptors |
|
|
When a b cell becomes activated it differentiates into..... |
Plasma cells – after they are activated they get rough ER these are pumping out a bunch of antibodies, they no longer have the receptors, they are secreting the antibodies/b cell receptors And Memory cells- have a receptor, long lived cell |
|
|
What is the product of activated B cells |
antibodies aka Immunoglobulin (Ig) |
|
|
Immunoglobulin molecules (Ig) Their structural features allow them to recognize and bind specifically to a unique structural entity on an _____ of an antigen. |
epitope Preforms a common biologic function after combining with the antigen |
|
|
Immunoglobin is composed of ____ polypeptide chains linked together by ____ bonds. The chains are made of both ____ and ____ regions. The class of antibody is based on the major class of the ____ chain |
four polypeptide chains linked together by disulfide bonds chains are made of both constant and variable regions class of antibody is based on major class of H chain |
|
|
Define the two polypeptide chains of antibodies constant variable regions |
constant- determines particular class that Ig belongs to Variable regions- particular shape and charge that enable the molecule to bind a particular antigen |
|
|
(class of antibodies) Main antibody in circulation; only antibody to cross placenta. Associated with memory response,most abundant and long lived antibody in our blood. binds to pathogens, activates complement and enhances phagocytosis |
IgG |
|
|
(class of antibodies) found in circulation; largest antibody the largest, most commonly found as a pentimer (5 linked together) very effective at agglutination (clumping) because it has so many receptive sites |
IgM
|
|
|
(class of antibody) found in secretions such as saliva and milk prevents pathogens from attaching to epithelial cells in digestive an respiratory tract |
IgA |
|
|
found as antigen receptor on basophils and mast cells in tissue responsible for immediate allergic response and protection against parasitic worms (class of antibody) |
IgE
IgE = eewwwwww b/c of parasites |
|
|
(class of antibody) found on surface of immature B cells. - Signifies the b cell passed clonal selection |
IgD |
|
|
What are the four requirements for a functional adaptive response? |
Memory, adaptiveness, discrimination between self and non self, specificity |
|
|
What is importance of the clonal selection theory? |
Prevent autoimmunity, self vs non self-recognition following their development, any cell that binds to self are killed during their development and prior to circulating |
|
|
To which two cell types does a b cell differentiate into upon activation? |
- Plasma cells and memory B cells |
|
|
Conferring protection to a developing fetus through the transfer of IgG across the placenta is an example of providing immunity by which type of immunization? |
passive |
|
|
What is the purpose of IgD? |
- Signifies the b cell passed clonal selection |
|
|
T cells bind to specific antigens using.... |
t cell receptors |
|
|
T cells interact with an antigen expressed on an ______ |
Antigen presenting cell |
|
|
Types of antigen presenting cells |
macrophages, dendritic cells, and B cells |
|
|
What do Antigen presenting cells do? |
They process and present antigens to specific receptors on T cells. |
|
|
What are the molecules that present antigens? |
MHC1 and MHC2 |
|
|
MHC1 is on all healthy nucleated cells. what does it do |
-Tells us what's going on inside of the cell -Presents cytosolic derived proteins. -Viruses will be processed and presented on MHC1. -The T cells will recognize this, they’re looking for a specific peptide in MHC1 |
|
|
Cytotoxic T cells can only see their specific antigen when it is presented on _____ |
MHC1 |
|
|
MHC II are extracellular derived proteins. What type of T cell can they present to? and where are they found? |
Can present to Helper T Cells- will only recognize peptides in MCHII -Solely found on antigen presenting cells (APCs) such as Macrophages -Dendritic cells -B cells |
|
|
Helper T cells what do they express and what do they interact with? |
express CD4 co-receptor which interacts with MHCII |
|
|
Cytotoxic T Cells- what do they express and what do they interact with? |
Express CD8 co-receptor which interacts with MHCI |
|
|
3 classes of cells responsible for functional adaptive response? |
T cells B Cells APCs |
|
|
Functions of Helper T Cells |
cooperation with B cells to enhance the production of antibodies Inflammatory effects Cytotoxic effects- t cell kills the cell that has cytotoxic effects regulatory effects cytokine effects |
|
|
What are the benefits of immunology |
integral role in prevention of and recovery from infectious diseases essential to the survival of the individual development of immunoprophylaxis |
|
|
What are some damaging effects of the immune response |
in the process of the immune response collateral damage occurs due to inflammation, cytokine production (ie itchiness, redness, burning sensation etc..) Allergic response- is a hypersensitivity and overactive immune response |
|
|
