![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
what is the panpiniform plexus?
|
vascular bundle of the teste
warm arterial blood dissipates heat to the cooler venous blood helps to maintain scrotal temperature for spermatogenesis b/c if it inc by 3 degrees it may not function correctly |
|
|
Where's hormone and sperm production occur in the male?
|
testes
|
|
|
What occurs in the testes?
|
hormone and sperm production
|
|
|
What is the function of rete testes and efferent ducts?
|
movement of sperm
|
|
|
Where are sperm matured and stored?
|
epididymus
|
|
|
What occurs in the epididymus?
|
Maturation and storage of sperm; absorption of fluid, sperm gain motility here
|
|
|
What secretes fructose, PGs (prostaglandins), ascorbic/citric acid, and amino acids in the male repro system?
(It also produces 60% of seminal fluid) |
Seminal vesicles
|
|
|
What do the seminal vesicles secrete? 4
|
1. Secretion of fructose
2. PGs (prostaglandins) – semen hits uretus it will help propel it forward 3. ascorbic/citric acid 4. amino acids, etc. 60% of seminal fluid production. |
|
|
What secretes and stores fluid containing acid phosphatase, amylase, citric acid, and enzymes to liquey semen? (20% of seminal fluid production)
|
the prostate
|
|
|
What does the prostate do? 4
|
Secretion / storage of fluid containing
1. acid phosphatase, 2. amylase 3. citric acid; etc. 4. enzymes to liquify semen. 20% of seminal fluid production; |
|
|
What secretes fluid upon arousal to ‘flush’ urethra?
|
bulbourethral
(Cowper’s) glands |
|
|
What do the bulbourethral (Cowper’s) glands do?
|
Secretion of fluid upon arousal to ‘flush’ urethra
|
|
|
sperm develop in what structure within the teste?
|
seminiferous tubule (starts in the epithelium and matures until in lumen)
|
|
|
what are the 4 stages of spermatogenesis
|
1. spermatogonial proliferation - mitosis
2. meiosis – reduction division (~24 days) 3. spermiogenesis - transformation from round spermatids into spermatozoa 4. spermiation – release into lumen of seminiferous tubule |
|
|
male vs female
synchronous spermatogenesis/oogenesis |
Males: Synchronous (all the cells are linked and mature at a common rate)
Females: a-synchronous (kind of random as to which oocyte wins out with maturing) |
|
|
please discuss the H-P-Testis axis: GnRH, FSH, and LH.
|
GnRH-->ant pit-->LH/FSH
FSH: Sertoli cells- Inhibin (tuns off FSH) LH: Leydig cells- Testosterone (regulates GnRH) |
|
|
what hormone is required for the initiation of spermatogenesis? what other effect does this hormone have on spermatogenesis? 3
|
FSH
it also controls the rate of spermatogenesis, has a trophic effect on seminiferous epithelium, and inc sertoli cells. |
|
|
What does GnRH do? 2
|
releases FSH and LH
|
|
|
lack of what hormone will lead to atrophy of many the testicular structures?
|
Testosterone
trophic for epididymus, prostate, seminal vesicles converted to dihydrotestosterone / estradiol circulates bound to albumin or SHBG |
|
|
what produces inhibin B? what does it do (male) 3
|
produced by Sertoli cells; (-) FSH
marker of testicular function |
|
|
what is the role of estrogen in the teste? 2
|
fluid absorption
prevents blockage of the seminiferous tubule epithelium |
|
|
What hormones cause fluid absorption and prevents blockage of the seminiferous tubule epithelium?
|
estrogen
|
|
|
What does LH do in the male repro system? 1
|
inc Leydig cells
|
|
|
What hormone inc Leydig cells?
|
LH
|
|
|
What hormone is a marker of testicular function?
|
inhibin B
|
|
|
What hormone do Sertoli cell produce that dec FSH?
|
Inhibin B
|
|
|
What hormone is produced by Sertoli cells, is a marker of testes and inhibited by testosterone?
|
AMH
|
|
|
What does AMH do? 3
|
produced by Sertoli cells, is a marker of testes and inhibited by testosterone
|
|
|
required for spermatogenesis
(+) Sertoli cells (-) LH and GnRH trophic for epididymus, prostate, seminal vesicles converted to dihydrotestosterone / estradiol circulates bound to albumin or SHBG |
testerone
|
|
|
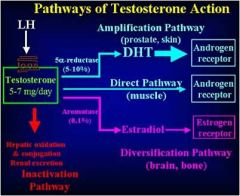
What does testerone do? 6
|
1. required for spermatogenesis
2. (+) Sertoli cells 3. (-) LH and GnRH 4. trophic for epididymus, prostate, seminal vesicles 5. converted to dihydrotestosterone / estradiol 6. circulates bound to albumin or SHBG |
|
|
What is AMH produced by? Use? (males)
|
product produced by Sertoli cells; marker of testes
if a person's balls never dropped and you need to find out if they are actually even there, you check AMH. If you see AMH then you have balls, if not....oh welll. |
|
|
What are the pathways of testerone action?
