![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
107 Cards in this Set
- Front
- Back
|
____ is the term for generalized edema
|
anasarca
|
|
|
anasarca
|
generalized edema
|
|
|
seroma vs cyst
|
seroma
- focal pocket of fluid accumulation (usually in subcutis) - usually due to trauma cyst - fluid filled cavity lined by epithelium |
|
|
define ascites
|
watery fluid in abdominal cavity
|
|
|
watery fluid in throacic cavity (pleural effusion)
|
hydrothorax
|
|

|
seroma
|
|
|
what does pulmonary edema look like
|
gross
- tracheal froth - interlobar edema microscopic - fluid is within alveoli |
|
|
3 types of SQ edema
|
dependent edema
- due to gravity bottle jaw - intermandibular edema in grazing ruminants pitting edema - indicates slightly longer duration |
|
|
what is edema
|
accumulation of excess watery fluid in the interstitial space or body cavities
|
|
|
what are the types of localized edema (6)
|
SQ
- dependent - intermandibular - pitting pulmonary hydropericardium hydrothorax ascites seroma |
|
|
inflammatory vs noninflammatory edema
|
inflammatory
- due to increased vascular permeability noninflammatory - results from circulatory disturbance |
|
|
what factors affect the development of non-inflammatory edema
|
hydrostatic pressure
- controlled by circulatory system fxn oncotic pressure - determined by solutes in plasma (esp albumin) lymphatic drainage |
|
|
true or false
anemia is a cause of edema |
false
|
|
|
what conditions result in noninflammatory edema
|
increased hydrostatic pressure
- decreased cardiac output (CHF) - impaired venous return (vein obstructed by thrombus or direct pressure) decreased oncotic pressure of plasma - excess loss of proteins (protein losing nepropathy or enteropathy, parasites) - decreased synthesis of proteins (severe dz or malnutrition) lymphatic obstruction - by trauma, neoplasia, parasites, or direct pressure |
|
|
hyperemia
|
ACTIVE dilation of arterioles to increase blood flow to an area or tissue by release of vasoactive chemicals such as histamine by neurogenic means
affected tissue is red b/c blood is oxygenated physiologic - blushing - exercise induced hyperemia of musc - hyperemia of gi tract after eating pathologic - increased blood flow during acute inflammation |
|
|
congestion
|
PASSIVE dilation of vessels (usually veins and capillary beds) due to decreased cardiac output and back up of blood into veins
affected tissue is dark red b/c venous blood has low oxygen due to increased hydrostatic pressure - often occurs with edema |
|
|
examples of congestion
|
pulmonary
hepatic hypostatic torsion of viscus barbituate effect on spleen |
|
|
how do barbituates result in congestion
|
cause relaxation of smooth muscle trabeculae & capsule of spleen
|
|
|
pulmonary congestion
|
capillary congestion pushes RBC into alveoli (diapedesis)
RBC engulfed by alveolar macrophages and digested into hemosiderin (brown) hemosiderin laden macrophages in the lung = heart failure cells |
|
|
what are "heart failure cells"
|
hemosiderin laden macrophages in the lung
|
|
|
hepatic congestion
|
acute
- high protein fluid exudes through the capsule of the liver - fibrinogen is converted to fibrin - acutely congested liver will be enlarged +/- fibrin on the surface chronic - blood accumulates in centrilobar sinusoids resulting in a reticular pattern grossly - congested (darker) centrilobar areaas and (lighter) portal areas = nutmeg liver a congested liver will be heavier than normal |
|
|
nutmeg liver is associated with
|
chronic hepatic congestion
|
|
|
hypostatic congestion
|
gravity pulls blood to down side of body
clinical relevance - lungs during anesthesia - color differences in organs postmortem |
|
|
torsion of viscus
|
veins more congested than arteries
|
|
|
what is hemorrhage
|
escape of blood from the cardio sys of a living organism
|
|
|
3 possible destinations of hemorrhage
|
the outside world
- epistaxis - hematemesis - hemoptysis - hematochezia - melena into a body cavity - hemoperitoneum (hemoabd) - hemothorax - hemopericardium (cardiac tamponade) into tissue - hematoma (3D extravascular clot) - venipuncture - trauma - splenic (at sites of lymphoid nodular hyperplasia) |