There are four primary types of hypersensitivity reactions. We can put them into two categories what are they? |
category 1: antibody mediated (3 types are antibody mediated) category 2: T cell mediated (1 type is t cell mediated) |
|
|
What happens if there is no immune response or a loss in a component involved in the immune response? |
Immunodeficiency more susceptible to getting sick. Also true if your lacking an innate component (macrophages) or lacking skin |
|
|
t/f an activated t cell produces antibody? |
False |
|
|
t/f CD8 cytotoxic t cells bind to peptide in a MHC class I molecule |
True |
|
|
Cd4 is found on which type of t cell? |
Helper T cell |
|
|
Postulates of clonal selection |
T and B lymphocytes of heterogeneous specificities exist before there is any contact with the foreign antigen. Lymphocytes participating in an immune response express antigen-specific receptors on their surface membranes Upon antigen binding, the cell is activated and releases various products |
|
|
Innate Immune defenses: what do they do? What are they made up of? where are they found? Are they specific? |
First line of defense- limits # of harmful microbes act upon any invading pathogen made up of molecules and cellular processes that defend host within minutes to hours after exposure found in plants vertebrates and invertebrates sends cellular signals to let other cells know there is a problem non specific, just looking for pamps |
|
|
Innate immune defenses include: |
Barriers - physical, chemical, biological cellular defenses- phagocytes Humoral (found in the blood) defenses- complement, cytokines |
|
|
What do burn patients, smokers, and patients receiving long term antibiotic or chemotherapeutic drugs have in common |
poor response of t cells, lacking barrier protection in burn victims, smokers- cilia lines trachea which propel things up in the mucus, cilia is lost in smokers. Causes ciliastasis |
|
|
Name the three types of physical barriers |
skin mucociliary escalator- cilia in the trachea flushing of bladder- mechanical barrier(you get a UTI because you're not flushing things out/urinating) |
|
|
Skin barriers: epidermis How does it protect against harmful bacteria? |
-Tight junctions -Impermeable- because it is a keratinized layer, layers of dead cells that is waterproofing and hardened -Dry -Acidic pH- as you age there are transitions in overall skin pH.Differences in susceptibility, diet can also change it -Sebum-antimicrobial -Sloughing of the skin |
|
|
Skin Antimicrobial Compounds: Lysozyme |
found in sweat, cleaves the peptidoglycan (cell wall) |
|
|
Skin Antimicrobial compounds Defensins |
antimicrobial peptides that cause lyses to the cell by inserting into the membrane |
|
|
Skin antimicrobial compounds Cathelicidins are found in the ______ and the ____ they insert into the membrane and cause ______ |
epidermis and dermis. Insert into membrane and cause lyses |
|
|
The skin also has ______ which is beneficial because they take up space and produce toxic compounds around them to inhibit anything that tries to take up residence around them. Kills things that try to take up their space |
Microbiota |
|
|
what are dendritic cells that are found in the dermis? |
Langerhans cells
|
|
|
mucous membranes barrier defenses |
Lysozyme Defensins pH differences- pH of the ilium is very acidic Mucous-sticky Microbiota- found in the majority of mucous membranes Depending on the location you'll find cilia (respiratory) intestinal tract movement of food is the continuous movement rapid flow so microbes can’t hang on and grow. sIgA- secretory IgA- enhances the stickiness of mucus-Abundance of this in the mucousa it enhances the ability to trap microbes |
|
|
Chemical barriers |
◦Sweat Contains sebum, an antimicrobial fatty acid Acidic pH ◦Hydrolytic enzymes, Lysozyme, ie: Tears ◦HCl Parietal cells in stomach ◦Defensins Anti-microbial |
|
|
Biological Barriers |
◦Normal microbiota Microbes that naturally inhabit the body Defend against invasion - Competition - Antimicrobial substances |
|
|
Cellular Defenses: specialized cells whose purpose is to destroy the invader. Name the cells that act as cellular defenses |
Polymorphonuclear leukocytes macrophages dendritic cells natural killer cells |
|
|
Our immune cells are derived from ? |
progenitor cells the stem cell differentiates into progenitor cells |
|
|
Majority of innate cells will be derived from the _____ progenitor |
Myeloid |
|
|
What types of cells form from the lymphoid progenitor? |
NK cell, T cell and B cell
|
|
|
Cells that are involved in the innate immune system are involved in assisting the induction of specific immune cells. __________ presentation and _________ production |
antigen cytokine cytokine can send out a signal saying there is something foreign-can recruit other cells or can stimulate bone marrow to pump out more innate cells |
|
|
Polymorphonuclear Leukocytes (PMN Cells) Types |
◦Granulocytes : Basophils, Mast Cells, Neutrophils, Eosinophils |
|
|
______ cells contain enzyme rich lysosomes for destroying pathogens and also produce peroxide, superoxide radicals, and other bacterial proteins |
PMN |
