![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
147 Cards in this Set
- Front
- Back
|
How is pregnancy usually diagnosed? |
A rise in the beta human chorionic gonadotropin (β-hCG)
Hormone is produced by the placenta |
|
|
When can a pregnancy be confirmed by ultrasound, and at what β-hCG level?
|
As early as 5 wks, correlating to a β-hCG of 1500-2000
|
|
|
Define the following terms:
Previable Preterm Full-term Post-term |
Previable: <24wks or weight less than 500g
Preterm: btw 24-36 6/7 wks Full-term: btw 37 -42 wks Post-term: >42 wks |
|
|
What are the common terms used to describe a patient’s pregnancy history?
|
Gravidity: # of times a woman has been pregnant
Nulligravid: never been pregnant Nulliparous: has not delivered a baby >20wks Primip (Primiparous): has delivered 1 baby Multip (Multiparous): has delivered more than 1 baby Parity: # of pregnancies that led to a birth beyond 20wks or infant greater than 500g Term Preterm Abortions (elective & spontaneous) Living children |
|
|
What is Näegele's rule?
|
Subtract 3 months from the LMP & add 7 days
|
|
|
When should you be able to detect fetal heart tones by Doppler ultrasound?
|
10 weeks
|
|
|
How much does cardiac output (CO) increase during preg?
|
CO ↑ 30-50%
|
|
|
Describe the effects of pregnancy on pulmonary physiology
|
Tidal volume: ↑ by 30-40%
Lung capacity: ↓ 5 % PaO2 and PAO2: ↑ PaCO2 and PACO2: ↓ |
|
|
What causes nausea and vomiting a/w pregnancy?
|
↑ levels of estrogen, progesterone, β-hCG
|
|
|
What are the hematogenous effects of pregnancy?
|
Dilutional anemia
↑ WBC ↓ platelets hypercoagulable |
|
|
What produces progesterone during pregnancy?
|
Corpus luteum (early) then the placenta (starting 9-11 wks)
|
|
|
What is the term for hyperpigmentation of the face?
|
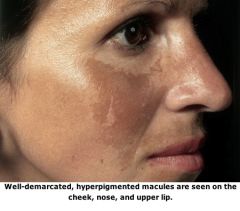
Melasma “mask of pregnancy”
|
|
|
does pregnancy have an effect on thyroid hormones?
|
Β-hCG has a weak stimulating effect on the thyroid – leads to slight ↑ in T3/T4 and slight ↓ TSH
|
|
|
What is the caloric requirement for an average preg woman?
|
2300-2800 kcal/day
Protein requirements: ↑ to 70-75g/day |
|
|
What are the folic acid recommendations for preg women?
|
Normal preg: 800-100mcg per day
High risk (h/o Neural Tube Defects): 4000mcg per day |
|
|
A 32-year-old pregnant woman has had a previous child with a neural tube defect. How much folic acid is recommended during this pregnancy?
|
At least 4000mcg (4mg) per day
|
|
|
In the early stages of a normal pregnancy how does the β-hCG level change?
|
Doubles every 48hrs
|
|
|
A 26-year-old female presents with amenorrhea. Her last period was about 5-8 weeks ago. She has a β-hCG level of 2200. Her ultrasound shows no intrauterine pregnancy. Why is this potentially concerning?
|
An IUP should be visible at a β-hCG level btw 1500-2000
This patient may have an ectopic pregnancy |
|
|
A 28-year-old pregnant female at 12 weeks gestational age presents with severe vomiting. She has lost significant weight in the last two weeks. What is her probable diagnosis?
|
Hyperemesis gravidarum
Greater than a 5% weight loss from prepregnancy weight & ketosis |
|
|
How does pregnancy affect the lab values of blood urea nitrogen (BUN) and creatinine?
|
BUN & Cr will ↓ by 25%
|
|
|
What are the imp lab tests for the initial visit?