|
|
|
|
what makes up the blood testis barrier? Importance?
|
gap junctions connect sertoli cells: forms blood testis barrier, prevents immune response to developing sperm (which might be seen as non-self)
|
|
|
what is the importance of androgen binding protein? what produces it?
|
allows testosterone to bind to it and increase the level of testosterone in the epithelium of the seminiferous tubules where spermatogenesis is occurring
produced by: sertoli cells |
|
|
what cell phagocytizes degenerating germ cells?
|
Sertoli cells
|
|
|
what cell produces testosterone?
|
Leydig cells
|
|
|
What does sertoli cells secrete? 4
|
inhibin
androgen binding protein (ABP) growth factors (estradiol) |
|
|
What do leydig cells secrete? 2
|
testosterone, estradiol
|
|
|
3 functions of the sertoli cell blood/testis barrier?
|
1. establish osmotic gradient
2. allow for [] of ABP / T 3. basal/adluminal compartment basal: spermatogonia; preleptotene spermatocytes adluminal: remaining 1° spermatocytes; 2° spermatocytes; spermatids |
|
|
Some facts about the cycle of seminiferous epithelium. 4
|
--Synchronous development of germ cells during spermatogenesis
--All germ cells developing in a region of the epithelium derived from single stem cell --Different lengths of time spent in various stages of the spermatogenic process --Any one region of the seminiferous epithelium provides a snapshot of groups of cells representing the continuum of the spermatogenic process |
|
|
What characterizes the wave of spermatogenesis? 3
|
1. Regional grouping of germ cells at various developmental stages along epithelium
2. Asynchronous initiation of stem cell development results in temporal variation of the spermatogenic process along the epithelium 3. Always some section of epithelium undergoing spermiation allowing for constant supply of sperm |
|
|
Epididymus actions: 3
|
1. secretes: glycoproteins, sialic acid; glycerophosphocholine
2. maturation ~16 days further condensation of chromatin (histones replaced with protamines) and gain motility 3. storage ~60 +/- days |
|
|
What is capacitation? where does it occur?
***** |
change in membrane fluidity, metabolism, intracellular [ion], pH,
rendering the spermatazoan fertilization competent OCCURS IN FEMALE necessary for acrosome reaction note: decapatication factors in seminal fluid / epididymus |
|
|
What has to happen for a guy to get a woody?
|
1. NO - endothelium and parasympathetic non-adrenergic-noncholinergic cavernous nerves
2. inc guanylyl cyclase 3. inc cGMP 4. dec Ca and open K channels => smooth m. relaxation and engorgement. 5. the venous system is then closed off so the blood stays there |
|
|
What is emission?
|
deposition of semen in posterior urethra
- entry of semen into bladder blocked by closure of bladder sphincter thoracolumbar sympathetic induced smooth muscle contraction associated with epididymis, vas deferens, ampulla, seminal vesicles, prostate closure of bladder sphincter in response to sympathetic activation |
|
|
What is ejaculation?
|
ejection of semen out urethra
somatic pudental efferents to striated muscles of the pelvic floor and bulbocavernosus and ischiocavernosus (levator ani) muscles propels semen through urethra |
|
|
What is Andropause?
|
↓ in circulating total serum [testosterone]
values remain within normal range Leydig cell response to gonadotropins ↓ [inhibin] ↓ ↓ Leydig cell number patchy degeneration of seminiferous epithelium |
|
|
Delayed fatherhood associated with
|
reduced fertility and fecundity of a couple
cerebral palsy multiple sclerosis schizophrenia autism epilepsy reduced learning capacity mental retardation risk of spontaneous abortion preeclampsia stillbirth childhood cancers neonatal mortality |
|
|
What is a testicular varicocele?
|
kind of like vericose veins of the ballsack
problem with valves in veins draining the testes most common in men between 15 and 25 years seen most on left side of scrotum may be palpable or observable on gross exam common cause of male infertility |
|
|
how can obesity effect male fertility?
|
you get FAT BALLS
literally fat in the scrotum that increases the heat of the scrotum thus killing off some spermys |
|
|
What are some causes of Male infertility? 3
|
1. Erectile dysfunction - 1/10 over 40 yo
2. Ejaculatory dysfunction i. e. Retrograde ejaculation – autonomic dysfunction due to neuropathy such as with diabetes i. e. Premature ejaculation – nerves with serotonin and 5-HT R regulate speed of ejaculation 3. Sperm/Testicular/Tubule dysfunction In vitro fertilization (IVF) Intracytoplasmic sperm injection (ICSI) |