|
|
What type of PMN cell comprises 60% of peripheral blood leukocyte, is effective at killing bacteria. |
neutrophils |
|
|
The increase in the number of neutrophils is an indication of an ___________ __________ |
acute infection phagocytic cells will increase in acute infection, NOT antigen presenting cells |
|
|
What releases histamine (inflammation) |
Basophils |
|
|
What are present during allergic reactions and parasitic infections? |
eosinophils they produce major basic protein that destroys parasites |
|
|
catoionic proteins are associated with eosinophils. what do they do? |
can insert membrane of parasite and result in lyses/cell death |
|
|
MHC1 presents antigens from which environment? To which cell does it present peptides? |
- Intracellular environment - Cytotoxic t cells |
|
|
What are benefits of skin? |
Salt, Antimicrobial compounds, impermeable, dry, sloughing,sebum, acidic, microbiota, cathelicidins, lysozyme, UVexposure, barrier, keratin |
|
|
T/F if a pathogen bypasses the epidermis its home free because there is no protective measure in dermis |
false |
|
|
Pathogen associated molecular patterns are recognized by _______ ________ _______of the innate immune system |
pattern recognition receptors |
|
|
3 types of APCs |
Macrophage, dendritic cells, B cells |
|
|
What cell type is associated with parasitic removal? |
Eosinophils |
|
|
What are the benefits of mucus? |
Sticky, antibacterial components, microbiota, sIgA, |
|
|
What functions to engulf and digest invaders, acts as an APC, and is derived from monocytes (found in the bone marrow) |
Macrophages |
|
|
Macrophages differentiate into |
Kupffer cells- found in the liver Alveolar macrophages- lung Splenic macrophages- spleen Peritoneal macrophages - abdominal cavity Microglial cells- nervous tissue (helps to clean up the damaged tissue) |
|
|
Macrophages are included in the reticulo endothelial system (RES) since we can find them in the endothelial lining of blood vessels and lymphatic tissues. what do they do? |
recognize pamps and foreign entities, release cytokines, Bind to foreign PAMPS using PRMs which can initiate phagocytosis to engulf and destroy those cells. |
|
|
What removes dying circulating cells ? |
Macrophages |
|
|
Macrophages are APCs T/F |
True |
|
|
what is the #1 APC for activating T cells? |
Dendritic cells |
|
|
Where are dendritic cells found? |
in T cell areas of lymphoid tissues and in non lymphoid tissues throughout the body |
|
|
Dendritic cells act to stimulate the ________ immune response |
adaptive |
|
|
Dendritic cells are used during the development of B and T cells. What types are used for T cell development? B cell development? |
T cell- Medullary dendritic cells B cell- follicular dendritic cells |
|
|
Large granular lymphocytes that are able to lyse certain virus-infected cells and tumor cells without prior stimulation, Also recognize membranes of altered cells and kill targeted cells |
Natural Killer cells |
|
|
NK cells are derived from the ______ progenitor |
lymphoid |
|
|
Explain how NK cells recognize and kill infectedcells |
The NK Cell has killing Inhibitory receptor (KIR) Which is looking forMCH1. It also has a Killing Activating Receptor (KAR). If the healthy cell has MHC1 the NK cell will bind to it, but not kill it. If it lacks MHC1 (it is dying/or infected cell) then nothing will engage KIR, but KAR is engaged and it sends a positive signal to release killing molecules Perforin: forms pores in the dying cell, and Granzymes- which activates apoptosis. This will kill the cell |
|
|
Natural Killer T Cells are non specific cells. what do they do? |
These are not looking for MHC They just look for lipids in a CD1 receptor (which is a receptor on the host) Natural killer t cell produces cytokines that trigger cell death (apoptosis). |
|
|
NKT cells are NOT the same as NK cells. What are they? |
◦NKT cells are T cells with an αβ TCR. Also express some of the cell-surface molecules of NK cells — hence their name. |
|
|
NKT cells are able to secrete large amounts of either |
◦IFN-γ,a major cytokine of Th1 immune responses ◦IL-4and IL-3, the major cytokines of Th2 responses. |
|
|
Aid in protective immunity at the acute phase of infections, tissue remodeling, anatomical containment, wound healing, and maintaining epithelial integrity at mucosal sites.Have been associated with pathophysiological conditions. Common lymphoid progenitor Do not have rearranged receptors. Produce an array of cytokines to influence other cells and influence inflammation seen prevalently in the inflammatory response |
Innate Lymphoid cells
|
|
|
what are cells that eat or engulf foreign materials, circulate through the body, guard the skin & mucous membranes against invasion by microorganisms |
Phagocytes |
|
|
What are 2 examples of phagocytes? |
neutrophils and macrophages |
|
|
Phagocytes engulf bacteria. If they can't engulf a cell due to biofilm etc... what do they do? |
they basically spew their cytotoxic stuff on the cells which can cause problems |
|
|
Specialized cells destroy invaders by ingesting and then destroying it. what is this called? |
