![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
Bacteria look almost the exact fuckln' same under a microscope... What can we use to CLASSIFY the different types of bacteria? (5 characteristics)
Why can't we just be lazy and use the GENOMIC ANALYSIS to identify which antibiotic to use for a patient? |
1. MICROSCOPIC CHARACTERISTICS (gram staining, etc)
2. COLONIAL CHARACTERISTICS (how they grow in media- color, shape, size, etc) 3. PHYSICAL/ BIOCHEMICAL PROPERTIES (growth requirements like carbon sources, etc) 4. CELL COMPONENTS (serological, biochemical tests) 5. GENOME ANALYSIS (increasingly popular, uses DNA to look for distinguishing char.) **It is important to remember that YOU CAN'T DO A FULL PROFILE OF ANTIBIOTIC SUSCEPTIBILITY FROM DNA alone- you need the VIABLE organisim to determine most of the characteristics above.** |
|
|
What are the different types of PHYSIOLOGICAL DETERMINANTS we need to know about a bacteria before we can culture it? (temp, acidity, air, micro/macronutrients, metabolisim)
|
1. TEMPATURE: Psychro-/ Meso-/Thermophiles
2. pH: aciduricity/ normal 3. GAS REQUIREMENTS: Obligate aerobes/ Microaerophilles/ Capnophiles/ Facultative/ Obligate anaerobes 4. TRACE ELEMENTS & VITAMINS: Prototrophs/ fastidious// auxotrophs/ opportunistic pathogens 5. CARBON SOURCE: autotroph/lithotroph //heterotroph/organotroph 6. NITROGEN SOURCE: NO3- reduction// N2 fixation/reduction 6. METABOLISIM: aerobic/ anaerobic/ fermentation |
|
|
What is the difference between microaerophiles and capnophiles?
|
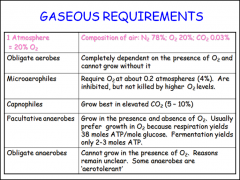
microaerophiles= need just a little bit of O2 to grow. It won't grow as well in higher oxygen
capnophiles= like higher CO2 (carbon dioxide) the best! |
|
|
There are two ways we can grow and test bacteria: we can plate it (solid media), or we can use a tube (liquid media).
Which one is better for mixed populations (poop, oral swab, skin etc.)? Why? Why isn't this necessary for sites like blood, CSF, synovial joints, etc? |
Solid media is better for MIXED cultures because it is TRICKIER TO ISOLATE the causative agents from the normal flora. Solid plates dilute and selectively grow bacteria to differentiate cultures
Liquid media is better for a SINGLE culture of bacteria. Infections in normally sterile areas of body mean that bacteria found=causitive agent |
|
|
What is bacteremia?
|
Bacteremia (also bacteraemia or bacteræmia) is the presence of bacteria in the blood. The blood is normally a sterile environment, so the detection of bacteria in the blood (most commonly accomplished by blood cultures) is always abnormal.
Bacteria can enter the bloodstream as a severe complication of infections (like pneumonia or meningitis), during surgery (especially when involving mucous membranes such as the gastrointestinal tract), or due to catheters and other foreign bodies entering the arteries or veins (including intravenous drug abuse). Bacteremia can have several consequences. The immune response to the bacteria can cause sepsis and septic shock, which has a relatively high mortality rate. Bacteria can also use the blood to spread to other parts of the body (which is called hematogenous spread), causing infections away from the original site of infection. Examples include endocarditis or osteomyelitis. Treatment is with antibiotics, and prevention with antibiotic prophylaxis can be given in situations where problems are to be expected. |
|
|
What are the different ways (4) we can MEASURE bacteria in a LIQUID media culture? Which one is most common?
|
1. DRY WEIGHT: μg/ml of culture
2. TOTAL PROTEIN: μg/ml of culture 3. VIABLE COUNT: c.f.u./ml of culture assumes that each colony is the progeny of a single cell (usually not true) 4. TURBIDITY: Optical density (OD) at a wavelength between 500 and 700 nm >106 cells/ml and the culture is visibly turbid |
|
|
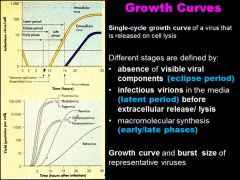
For the bacteria growth curve, what are the key features of each phase (4)?