|
|
cardiac tamponade
|
cardiac dysfxn due to fluid in the pericardium compressing the heart
|
|
|
hematoma
|
3 dimensional extravascular clot
|
|
|
splenic hematoma
|
occurs at sites of lymphoid nodular hyperplasia
can rupture resulting in hemoabd can organize into firmer fibrous tissue impossible to tell from neoplasia |
|
|
descriptive terms for type of hemorrhage
|
petechial hemorrhages (petechiae)
- pinpoint to 2 mm foci ecchymotic hemorrhages (ecchymoses) - 3mm to 3 cm foci paintbrush hemorrhage - linear streaks |
|
|
3 mm to 3 cm foci of hemorrhage
|
ecchymotic hemorrhages
ecchymoses |
|
|
linear streaks of hemorrhage
|
paint-brush hemorrhages
|
|
|
pinpoint to 2 mm foci of hemorrhage
|
petechial hemorrhage
|
|
|
what 3 factors determine the effect of hemorrhage on the organism
|
location
- brain - spinal cord - pericardial sac rate - rapid loss is more often fatal - organism can compensate for slow loss quanitity - loss of 30% of total volume leads to shock |
|
|
what is shock
|
severe systemic hypoperfusion
|
|
|
4 categories of shock
|
cardiogenic
- failure of heart to pump blood hypovolemic - loss of blood or plasma volume anaphylactic - vasodilation due to IgE mediated hypersens rxn septic - systemic bact/ fungal infection |
|
|
linear streaks of hemorrhage
|
paint-brush hemorrhages
|
|
|
pinpoint to 2 mm foci of hemorrhage
|
petechial hemorrhage
|
|
|
what 3 factors determine the effect of hemorrhage on the organism
|
location
- brain - spinal cord - pericardial sac rate - rapid loss is more often fatal - organism can compensate for slow loss quanitity - loss of 30% of total volume leads to shock |
|
|
what is shock
|
severe systemic hypoperfusion
|
|
|
4 categories of shock
|
cardiogenic
- failure of heart to pump blood hypovolemic - loss of blood or plasma volume anaphylactic - vasodilation due to IgE mediated hypersens rxn septic - systemic bact/ fungal infection |
|
|
pathogenesis of septic (endotoxic) shock
|
infectious agent gains access to blood stream
endotoxins (LPS released when bact lysed) LPS activates endothelial cells, monocytes, and complement activated cells release cytokines (TNF and IL-1) circulating cytokines result in - systemic vasodilation and reduced myocardial fxn (hypotension) - widespread endothelial inj (ARDS/ SIRS) - activation of coag cascade (DIC) septiic shocl is often the cause of death in parvo and equine colic b/c gram neg bact enter blood through damaged GI mucosa |
|
|
thrombosis
|
coag of blood within intact cardio sys
|
|
|
thrombus
|
an IV pathologic mass of coag blood
|
|
|
4 steps of blood coag
|
vasoconstriction (brief)
platelet rxn (requires VWF) coag cascade (final prod is fibrin) anticoagulant mechanisms - antithrombin III (inhibits several clotting factors) - thrombomodulin - protein C - plasminogen activators |
|
|
what are the characteristics of ideal hemostasis
|
clot forms quickly (but only when needed)
becomes only as large as needed to plug defect remains localized to area of damage dissolves when no longer needed |
|
|
coag at site of vessel puncture
|
clot
|
|
|
pathologic coag within an intact vessel
|
thrombus
|
|
|
coag postmortem
|
clot
|
|
|
what is virchow's triad
|
3 factors predisposing to thrombus
endothelial inj (phys or fxnal) alterations in normal blood flow increased blood coagulability |
|
|
virchow's triad
endothelial inj |
physical or fxnal
trauma parasites (migrating strongyle larvae in horses/ canine heartworms) atherosclerosis (intimal fatty plaques) arteriosclerosis (mural fibrosis or mineralization, often secondary to age) systemic/ local inflammation (cytokines in circulation) |
|
|
virchow's triad
alterations in normal blood flow |
mechanisms
- loss of laminar blood flow allows platelets to contact endothelium - clotting factors and their inhibitors cannot interact normally - activation of endothelial cells turbulence - cardiac dysfxn or anomaly - cardiac IV cath - aneurysm stasis - inactivity (normal fxn of fibrinolytic sys req blood flow) - DVT |