phagocytosis- takes it into cell and ingests it endocytosis through pinocytosis (the ingestion of liquid into a cell by the budding of small vesicles from the cell membrane.) or receptor mediated ( specific molecules are ingested into the cell. The specificity results from a receptor-ligand interaction. Receptors on the plasma membrane of the target tissue will specifically bind to ligands on the outside of the cell.) |
|
|
Specialized cells destroy invaders by ______ _______ preformed without ingesting the invader |
extracellular killing- release oxidative and analytic components from granules |
|
|
Phagocytosis |
Process by which phagocytes digest & destroy invading microbes |
|
|
Neutrophils & macrophages use 4 step process to destroy invading microbe (phagocytosis). Define these |
Find- chemotax is to find PAMPS PRM to find PAMPS cytokines- chemokine (chemokine tells you it is acting as an attractant and is still a cytokine)Compliment proteins that act as attractants (C3a, C4a, C5a) Adhere to: PAMP binding by PRR activates phagocyte Ingest: phagocyte ingests microbes enlarges and increases metabolic activity Digest: -Destroy microbe by -Oxidative/nitrosative stress-Various oxygen or nitrogen radicals can cause oxidation to protein. -Hydrolytic/Acidification/Iron Binding-Killing by using antimicrobial peptides which causes lyses. |
|
|
adherence (phagocytosis) |
◦Phagocyte binds to microbe ◦Opsonins enhance adherence |
|
|
(adhere) The phagocyte can use the PRM to bind to PAMP. There are two ways to do this. Psudopodia, and Neutrophil Extracellular Trap (NET) define these |
Pseudopodia- send out projections as a means to capture Neutrophil Extracellular Trap (NET) – like spider mans web. Neutrophil detects something foreign using PRM and sends out a net which has protein, antimicrobial compounds, sugars, and DNA and it captures these cells and to initiate the killing of the foreign cell |
|
|
(adhere) The phagocyte can also bind to opsonins. describe these methods |
-Opsonins C3b bind to PAMPS on the surface of a microbe. The macrophage then has a complement receptor that binds to the opsonins and initiates attachment. It then professes to ingestions -Opsonin IgG is bound to something specific on the microbe and the macrophage has a receptor known as the FC receptor which recognizes the FC region of IgG and binds. It then progresses to ingestion |
|
|
What are the two categories of opsonins |
complement protein C3b IgG |
|
|
Pattern recognition receptors in phagocytes are receptors associated with the innate response that lack specificity. What do they recognize? |
They recognize conserved microbial structures (PAMPS). |
|
|
What toll like receptor is found on macrophages and detects LPS? |
TLR4- on the macrophage detects LPS causing the macrophage to release inflammatory cytokines Also LPS binding proteins can take LPS to the TLR4 which releases the inflammatory cytokines. Bad??I think if there is too many, but not quite sure |
|
|
Ingest (phagocytosis) |
-Enclose the microbe into a phagosome (phagosome is a membrane bound compartment) -For digestion to occur there is a reduction in pH in the phagosome which results in the fusion between the phagosome and the lysosome inside of the cell. This forms the phagolysosome. |
|
|
Digestion: destroys the microbe by? (two things) |
-Oxidative/nitrosative stress-Various oxygen or nitrogen radicals cancause oxidation to protein. -Hydrolytic/Acidification/Iron Binding-Killing by using antimicrobial peptides which causes lyses. |
|
|
Digestion: lysozymes found in phagocytic cytoplasm contain digestive enzymes and small proteins called _____ that fuse with _____ forming _______ |
defensins, phagosome, phagolysosome |
|
|
◦Damage to microorganisms occurs via: (digestion) |
Acidification Toxic oxygen- derived products (superoxides,hydrogen peroxide) Toxic nitrogen oxides Antimicrobial peptides Antimicrobial enzymes Iron sequestration molecules |
|
|
A complex of proteins called phagocyte oxidase in the membrane of a phagolysosome generates oxygen radicals in the phagosome. A single electron is taken from NADPH and added to oxygen,partially reducing it. The resulting highly reactive molecules react with proteins, lipids and other biological molecules |
Oxygen Radicals |
|
|
synthesizes nitric oxide, a reactive substance that reacts with super oxide to create further molecules that damage various biological molecules. |
Nitric oxide synthase |
|
|
Defensins and what other peptides attack bacterial cell membranes. Similar molecules are found throughout much of the animal kingdom. |
Anti-Microbial Peptides. |
|
|
Lactoferrin binds iron ions, which are necessary for growth of bacteria. Another protein binds vitamin B12. Which protein is that? |
Binding Proteins |
|
|
Inflammation is a response to an infection. phagocytes are activated to release _______. ______ are activated. Increased _______ _______ which is important so white blood cells can get out of blood vessels and go and clear up foreign entities that entered the body. ________ blood flow and _____ in blood velocity |