Which one has the most intense metabolic activity but little cell division? Which phase is most susceptible to antibiotics? Which has the # of cells formed= # of cells dying? What about when # of cells dying > # of cells formed? |
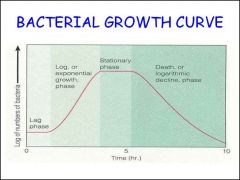
1. LAG PHASE: Increase in cell size but little or no cell division; Intense metabolic activity; Uptake of nutrients and macromolecular biosynthesis of, DNA, protein, etc.; Sensitivity to physical and chemical agents such as antibiotics; uniform staining with Gram’s stain
2. EXPONENTIAL (LOG) PHASE: Maximum growth rate; minimum generation time; balanced growth; cellular reproduction most active; most susceptible to uptake of foreign DNA; most susceptible to antimicrobial agents; uniform staining with Gram’s stain 3. STATIONARY PHASE: Growth rate slows; number of bacterial deaths equals number of new cells; metabolic rate slows; production of secondary metabolites, e.g., antibiotics, spores, inducible enzymes 4. DEATH PHASE: Number of deaths exceeds number of new cells formed; culture may die out, or a small fraction of the population may survive for a long time |
|
|
Explain why we need to dilute the bacteria for a mixed population growing on the agar plate.
|
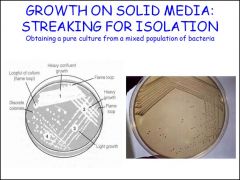
This is because ALL SECONDARY DETERMINITIVE TESTS MUST BE PERFORMED ON a single bacteria type. secondary (determinative) tests MUST be performed on bacterial cells obtained from WELL ISOLATED INDIVIDUAL colonies.
The object of the exercise is the progressive dilution of the bacteria until SINGLE bacterial cell are deposited on the surface of the agar. Each bacterial cell will divide to become a visible colony. EACH COLONY WILL BE A CLONAL POPULATION! |
|
|
What are the different advantages for the GENERAL PURPOSE media, DIFFERENTIAL/"Partially selective" media and SELECTIVE media types?
|
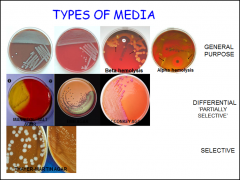
General purpose media: Blood agar and chocolate agar. These are nutritionally rich general purpose media that are used in the primary recovery of human pathogens. They each have advantages. Blood agar is an ‘indicator’ medium that reveals the production of hemolysins by bacteria by the lysis of the red blood cells (RBCs) in the medium. Hemolysins are exotoxins that are cytotoxic. Chocolate agar is more nutritious than blood agar because the RBCs are lysed and release cofactors such as NAD and hemin into the medium. Chocolate agar is used to recover fastidious human bacterial pathogens.
Differential and partly selective: These media are designed to favor the growth of certain groups of bacteria while inhibiting others. The two media commonly used in the clinical laboratory are mannitol-salt agar and MacConkey agar. Mannitol-salt agar is designed for the recovery of staphylococci from the skin. Sodium chloride (7.5%) is the selective agent and the sugar alcohol mannitol is the differentiating component. The indicator is the pH indicator phenol red. Staphylocooci can withstand high levels of salt whereas few other bacteria can. In addition, S. aureus ferments mannitol readily whereas other species of staphylococci do not. Acid produced by S. aureus colonies turns phenol red to yellow so that colonies turn yellow and there is a yellow halo in the agar around each colony. Other species of staphylococci do not produce sufficient acid from mannitol to change the color of the colonies or agar. Selective media: The only selective medium rountinely used in the clinical laboratory is Thayer-Martin agar which is used to isolate Neisseria gonorrhoeae and N. meningitidis when the clinical specimens are taken from the skin or mucosae. Consisting of chocolate agar with vancomycin, colistin and nystatin, it is formulated to minimize the overgrowth of gonococci and meningococci by contaminants, to suppress the growth of saprophytic Neisseria species and to enhance the growth of pathogenic Neisseria. |
|
|
How do gram stains work? What are the 4 ingredients/ 4 steps needed? Which one is the most important?
|
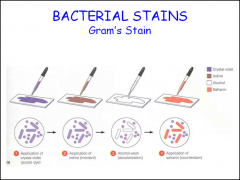
The way it works is the differential effect on the ALCOHOL on the gram (+) and gram (-) cell wall.