|
|
Virchow's triad
increased blood coagulability |
corticosteroids
- inhibit plasminogen activators => reduced fibrinolysis protein losing nephropathy/ enteropathy - loss of antithrombin III pancreatitis - circulating enzymes activate coag cascade dehydration - hyperviscosity hormones - estrogenic and androgenic steroid hormones |
|
|
true or false
pancreatic hemorrhage is usually not significant |
true
|
|
|
embolus
|
an IV mass carried by bloodstream to a site distant from origin
most emboli derived from thrombi can get fat emboli with severe bone frx fibrocartilaginous emboli tumor emboli gas emboli (scuba) |
|
|
morphology of thrombi
|
microscopically
- alternating layers of fibrin, platelets (invisible), and erythrocytes (lines of Zahn) - form at sites of blood flow (not present in postmortem clots) grossly - chicken fat clot (postmortem clot in which serum and rbc have separated) - normal in horses due to rapid rbc sedimentation |
|
|
thrombus vs postmortem clot
consistency surface texture relationship to vessel color |
thrombus
- firm - rough - +/- attached to vessel - tan-red (higher proportion of fibrin to RBC) postmortem clot - soft/gelatinous - smooth/glistening - not attached - red-black |
|
|
fate of thrombi
|
dissolution
- fibrinolytic factors remove (recent small) thrombi propagation - continued enlargement resulting in vessel occulusion embolization - entire thrombus or portions may dislodge and travel to other sites organization - ingrowth of fibroblasts and smooth musc cells recanalization - formation of endothelium lined channels to allow blood through or around it |
|
|
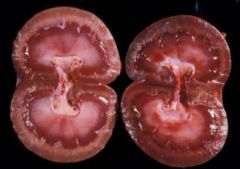
clinical implications of infarct
|
regional area of ischemic necrosis caused by blood flow obstruction
susc organs kidney - often wedge or fan shaped spleen - often venous and raised (congested) heart - sm area can lead to arrhythmia and death brain - sm area has big consequences skin - uncommon but striking (erysipelas) intestines - strongyle larvae lesion in horses resis organs (dual blood supply) liver lung - pulmonary and bronchial arteries |
|
|
clinical implications of pulm thrombi
|
obstruction of pulmonary arteries stops oxygenation of blood and results in hypoxia
lungs radiographically and grossly normal animal exhibits tachypnea with decreased spO2 thrombi in pulm arteries don't result in infarct b/c of dual supply originate w/in pulm arteries in animals (not legs) PTE - not correct in animals |
|
|
clinical implications/ pathogenesis of saddle thromboemboli
|
in cats
cardiac dysfxn => left atrial dilation => turbulence => formation of left atrial thrombi =>dislodge from heart => lodge at iliac bifurcation => cat presents w/ nonfxnal hind limbs poor prognosis |
|
|
clinical implications of saddle thrombus
|
in dogs with arteriosclerosis of cd aorta
less common than saddle thromboemboli in cats |
|
|
what is DIC
|
disseminated intravascular coag
pathologic activation of coag sys leading to inappropriate hypercoagualtion and secondary hemorrhage throughout the body |
|
|
what is your concern if you see petechiae and ecchymoses
|
DIC
|
|
|
sequential manifestations of DIC
|
mild or early cases detected only by abn coag profile (thrombocytopenia, elevated fibrin degredation products, prolonged clotting time)
formation of many microthrombi consume clotting factors and platelets results in spontaneous bleeding (consumptive coagulopathy) - excessive bleeding from venipuncture sites - petechiae andd ecchymoses mult org fail death |
|
|
causes of DIC
|
not a primary dz, but a complication of many conditions
heat stroke/ hyperthermia - widespread endothelial inj pancreatitis - circulating proteases activate coag cascade massive tissue inj - release of tissue factor into circulation sepsis - circulating cytokines activate and injure endothelial cells envenomation - endothelial inj and activation of coag cascade |
|
|
gross lesions of DIC
|
petechial and ecchymotic hemorrhages
NO grossly visible thrombi |
|