phagocytes are activated to release cytokines◦ Immune cell recruitment◦ lymphocytes are activated ◦Increased vascular permeability Increased blood flow, but you’ll see a reduction in blood velocity |
|
|
Which leukocyte becomes activated by the absence of MCH1? And what is the effect of this cells activation |
NK Cells- Produces perforin and Granzyme Apoptosis of cell |
|
|
What are the stages of phagocytosis |
Find Adhere to Ingest Digest the microbes |
|
|
What is involved in recognition of intracellular pathogens in innate immune cells |
Nod like receptors |
|
|
3 Hallmark signs of infection and why? |
Redness, pain, swelling, heat: blood flow causes redness and heat, pain is from cytokines and other proteins, swelling because we have vascular permeability also anywhere you have blood vessels you have lymphatic fluid as well |
|
|
In inflammation, what induces the expression of adhesion molecules on endothelial cells slowing down other cells and creating speed bumps/road blocks |
Cytokine and kinin |
|
|
within minutes of injury, increased production of ____ _____ _____ happens called the ___ _____ _____ |
acute phase proteins acute phase response |
|
|
acute phase proteins induce localized and systemic response. This results in activation of ____ and ______ system |
kinins and coagulation systems |
|
|
proteins that are expressed early in infection. Will see the increased production by the liver. They assist in the inflammatory response and reduction of microbial presence. Will also see increased coagulation protein, recruitment, and they can act as an opsonin |
acute phase proteins |
|
|
acute phase proteins are iron binding. Why is that important? |
bacterial cells need iron by inducing iron binding you reduce the ability of bacteria to replicate. |
|
|
Kinins are a type of acute phase protein. what does it do? |
◦Cause smooth muscle contraction◦ Acton axons to block nervous impulses ◦Nerve stimulators Pain and itching ◦Increase vascular permeability and expression of endothelial cell adhesion molecules (ECAMS) |
|
|
The systemic inflammatory response includes |
Fever, increased white blood cells, increased hydocortisone and ACTH, production of acute phase proteins (c reactive protein) This systemic response can start even just from inflamed mosquito bites and is also seen in autoimmune disease |
|
|
Occurs in cases of chronic infection or chronic activation of the immune response |
chronic inflammation example: asthma |
|
|
Fever is caused by |
bacterial products like endotoxins cytokines also can trigger fever such as IL-1- primary cytokine in fever, the more you have the more it increases your fever can be either endogenous or pyrogen |
|
|
Innate Humoral Defenses: multiple proteins produced in the liver. They act as a cascade? How? |
Enhance phagocytosis through opsonization Lyse microorganisms Generate peptide fragments that regulate inflammation and immune responses |
|
|
Glycoproteins produced by a variety cells such as monocytes, macrophages, NK cells, Lymphocytes, and endothelial cells are? |
cytokines, they can have an affect locally and distally. They are produced during early stages of infection |
|
|
Key criteria required for Adaptive Immunity |
1.Adaptiveness/heterogeneity 2.Recognition of self vs non self (developed by clonal selection) 3.Memory 4.specificity |
|
|
Humoral Immunity (adaptive immune response) |
B cell Mediated response which produce antibodies |
|
|
Cell Mediated Immunity (adaptive immune response |
T lymphocyte, cannot simply bind to antigen, APC's process and present antigen to T cell activating the T cell |
|
|
Helper T cells aka |
CD4 |
|
|
Cytotoxic T cells aka |
CD8 |
|
|
_______ presents to T cells? |
MHCII |
|
|
What are APC cells which present MHCII? |
Macrophages, dendritic, and B cells |
|
|
MHCI presents to ______ t cells |
cytotoxic |
|
|
•Organs in which lymphocyte maturation, differentiation, and proliferation take place |
Lymphatic organs |
|
|
lymphatic organs function to: |
•Collect excess fluid from the spaces between body cells;• Transports digested fats to the cardiovascular system• Provides many of the nonspecific & specific defense mechanism.A place to come in contact with innate and adaptive cells |
|
|
Primary lymphoid organs |
Thymus gland- stem cells migrate to thymus and they come in contact with dendritic cells. Thymus provides key points of contact for development of T cells. If you don’t have this then you don’t have T cells bone marrow- is where we have the developmental pathway of B cells |
|
|
Secondary lymphoid organs |
structures in which mature lymphocytes are stimulated by antigens |
|
|
secondary lymphoid organs function |
trap and concentrate foreign material, activation of adaptive cells induction of b cells to produce antibodies induction of antigen specific T cells |
|
|
Secondary organs include |
all removable Spleen Lymphnodes Tonsils Appendix Peyer’s Patches Lymphoid aggregates of mucosal tissue - Mucosa- associated lymphoid tissue (MALT) - Gut-associated lymphoid tissue (GALT) - Bronchus- associated lymphoid tissue (BALT) |
|
|