For the gram-positive cell wall the peptidoglycan matrix is dehydrated by the alcohol so that its pores are small trapping the complex of the crystal violet and Lugol’s iodine. In contrast alcohol increases the permeability of the gram-negative cell wall so that the crystal violet-Lugol’s iodine complex is released. |
|
|
Why can't we use gram stains for the gram (+) MYCOBACTERIUM? What test do we need to use instead?
|
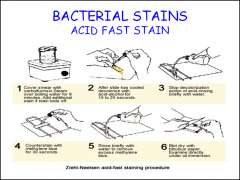
The cell wall of Mycobacterium is so HYDROPHOBIC (with mycolic acids) that it resists staining by grams method. We use the ACID FAST STAIN.
CARBOLFUSCHIAN= stains mycobacterium METHELYNE BLUE= counterstains everything else |
|
|
What do coccus bacteria look like?
What do bacillus bacteria look like? |
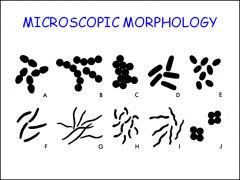
Coccus= sphere
Bacillus= rod |
|
|
When you are doing an ACID FAST STAIN, what do the MYCOBACTERIA look like?
|
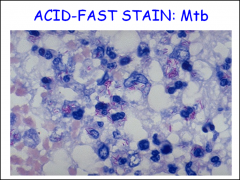
Mycobateria (like M. tuberculosis an M. Leprae) appear as RED BEADED DOTS (carbolfuschian) on a BLUE BACKGROUND (methylene blue) .
|
|
|
For the ENTEROBACTERIA family (like samonella or e.coli), what color would they appear on a gram stain (+ or -)? What category of tests would help to further identify the different types from the MIXED pathogens?
|
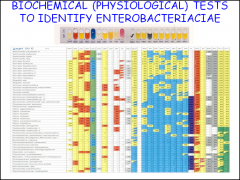
Pink= GRAM NEGATIVE (-)
BIOCHEMICAL TESTS (physiological) help id different bacterium. substrates--> various enzyme activities sugars--) fermentation patterns |
|
|
What is the difference between MacConkey agar and MacConkey-sorbital agar? Which type of e. coli (commensal or pathogenic) can ferment sorbitol?
What color would it appear as on a gram stain? What shape is e.coli? |

MacConkey tests fermentation of LACTOSE (LAC+ =pink LAC- = white)
MacConkey-Sorbitol tests fermentation of SORBITOL (Sorb+= pink Sorb- = white) ***Pathogenic (0157:H7) E. coli CANNOT FERMENT SORBITOL (gray) E.coli= gram - rods. |
|
|
Bacteria that are grow in fluid are very different than the ones growing in nature called BIOFILM communities. How is growth of bacteria in BIOFILM different from fluid growth?
|
Bacterial communities are termed biofilms, and cells growing in biofilms are different from those growing in fluid (planktonic growth). For example, biofilm bacteria grow slower, they may use different methabiloic pathways and they are more antibiotic resistant. There is also greater opportunity for horizontal gene transfer.
|
|
|
Where do biofilms love to grow?
|
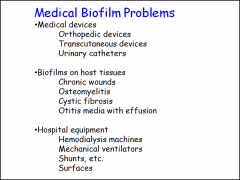
Non-shedding surfaces.
|
|
|
What are the key differences between prokaryotes and eukaryotes?
|

The prokaryotes have a unique CELL WALL made of PEPTIDOGLYCAN not shared with the eukaryotes. Furthermore, prokaryotes LACK CHOLESTEROL in the cell MEMBRANE. The ONLY ORGANELLE IS RIBOSOME in the cytosol of prokaryotes is the ribosome and even here it is structurally different from the ribosomes of eukaryotes (70s vs. 80s in eukaryotes)
|
|
|
Bacteria have lots of ways to avoid our immune system and causing havoc in our bodies. What are the actual features of bacteria that can make them so dangerous (virulent) to humans? (7 things that make them virulent/ pathogenic to humans) How does their structure relate to these fxns?
|
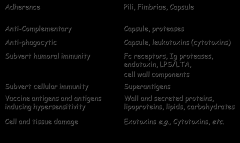
1.ADHERENCE- pili, fimbrae, capsule
2. ANTI-COMPLEMENTARY- capsule, proteases 3. ANTI-PHAGOCYTIC- capsule, leukotoxins/ cytotoxins 4. SUBVERT HUMERAL IMMUNITY- Fc receptors, Ig proteases, enotoxins, LPS/LTA, cell wall components 5. SUBVERT HUMERAL IMMUNITY- superantigens 6. VACCINE ANTIGENS & ANTIGEN INDUCED HYPERSENSITIVITY- wall and secreted proteins, lipoprotiens, lipids, carbs 7. CELL AND TISSUE DAMAGE- exotoxins ie. cytotoxins |
|
|
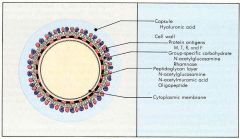
What is the very diverse "slimey" part of bacteria may be the true virulence factor? The "K antigen"?