|
anasarca (generalized edema)
|
|

|
ascites
|
|
|
hyperemia/ congestion
|
|
|
hyperemia (physiologic)
|
|
|
physiologic hyperemia
|
|

|
pathologic hyperemia
|
|

|
pathologic hyperemia
(cystitis) |
|

|
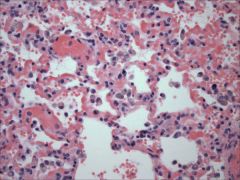
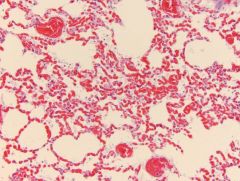
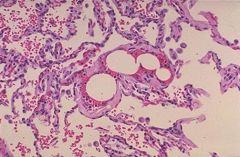
severe
acute diffuse pulmonary congestion |
|
|
what do you see when you have left heart failure
|
pulmonary edema
|
|
|
what do you see when you have right heart failure
|
hepatic congestion/ ascites
|
|
|
heart failure cells
hemosiderin laden macrophages due to pulmonary congestion |
|
|
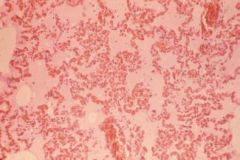
pulmonary congestion
|
|
|
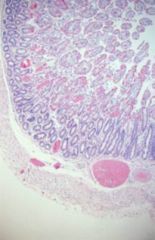
pulmonary congestion/ edema
|
|
|
chronic passive congestion (lung)
|
|

|
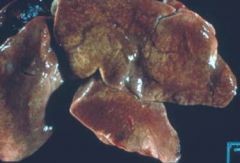
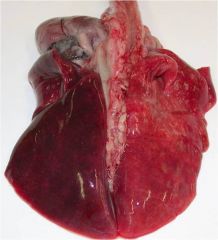
acute hepatic congestion
|
|

|
chronic hepatic congestion
|
|
|
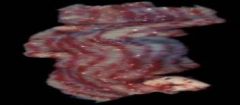
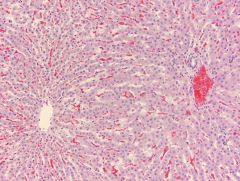
centrilobar hepatic congestion
(chronic hepatic congestion - nutmed liver) |
|

|
nutmeg liver
chronic hepatic congestion |
|
|
hypostatic congestion
|
|
|
hypostatic congestion
|
|

|
livor mortis
hypostatic congestion |
|

|
mesenteric torsion -> congestion
|
|

|
uterine torsion = ouch
|
|

|
diffuse splenic congestion
|
|
|
Which of the following would cause hepatic congestion
a. hepatitis b. heart failure c. vena caval obstruction at the kidneys d. B & C e. All of the above |
b. Heart failure
* vena caval obstruction at level of diaphragm would, but at level of kidney is before liver so no congestion * |
|

|
epistaxis
|
|

|
epistaxis
|
|

|
epistaxis
|
|

|
hemoperitoneum (hemoabd)
|
|

|
hemothorax
|
|

|
hemothorax
|
|

|
hematoma
|
|

|
splenic hematoma
|
|

|
petechial and ecchymotic hemorrhage
|
|

|
ecchymotic hemorrhage
|
|

|
petechial hemorrhage
|
|

|
endotoxic shock (on right side)
|
|
|
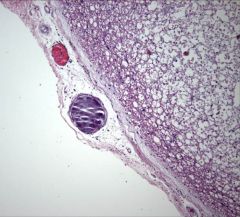
fat thromboemboli
|
|
|
fibrocartilaginous emboli
|
|
|
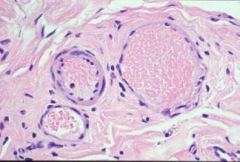
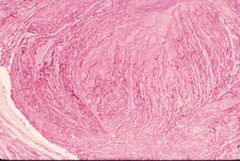
thrombi
lines of zahn |