what is the largest secondary lymphoid organ |
spleen
|
|
|
the spleen is the major organ in which antibodies are synthesized and released. They are composed of? |
white pulp- rich in lymphoid cells Red Pulp- contains many sinuses, erythrocytes, and macrophages |
|
|
Lymph nodes are composed of |
edulla with many sinuses and a cortex surrounded by a capsule of connective tissue
|
|
|
The cortical region of the lymph node contains |
primary lymphoid follicles- these structures enlarge after antigenic stimulation (due to formation of secondary lymphoid follicles that contain B cells which are undergoing mitosis) |
|
|
•Following antigenic stimulation in lymph node, B cells undergo ______ ______ |
affinity maturation where they generate clones having similar affinity receptors for antigen response |
|
|
What does the lymph node cortex contain? What do the deep cortical region of lymph nodes contain? |
APC's and B cells T cells and Dendritic cells |
|
|
explain lymphocyte re circulation |
•Lymphocytes enter lymph nodes through afferent lymphatic vessels• Leave lymph node through efferent vessels• Converge in thoracic duct• Empties into vena cava |
|
|
An antigen that penetrates defenses of the immune system will take the following path if it enters into the bloodstream |
•Carried to spleen, where it interacts with APCs...stimulates B and T cells |
|
|
An antigen that penetrates defenses of the immune system will take the following path if it enters into the skin |
•Become lodged in epidermal, dermal, or subcutaneous tissue•Induces inflammatory response•Antigen becomes trapped by APCs and is transported to lymph nodes•Stimulation of B and T cells |
|
|
An antigen that penetrates defenses of the immune system will take the following path if it enters into the gastrointestinal or respiratory tract |
•Become lodged in MALT•Interacts with macrophages and lymphocytes•Stimulation of B cells to produce antibodies |
|
|
Innate and Adaptive Responses interact |
|
|
|
Out of control innate immune defenses can result in.... |
septic shock |
|
|
out of control adaptive defenses can result in...... |
autoimmune disease |
|
|
Immunogens are |
antigens that bind lymphocyte receptors and activate their response |
|
|
Antigen |
any molecule that has the ability to bind to lymphocyte receptors and may or may not lead to activation |
|
|
The part of the antigen that your antigen binding site is binding |
eptiopes |
|
|
Part of the receptor that binds to the epitope |
paratope |
|
|
Hallmark molecules of adaptive immune response are: |
antibody t cell receptors |
|
|
Immunogen is an agent capable of stimulating _____ ______ |
the immune response |
|
|
The immune response is evoked by an ______ or _______ |
antigen or immunogen |
|
|
antigen |
any antigen capable of binding specifically to components of the immune system (BCR, Antibodies) |
|
|
T/F All immunogens are antigens? |
True |
|
|
T/F every antigen is an immunogen |
False: not all compounds that can be bound by antibody stimulate an immune response |
|
|
A compound that cannot induce an immune response by itself |
hapten Dyes found in your food are haptens, they’re small, not complex. |
|
|
When will lead Hapten to induce an immune response? |
If it is linked to or conjugated to a carrier molecule that is immunogenic this will lead to activation of the immune response |
|
|
Part of an antigen that combines with a specific antibody or T cell receptor(Antigenic determinant) |
epitope |
|
|
Hapten-carrier conjugates are _______ |
immunogenic |
|
|
Requirements for Immunogenicity |
Foreignness (more likely to be recognized) Molecular size (need a large molecular weight) Chemical Complexity (not being all the same thing) Degradability and Interaction with the host's MHC- has to do with T cell response. If you have an inability to break up that antigen you won’t get lymphocyte activation or t cell activation |
|
|
Because of self vs non self recognition, the more foreign the substance is, the more ______ it is |
immunogenic |
|
|
small substances are ______ immunogenic |
less most active immunogens have a molecular mass of 100,000 Da |
|
|
Chemical complexity _______ immunogenecity |
increases |
|
|
What are the most immunogenic of our macromolecules and why? |
proteins, because because theyr’e more complex. Leads to greater binding and more activation of lymphocytes overall |
|
|
How can we increase our chemical complexity? |
Can take a copolymer to add glu-ala-lys it is now immunogenic |
|
|
Macromolecules that cannot be degraded and processed by APCs and presented with MHCs are _____ immunogens |
poor
|
|
|
Antigen presentation is necessary to activate_____ |
t cells |
|
|
Tcells really only respond to protein. A good protein antigen is |
stable enough to reach the site of interaction with T or B cells Able to be enzymatically degraded by proteases of an APC |
|
|
Peptides of D-amino acids are not immunogenic, but L-isomers are. Why? |
We primarily have L isomers in our protein. Bacteria can be solely D isomers we will not be able to degrade them appropriately and will not illicit an immune response |
|