Hint- this part is the vaccine anigen for pneumococcus, meningiococcus and haemophilus influenzae type b vaccines? |
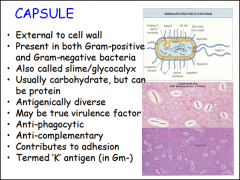
The CAPSULE
|
|
|
In bacteria, which are the organs driven by proton motive forces, that can also contribute to their virulence by swimming around to different barriers??
Hint- the "H antigen" |
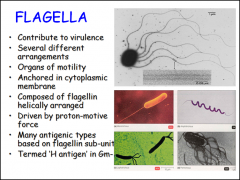
The FLAGELLA
|
|
|
In both GM+ *AND* GM- bacteria, what are the principle organs of host-tissue ADHESION, biofilm formation, co-aggregation, immunomodulation?
|

FIMBRAE & PILLI
via lectin or protien-protien interactions * antigenic variation make it diffidult to be caught be adaptive immune system In BOTH GM+ and GM- |
|
|
The peptidoglycan structure of bacterial cells walls help to protect the delicate cytoplasmic membrane in both gram + an.d - bacteria (but much thicker in gram +). What are the 5 general principles of petidoglycan structures?
hint- 1. What does the backbone consist of? 2. How are they linked? 3. What type amino acid isomers do they have? 4. What are the 1st, 3rd and 4th type of amino acid? |
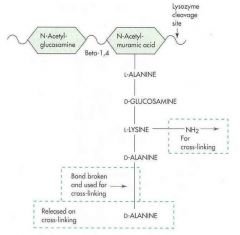
Backbone consists of glycan chains of the disaccharide N-acetylmuramic acid (NAM) - N-acetylglucosamine (NAG)
Chains are linked via TETRAPEPTIDES attached to N-acetylmuramic acid Tetrapeptides consist of alternating L- and D- amino acids First and fourth amino acids are alanine The third amino acid is always a di-amino acid e.g., lysine, diaminopimelic acid, etc. |
|
|
What SPECIFIC KEY FEATURE is essential for the biosynthesis of the cell wall structure in bacteria?
|
BACTOPRENOL- like building a space station from earth, bactoprenol transports PEPTIDOGLYCAN monomers across CYTOPLASMIC MEMBRANE and helps insert it into growing peptidoglycan chains outside.
NAM assembled in cytoplasm, |
|
|
Spore formation only happens in gram ______ cells. Why is this?
|
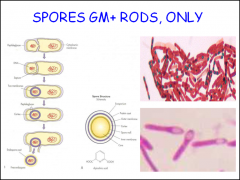
GM+ rods only
Spore formation is a property of some gram-positive bacilli such as Bacillus and Clostridium. The process is initiated by nutrient limitation, frequently of the amino acid alanine. Bacteria produce a single endospore internally. The spore is sometimes surrounded by a thin covering known as the exosporium, which overlies the spore coat. The spore coat, which acts like a sieve that excludes large toxic molecules like lysozyme, is resistant to many toxic molecules and may also contain enzymes that are involved in germination. The cortex lies beneath the spore coat and consists of peptidoglycan. The core wall lies beneath the cortex and surrounds the protoplast or core of the endospore. The core contains the spore chromosomal DNA which is encased in chromatin-like proteins known as SASPs (small acid-soluble spore proteins), that protect the spore DNA from UV radiation and heat. The core also contains normal cell structures, such as ribosomes and other enzymes, but is not metabolically active. Up to 20% of the dry weight of the endospore consists of calcium dipicolinate within the core, which is thought to stabilize the DNA. Dipicolinic acid could be responsible for the heat resistance of the spore, and calcium may aid in resistance to heat and oxidizing agents. |
|
|
What are the methods(3) of horizontal gene transfer (HGT)?
|
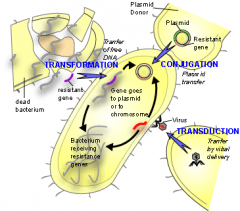
1. TRANSFORMATION= uptake of NAKED DNA from the environment
2. TRANSDUCTION=transfer of bacterial genetic material by a BACTERIOPHAGE. 3. CONJUGATION= direct CELL TO CELL CONTACT and a PLASMID. |
|
|
What are genomic islands?
|

|
|
|
Describe streptococcus.
