![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
What are the types of hyperparathyroidism? Levels of Calcium in each? |
- Primary: hypercalcemia
- Secondary: hypocalcemia - Tertiary: hypercalcemia |
|
|
What is the most common cause of primary hyperparathyroidism?
|
Parathyroid Adenoma
|
|
|
How are hormones / electrolytes affected by Primary Hyperparathyroidism?
|
- ↑ Ca2+: hypercalcemia and hypercalciuria
- ↓ PO4-: Hypophosphatemia - ↑ PTH - ↑ ALP - ↑ cAMP in urine |
|
|
What are the most common symptoms of Primary Hyperparathyroidism?
|
- Most often asymptomatic |
|
|
What mnemonic helps you remember the symptoms of hypercalcemia?
|
"Stones, bones, groans, and psychiatric overtones"
- Renal stones → abdominal / flank pain - Bones → osteitis fibrosa cystica (cystic bone spaces filled with brown fibrous tissue causing bone pain) - Groans → weakness and constipation - Psychiatric overtones → depression |
|
|
What happens in Osteitis Fibrosa Cystica? Cause?
|
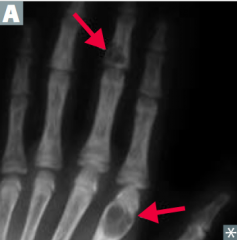
- Cystic bone spaces are filled with brown fibrous tissue → bone pain
- Caused by hyperparathyroidism |
|
|
What causes Secondary Hyperparathyroidism?
|
- Secondary hyperplasia due to ↓ gut Ca2+ absorption and ↑ PO4(3-)
- Most often in chronic renal disease (causes hypovitaminosis D → ↓ Ca2+ absorption) |
|
|
What are the hormone / electrolyte findings in Secondary Hyperparathyroidism?
|
- ↓ Ca2+: hypocalcemia
- ↑ PO4-: hyperphosphatemia in chronic renal failure, although most other causes have hypophosphatemia - ↑ ALP - ↑ PTH |
|
|
How are the bones affected by Secondary Hyperparathyroidism or Tertiary Hyperparathyroidism?
|
Bone lesions occur in 2° or 3° hyperparathyroidism due in turn to renal disease = Renal Osteodystrophy
|
|
|
What causes Tertiary Hyperparathyroidism?
|
Refractory (autonomous) hyperparathyroidism resulting from chronic renal disease
|
|
|
What are the hormone / electrolyte findings in Tertiary Hyperparathyroidism?
|
- ↑ Ca2+ |
|
|
What is the difference between secondary and tertiary hyperparathyroidism?
|
Both commonly due to chronic renal disease |
|
|
What are the most common causes of hypoparathyroidism?
|
Hypoparathyroidism: |
|
|
What are the findings associated with hypoparathyroidism?
|
- Hypocalcemia
- Tetany - Chvostek sign - Trousseau sign |
|
|
How do you check for a Chvostek sign? What does it indicate if it is positive?
|
- Tap the facial nerve (tap the cheek)
- Positive: contraction of facial muscles - Sign of hypoparathyroidism |
|
|
How do you check for a Trousseau sign? What does it indicate if it is positive?
|
- Occlusion of brachial artery with BP cuff (cuff the TRiceps)
- Positive: carpal spasm - Sign of hypoparathyroidism |
|
|
What is the other name for pseudohypoparathyroidism? Cause?
|
Albright Hereditary Osteodystrophy
- Autosomal dominant unresponsiveness of kidney to PTH |
|
|
What are the symptoms of Albright Hereditary Osteodystrophy? Cause?
|
- Hypocalcemia, shortened 4th/5th digits, and short sature
- Caused by autosomal dominant unresponsiveness of kidney to PTH (pseudo-hypoparathyroidism) |
|
|
Which PTH / Calcium pathology is associated with a low Ca2+ and a low PTH? Cause?
|
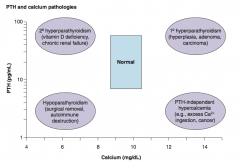
Hypoparathyroidism:
- Surgical removal - Autoimmune destruction |
|
|
Which PTH / Calcium pathology is associated with a low Ca2+ and a high PTH? Cause?
|
2° Hyperparathyroidism
- Vitamin D deficiency - Chronic renal failure |
|
|
Which PTH / Calcium pathology is associated with a high Ca2+ and a low PTH? Cause?
|
PTH-independent hypercalcemia:
- Excess Ca2+ ingestion - Cancer |
|
|
Which PTH / Calcium pathology is associated with a high Ca2+ and a high PTH? Cause?
|
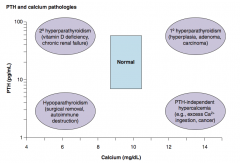
1° Hyperparathyroidism:
- Hyperplasia - Adenoma - Carcinoma |
|
|
What is the most common form of pituitary adenoma? Symptoms?
|
Prolactinoma |
|
|
How do you treat a prolactinoma (pituitary adenoma)?
|
Dopamine agonists:
- Bromocriptine - Cabergoline |
|
|
What are the types of pituitary adenomas?
|
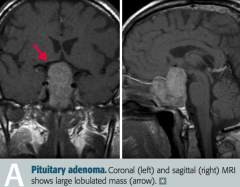
- Functional (hormone producing, eg, prolactinoma)
- Non-functional (silent, present with mass effect) |
|
|
What is most likely wrong in a patient with amenorrhea, galactorrhea, low libido, and infertility?
|
Prolactinoma (type of functioning pituitary adenoma) |
|
|
What is most likely wrong in a patient with bitemporal hemianopia, hypopituitarism, and a headache?
|
Non-functional pituitary adenoma, causing problems due to mass effect
|
|
|
What are the symptoms of a non-functional pituitary adenoma with mass effect?
|
- Bitemporal hemianopia
- Hypopituitarism - Headache |
|
|
What are the symptoms of a somatotropic pituitary adenoma?
|
Acromegaly
|
|
|
What is the cause of acromegaly?
|
Excess GH in adults, typically caused by a pituitary adenoma
|
|
|
What are the characteristic findings in a patient with Acromegaly?
|

- Large tongue with deep furrows
- Deep voice - Large hands and feet - Coarse facial features - Impaired glucose tolerance (insulin resistance) |
|
|
What is the name of the syndrome caused by increased GH in children? Symptoms? Cause of death?
|
Gigantism
- ↑ Linear bone growth - Cardiac failure most common cause of death |
|
|
How do you confirm a diagnosis of Acromegaly?
|
- ↑ Serum IGF-1
- Failure to suppress serum GH following oral glucose tolerance test - Pituitary mass seen on brain MRI |
|
|
How do treat a patient with Acromegaly?
|
- Pituitary adenoma resection
- If not cured, treat with Octreotide (somatostatin analog) or Pegvisomant (GH receptor antagonist |
|
|
What drug is a GH receptor antagonist?
|
Pegvisomant
|
|
|
What drug is a somatostatin analog?
|
Octreotide
|
|
|
What drugs are dopamine agonists?
|
- Bromocriptine |