|
Carbohydrates can activate B cells, but don't activate T cells. T/F |
True. B cells can bind to anything |
|
|
There was a new study that suggests you can have an activation of T cells through carbohydrates. how? |
You can have breakdown of carbohydrate withinthe cell and load it onto mhc2 so you can present carbs to t cell |
|
|
How can genetics affect immunogenecity |
Species Individual Responders vs Non-responders Genotypeof individual influences whether a given compound will stimulate an immune response Differences in genes of the MHC .Individual repertoires of B and T cells Not every antigen-specific receptor is present |
|
|
How can dose affect immunogenecity? |
Dosage can be: Too low (not enough to activate lymphocytes) or Too high (inducing tolerance). Number of doses also affects outcome of the immune response |
|
|
Routes of administration for immunogenecity |
subcutaneous intravenous Intragastric Intranasal |
|
|
Subcutaneous route of administration |
breath through skin, carries antigen to neares lymphnode Elicitsstrong response due to potent antigen presenting ability of Langerhans cells |
|
|
Intravenous route of administration |
Antigens go to spleen, induce tolerance or induce response. |
|
|
Intragastric Route of Administration |
Antigens often produce systemic tolerance, but sometimes elicit local antibody response |
|
|
Intranasal Route of administration |
antigens often elicit allergic response |
|
|
binding of antigen to antibody or lymphocyte is _____ |
specific |
|
|
Immune cells do not recognize an entire immunogen molecule. What do they recognize? |
discrete sites on the macromolecule, Ie: epitopes, a single antigen may have numberous epitopes |
|
|
what are areas in the antigen binding pocket that give that whole specificity, these are regions of hyper variability. This gives specificity for that recognition |
Complementary determining regions (CDR) |
|
|
Antibody binds epitope based on the ____ _____ ____, formed from several hypervariable regions |
complementarity-determining region (CDR) |
|
|
Paratope is the same size as epitope? T/f |
True, paratope is a complementary antibody-combining site |
|
|
Paratope is the part of the antibody that binds to the ________on the antigen |
epitope |
|
|
The eptiope that binds the T cell receptor is how many amino acids? It is also functionally ______ because of noncovalent association with MHC proteins on MHC |
8-12 amino acids funcitonally larger |
|
|
Trimolecular complex forms when (t cell receptor) |
TCR binds MHC + epitope complexes |
|
|
B cells have _____ binding T cells need.... |
Direct Presentation by MHC and most commonly will be a peptide |
|
|
Antibody or TCR binds to antigen ______ |
noncovalently |
|
|
Noncovalent binding may involve |
electrostatic interactions hydrophobic interactions hydrogen bonds van der Waals forces |
|
|
Non covalent interactions are _____ so _____are required for good bonding |
weak many Interaction between antigen and its complementary site must cover enough area to maximize available interactions When we have this binding we’ll have a variety of non covalent bonds and ionic bondsas well. Themore specificity will have greater affinity because you’ll have more chemicalinteractions there. |
|
|
B cells can bind to both _____ and _______ epitopes whereas T cells can only recognize ____ |
linear and conformational (conformational is when the epitope is only formed when it is folded together, once it is unfolded the epitope goes away) linear |
|
|
______ Cells are able to only bind to that which is accessable/that which is exposed. Cannot recognize something inside of the cell. |
B |
|
|
_______ Cells can recognize things that are inside a cell because MHC1 presents it |
T cells |
|
|
______ cells have the ability to bind to soluble proteins and molecules (antigens) |
B |
|
|
When a B cell binds to that which is soluble it can precipitate it so that other cells can attack it t/f |
true |
|
|
Can T cells bind to soluble proteins? |
No, they can only bind to that which is presented. It has to be tangible |
|
|
Differences between antigen recognition by B and T cells Antigen interaction: Nature of Antigens: Binding of Soluble Antigens: Epitopes recognized: |
Antigen Intereaction: B cells- b cell receptor binds to antigen------ T cells- T cell receptor binds antigenic peptides bound to MHC Nature of Antigens: B cells- protein, polysaccharid, lipid------T cells- peptide Binding of soluble antigens? B cells yes ------ T cells no Epitopes recognized: B cells- accessible, sequential, nonsequential------ T cells, Internal linear peptides produced by antigen processing |
|
|
Proteins, polysaccharides, nucleic acids, lipids (some glycolipids and phospholipids can be immunogenic for T cells and ilicit a cell mediated immune response) are examples of the ___________ nature of immunogens |
chemical |
|
|
Some things when coupled with a carrier can become an immunogen. Provide examples |
drugs, haptens, food additives, cosmetics, antibiotics, small synthetic peptides |
|
|