Are they GM +/-? Catalase test? +/- Rods or cocci? Gaseous enviorment? Where are they found commensually? What TEST can we do to differentiate species? |
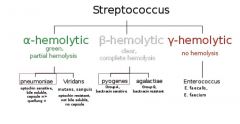
GM+ cocci (purple), catalase -, canophillic, found in mucosa,
Hemolytic features differ! Blood agar |
|
|
Out of the different Streptococcal species, which one causes upper respiratory tract infections? Lower respiratory infections?
Bonus*What would they look like plated on blood agar? Hint** its either S. pyogenes or Streptococcal pneumonia? |
Strep pyogenes for upper= β hemolytic/clear
strep pneumoniae= lower= α hemolytic/ green |
|
|
Describe the 4 types of groups of strep based on hemolytic classification.
|
s. pyogenic group- β puss producing
viridans group- α hemolysis enterococcus group- γ live in large bowel lactic group- make CHEESE |
|
|
What are the "C" polysaccharides antigens? Where are they located on bacteria? How can we use this antigen to classify the β-hemolytic streptococci?
|
LANCEFIELD SYSTEM:
The "C polysaccharide"= teichoic acid covalently attached to cell wall in GM + Group A,B,C,D ... etc.... S. pyogenes= GROUP A STREP (GAS) |
|
|
When you go to the doctor's office to make sure you don't have strep throat (aka. STREPTOCOCCAL PHARYNGITIS), what type of test do they use to classify the culture?
|
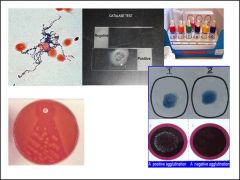
Lancefield Group A typing serum: LATEX AGGLUTINATION TEST
To test for streptococcal PYOGENES Rapid test: throat swab--> antigens from organisims in throat extracted-->latex--> + agglutination = GAS |
|
|
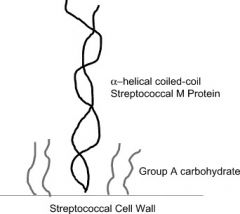
What is the most important virulence factor in streptoccocus pyrogenes (GAS)? Why? Also, how does the immune system respond to the many different types of this specific virulence factor--> How does this contribute to the difficultly in adaptive immune response?
Bonus* since there are so many different strains of antigens... what can we use to test for a marker of after GAS infection? |
the M PROTIEN (adhesion,antiphagocytic--> degrades C3b--> important for OPSONIZATION)
Immunity for GAS is M-TYPE SPECIFIC! (There are 90 different types) *Bonus ?:* presence of STREPTOLYSIN O is a marker after GAS infection |
|
|
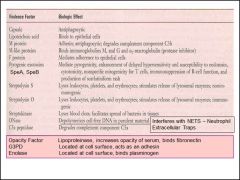
VERY IMPORTANT:: What about the the composition of GAS (pyogenes) contribute to its virulence?
|
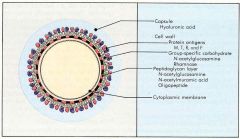
*capsule of HYALURONIC ACID--> POORLY IMMUNOGENIC
*M-PROTIEN--> degrades C3b (antiphagocytic) *M-LIKE PROTIENS--> look like Fc receptors, capture Ig(M,G) * STREPTOLYSIN O & A--> Cytotoxic * C5a PEPTIDASE--> destroy important CHEMOTATIC factor of complement *LIPOTECHOIC ACID, FIBRONECTIN BINDING PROTIEN, (ENOLASE, G3PDH)--> adherence to host tissue *STREPTOKINASE--> lyses blood clots,bacteria can spread farther |
|
|
AGAIN, VERY IMPORTANT!!
Name the different virulence factors of Group A Strep (GAS) that make it one badass motherfucka |
|
|
|
1.) With all the different virulence factors of GAS, what type of PATHOGENISIS can this produce in our bodies?
2.) What are the different M types assosciated with certain diseseases? |
Diseases resulting from local infection with GAS and their products
Diseases resulting from invasion of GAS Infective endocarditis Post-streptococcal disease TOXIC SHOCK/ NECROTIZING FASCIITIS: M1, 3, 5 RHEUMATIC FEVER: M3,5,18,19,24 (S. pyoderma) IMPETIGO/ GLOMERULONEPHRITIS: M49, 57,59-61 |
|
|
Exam question: Which type of hepatitis does not have ANY deaths from CHRONIC infection?
Aka. which type of hepatitis only has ACUTE infections?? Which Ig type (antibody) would you see with an active ACUTE infection? |
Hepatitis type A (HAV) only has acute infections (6-9 months and then it will go away)
IgM (anti- HAV) would indicate a current/ recent infection |
|
|
All the Hepatitis Viruses are very different from one another. Some DNA/ some RNA etc.... WHAT DO THEY ALL HAVE IN COMMON? WHAT IS A SINGLE DEFINING FEATUERE OF THE HEPATITIS VIRUS?
|
The Hepatitis Virus ONLY infects the LIVER
|
|
|
Which hepatitis types can you get vaccines for? Why not all of them?
Hint* A+B both have vaccines. What is it about the C virus that make it useless to make a vaccine. |
Hepatitis C virus (HCV) does not have a vaccine!
B/c it is an RNA VIRUS. (Unlike HAV and HBV which are both stable DNA virus types) -no protective immunity -RNA polymerase= no proofreading / high mutations - mutation too frequent-- antibodies are useless |
|
|
Someone comes in that you suspect may have Heptitis type A (HAV). What might they look like and how would you diagnose it?
|
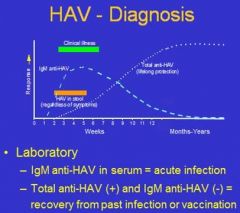
Clinical
i. Symptoms of actute hepatitis • not specific for HAV vs. other hepatitides • not always present ii. Patient history / social factors • Travel to endemic area • part of an outbreak Laboratory Diagnosis i. Tests for IgM and total anti-HAV antibodies • IgM anti-HAV (+) = acute HAV infection • IgM (-) + total anti-HAV (+) = past HAV infection or vaccination |
|
|
A patient comes in that you suspect may have Hep B virus. Which antigen/ antibodies would you use to diagnose for it (acute vs. chronic)? How do they symptoms present?
|
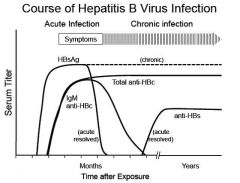
Diagnosis
Clinical: Symptoms of hepatitis • not specific for HBV vs. other hepatitides • not always present vi. Assess patient history for risk factors • HBV status of mother • Exposure (IV drug use, HBV-pos. sex partner) b. Laboratory Diagnosis of HBV infection requires analysis of more than one serum marker in order to differentiate current acute infection, previous resolved infection, chronic infection, and possibly vaccination status. The markers used and their utilities are as follows: • HBsAg (hepatitis B surface antigen) – the virus envelope protein – indicates presence of virus (acute or chronic infection) • anti-HBc (total antibody to the HBV core protein) – indicates current or past infection. (Antibody to the virus core protein (HBc) can coexist with chronic infection because this antibody does not bind to whole virus particles – the core protein is sequestered inside). • IgM anti-HBc (IgM antibody to the HBV core protein) – indicates current acute infection • anti-HBs (antibody to the hepatitis B surface antigen) – protective antibody generated following resolution of infection and by the HBV vaccine • HBe / anti-HBe (hepatitis B “e antigen”/antibody to hepatitis B e antigen) – mutually exclusive markers can be useful for assessing status of chronic infection (HBe pos = high levels of virus; anti-HBe = low levels of virus) |
|
|
When testing for Hepatitis B virus (HBV), how could you determine if the infection was acute or chronic?
• HBsAg • anti-HBc • IgM anti-HBc • anti-HBs • HBe / anti-HBe |
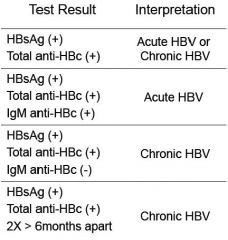
If we have the ANTIGENS for HBsAG and ANTIBODIES for the HB capsule antigen= (+) diagnosis for HepB.
**Again, when IgM present= ACUTE INFECTION*** Clear differential |
|
|
What the F*ck is the difference between HBsAg and HBcAg? And why the F*ck do we care?