Carbohydrates are a major chemical that may be antigenic and can induce _______ response in the absense of T cell help. ______ are more immunogenic when associated with protein or lipid carriers. ________ are usually immunogenic. ABO blood group reactions are based on _____ on RBCs |
can induce antibody response in absence of T cell help polysaccharides are more immunogenic when associated with protein or lipid carriers glycoprotiens are usually immunogenic ABO blood group reactions are based on polysaccharides on RBCs (if your given someone elses blood type then it will attack those foreign plasma cells) |
|
|
Same sugars alone are or are not immunogenc? |
They are not immunogenic |
|
|
Lipids can be antigens, but they are rarely immunogenic. How is the response induced? |
by binding lipids to protein carriers Glycolipids and sphinigolipids may also be immunogenic |
|
|
Nucleic acids are the _______ immunogenic of the categories |
least, They are poor immunogens unless conjugated to protein carriers |
|
|
Native helical DNA is normally immunogenic? T/f |
false |
|
|
immune responses to nucleic acid sometimes occur. Give an example of when? |
systemic lupus erythematosus (SLE) |
|
|
Proteins are virtually all immunogenic. why? |
The more complex proteins stimulate more vigorous immune responses. Proteins are large and complex and contain multiple epitopes |
|
|
Explain Cross reactivity |
Even though it is not the perfect antigen to bind to, it is similar enough to bind to start activation. This is great because we rely on it for vaccines since injecting the actual microbe can actually kill you |
|
|
2 different forms of cross reactivity |
homologous heterologous |
|
|
Homologous cross reactivity |
means the same. Using antigen from microbe for which you want protection -Example DTaP vaccine- we have diphtheria toxoid, tetanus toxoid, and Pertussis toxoid & other adhesins. Toxoid is the term that is used for an inactivated toxin. By inactivating these toxins and changing the structures it is not in its active form but will confer protection against that toxin if you come into contact with it- Example-flu vaccine |
|
|
Heterologous cross reactivity |
using something similar but different to protect against another organism- example: small pox vaccine- were using cowpox to protect against smallpox. Don’t actually inject smallpox but cowpox has Similar epitopes on the surface so if your body was to see smallpox you’d be protected against it. |
|
|
Cross reactive molecules may: |
share a source be unrelated to each other except for having common epitopes somewhere in their structures example: Blood group a and b can cross react with your blood type antigen when they get certain illnesses |
|
|
Substances that enhance an immune response to an antigen that has low immunogenicity Also used when only a small amount of antigen is available. used a lot in vaccines |
adjuvants |
|
|
adjuvants will make a hapten immunogenic t/f |
false. |
|
|
adjuvant mechanisms work by.... |
Increasing half-life of vaccine antigen Increasing cytokine production in local inflammation Improving antigen delivery, processing and presentation by APCs (esp. dendritic cells) |
|
|
The only adjuvant approved for the U.S. is Aluminum hydroxide and aluminum phosphate (alum). How does it work |
Alum as inorganic salt binds proteins, causes proteins to precipitate and elicit an inflammatory response, increases immunogenicity of the antigen nonspecifically, precipitated antigen is released more slowly at injection site, larger size due to precipitation, increases likelihood that it will be phagocytized
|
|
|
Freund’s complete adjuvant (FCA) is killed Mycobacterium tuberculosis or M. butyricume mulsified in oil with aqueous antigen solution. how does it work? |
Oil causes slower release of the protein Muramyl dipeptide activates dendritic cells and macrophages Activated cells are more phagocytic and express higher levels of the costimulation molecules for enhanced T cell response |
|
|
what is that adjuvant that contains antigen in aqueous solution, mineral oil, and an emulsifying agent that disperses the oil into small droplets around the antigen |
Freund’s incomplete adjuvant (FiCA) |
|
|
Alum and Freunds adjuvants stimulate local chronic inflammatory response and attracts phagocytes and lymphocytes. Infiltration of these cells may result in the formulation of a _____ |
granuloma because you have such a great response they start to wall off the antigen and now this is stuck in a hardened pocket. This causes a granuloma |
|
|
Explain the first exposure to an immunogen/primary response |
T cell activation B cell activation to make and secrete antibody -Long delay because you haven’t encountered it before. You have to become activated- Primary antibody that you will have is IgM which will be expressed then decrease as you fight the infection- What were relying on in vaccines |
|
|
Explain second exposure to the same immunogen/secondary response |
-Memory or Anamnestic response. -Reduced to no lag-Will have a lot more antibody because we have more cells becoming activated -We also see isotype switching to IgG. More IgG expressed than IgM-- |