(Hepatitis B SOLUBLE Antigen and Hepatitis B CAPSULE Antigen) |

Surface protien (Anti-HBs Ig is protective)
Core protein (Anti-HBc Ig is NOT protective) |
|
|
Describe differences between GM+ and GM- bacteria. Which stains purple/pink? Which one has teichoic acids? "O antigens"? Thick peptidoglycan layer? Periplasmic space?
|

GM+:
thick peptidoglycan teichoic/lipotechoic GM-: periplasmic space "O antigen" carbohydrate bilayer membrane |
|
|
Thinking purely about structure, Which type of bacteria have 90% of their dry weight as PEPTIDOGLYCAN ? Which one have the Lipopolysacharide (LPS) PAMP?
|
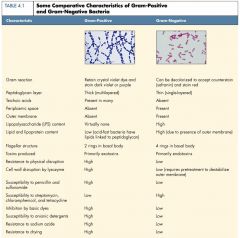
Gram+: 90% dry weight peptidoglycan
Gram -: has LPS |
|
|
How can we tell the difference between a bacteria and a virus? Which one do you need an ELECTRON MICROSCOPE to see?
95% of laryngitis are VIRAL infections! Why wouldn't an antibiotic work? |
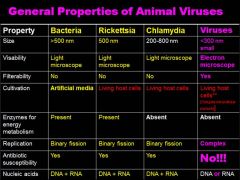
Animal Viruses: >300nm, viruses have FILTERABILITY because they are so small, viruses are NOT SUCEPTIBLE to antibiotics!! (duh) Not subject to the same replication patterns
|
|
|
What is the smallest virus? What property do all the small viruses have in common? How about smallest bacteria?
|
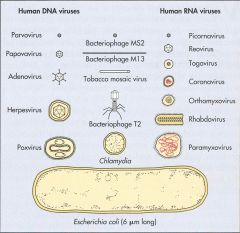
The small viruses do NOT HAVE ENVELOPES!
|
|
|
What are all the Human DNA viruses?
(smallest to largest) |
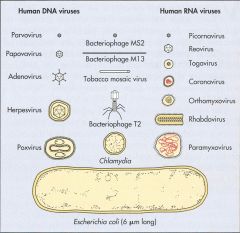
Parvoviridae
Papoviridae Hepadnaviridae Adenoviridae Herpesviridae Poxviridae |
|
|
Don't mess up CHICKEN POX and SMALL POX!!! Two different VIRUS types.
Which one is the POXVIRIDAE? What do they have in common? |

Small pox= Poxviridae
Chicken pox= herpesviradae (HHV3/ Varicella-zoster virus) *both linear dsDNA, both large and enveloped |
|
|
So viruses can come in all shapes and forms in nature: NAKED or ENVELOPED (bud off animal cells)
Different capsid assemblies: ICOSAHEDRAL or HELICAL shape But, what is one morphology that will NEVER BE SEEN IN HUMAN/ MAMMALIAN VIRUSES? |
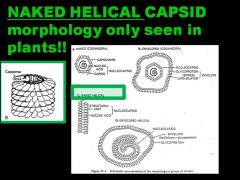
|
|
|
What is it about the RNA viruses that makes it so difficult to find a cure (HIV, Hep C)? Why is their genome type important? What extra tools do they need to have to replicate?
|
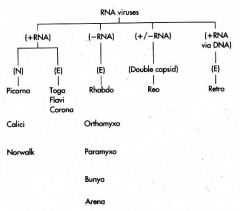
RNA viruses are very prone to mutation!
Cells cannot replicate RNA. RNA viruses must encode an RNA-dependent RNA polymerase The genome structure and polarity determine how viral mRNA is generated and proteins are processed RNA viruses, except (+)RNA genome, must carry polymerase Reoviruses (+/–) segmented DS RNA genome is template for mRNA. (+)RNA may also be encapsulated to generate the (+/–)RNA and then more mRNA Retroviruses (HIV) (+) retrovirus RNA genome is converted into DNA, which is integrated into the host chromatin and transcribed as a cellular gene Picornaviruses, Togaviruses, Flaviviruses, Caliciviruses, and Coronaviruses (+)RNA genome resembles mRNA and is translated into a polyprotein, which is proteolyzed. (–)RNA template is used for replication Orthomyxoviruses, Paramyxoviruses, Rhabdoviruses, Filoviruses, and Bunyaviruses (–)RNA genome is a template for individual mRNAs, but full length (+)RNA template required for replication |
|
|
Why is the capsule of the VIRUS so critical in determining the virus's ability to infect?
|
Attachment proteins and receptors are specific for certain viruses; without the proper combination, viruses cannot infect cells OR replicate
The viral envelope (if present) is removed during attachment and penetration A virus cannot be replicated if the capsid is not removed The receptors and attachment proteins are highly specific to certain viruses, the viral envelope is removed during attachment and penetration, and if the capsid is not removed, the virus will not replicate |
|
|
Viral phages can release new phage particles when they infect and BURST out of the cell like a motherfuc*er during LYTIC infection, and can VARY in the size of their progeny release.
Why is that? What factors/ length of different stages may cause the burst size to vary in the LYTIC infection? |
Both the type of virus can affect the burst size. and the length of the eclipse periods + latent periods can vary the amount of virus being made.
|
|
|
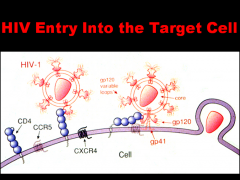
Retroviruses (RNA virus type) are freaking SCARY. We have the ONCOVIRINAE family that can cause CANCER (transforming virus) and then the LENTIVIRINAE family which is HIV (slow but certain death via immunosuppresion, cylindrical nucleocapsid).
WHY ARE RETROVIRUSES SO DAMN SCARY?! (And incurable) Also, what is the difference between a simple and complex retrovirus? What three elements do we need for this virus to be expressed? |

This provirus INTEGRATES randomly INTO THE HOST CHROMOSOME and becomes a cellular gene!!!
SIMPLE RETROVIRUSES encode gag, pol, and env genes COMPLEX RETROVIRUSES also encode accessory genes (e.g., tat, rev, nef, vif, vpu for HIV) RNA-dependent DNA polymerase (reverse transcriptase) and INTEGRASE enzymes are carried in the virion-- Virus enveloped spherical virion containing two copies of the positive-strand RNA genome Replication proceeds through a DNA intermediate, termed the provirus Transcription of the genome is regulated by the interaction of host transcription factors with promoter and enhancer elements in the long-terminal repeat (ltr) portion of the genome Virus assembles and buds from the plasma membrane Final morphogenesis of HIV requires protease cleavage of gag and gag-pol polypeptides after envelopement |
|
|
If you suspect a patient may have herpes, what sort of lab test would you use to diagnose? What would you say if the test was negative?
|
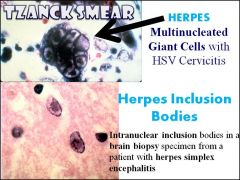
"Tzanck God I don't have herpes."
"Herpes is for life" Use the TZANCK smear to look for MULTINUCLEATED GIANT CELLS or INCLUSION BODIES |
|
|
So... herpes is your basic dsDNA virus, with a core, ICOSADELTAHEDRAL capsid, TEGUMENT, and envelope with glycoprotiens...but it can present in many different virus types, alpha, beta, and gamma (HHV 1-8) describe the different general features of each category.
|

|
|
|
"Herpes is for life"
- Maddie lee Why? Also, what about the mechanism of infection cause the symptoms? Which immune response (humoral or cell- mediated) are the most important for fighting a herpes infection? Why? |
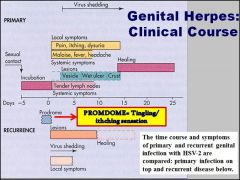
Once exposed to herpes, even though you may be asymptomatic, doesn't mean it infection wont reoccur in same site, reinfect a NEW site, or still be able to transmit the disease to others.
The diesase is spread via SYNCYTIA (cell to cell). During reexposure, viruses hide in cells, so antibodies (B cells) not very effective. CELL MEDIATED (T-CELLS) IMMUNITY IS REQUIRED FOR CONTROL. Virus is reactivated by stress. |
|
|
Viruses can jump from animal reservoir hosts in to humans, and then MUTATE (genetic changes occur) to efficiently become more infectious.... What do we call these types of viruses that jump from animals to human? What kind of animal sources do we seem them from?
|
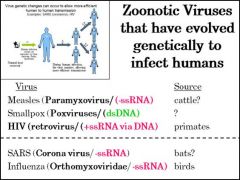
All sort of flavors of Zoonotic viruses
|
|
|
What is the difference between a HOST and a NATURAL HOST RESERVOIR for a disease with very little human to human transmission?
Bonus* what could happen if there is a mutation? |
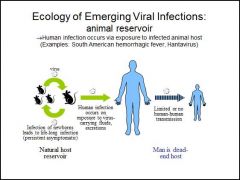
Host reservoir = life long infection (persistent asymptomatic)
with mutation, we could have more effective human to human transmission (like in a hospital/ nosocomial) and/or symptoms = more severe disease |