|
CBC
Blood type Antibody screen RPR (syphilis) Rubella antibody screen HIV Hepatitis B surface antigen Urinalysis Urine Culture VZV titer (if no h/o chicken pox) PPD |
|
|
What is included in the quad screen?
|
a blood test (non-invasive) done btw 15-20wks
β-hCG Estriol Maternal serum α-fetoprotein (MSAFP) Inhibin A |
|
|
When is RhoGAM given routinely during prenatal care?
|
At 28 wks (note that RhoGAM lasts ~12 wks, which will cover til about 40wks)
|
|
|
When is the group-B streptococcus (GBS) screen performed?
|
35-37wks
|
|
|
Which immunizations are contraindicated in pregnancy?
|
Measles, mumps & rubella (MMR) – give this post-partum
Varicella Oral polio Nasal influenza (the shot is okay!) |
|
|
What is the primary cause of lower extremity edema in pregnant women?
|
Compression of the inferior vena cava
Compression of the pelvic veins |
|
|
What are the components of the biophysical profile (BPP)?
|
Amniotic fluid volume
Fetal tone Fetal activity Fetal breathing movements Nonstress test (NST) Score of 8-10 is reassuring |
|
|
What test is commonly used to assess fetal lung maturity?
|
Lecithin to sphingomyeline ratio (as lungs mature, lecithin increases & sphingomyeline decreases, ∴ a ratio >2 signifies mature lungs)
|
|
|
What test allows you to sample fetal blood to confirm platelet alloimmunization in the case of severe fetal anemia?
|
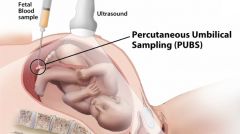
Percutaneous umbilical blood sampling (PUBS) or cordocentesis
|
|
|
What medications are often used to treat GERD associated with pregnancy?
|
H2 blockers & PPIs (both are Class B meds)
H2 blockers include: - Cimetidine (Tagamet) - Ranitidine (Zantac) - Famotidine (Pepcid, Mylanta) PPIs: - Omeprazole (Prilosec) - Lansoprazole (Prevacid) - Pantoprazole (Protonix) - Esomeprazole (Nexium) |
|
|
Urine is routinely checked at prenatal visits. What abnormal findings in the urinalysis may indicate disease or complication?
|
Protein → can indicate preeclampsia
Glucose → can indicate gestational diabetes Leukoesterase → can indicate urinary tract infection (UTI) |
|
|
A 26-year-old female has recently had a positive pregnancy test. Her last menstrual period was 7/4/11. What is her estimated date of confinement using Näegele's rule?
|
4/11/12
|
|
|
A 35-year-old female is currently pregnant. She has been pregnant 3 times prior to this pregnancy. She had one miscarriage at 10 weeks. She has two living children now with one baby born at term and one baby born preterm. Characterize this patient using TPAL designation.
|
G4P1112
|
|
|
A 33-year-old female has given birth to one set of preterm twins, one term infant and had one miscarriage. Characterize this patient using TPAL designation.
|
Note: twins always ct as 1, for both G & Ps (except for living children)
G3 P1113 |
|
|
Fundal height measurement corresponds with gestational age. If the fundal height does not match the gestational age, when is it appropriate to order an ultrasound?
|
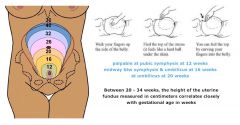
Generally when the fundal height is 3cm off from the gestational age
|
|
|
When is the glucose loading test performed during pregnancy in a normal risk patient?
|
27-29 weeks
|
|
|
If a patient has an abnormal glucose loading test what is the next step?
|
A glucose tolerance test
Patient is given oral dose of 100g of glucose Serum glucose is checked fasting, at 1, 2 and 3 hrs Diabetes is diagnosed if the pt has abnormal values in 2 or more values |
|
|
What is the common name for irregular contractions, and what is a common cause of these contractions?
|
Term → Braxton Hicks contractions
Cause → Dehydration note: the magic number is >6 contractions/hr for true labor - they should be occurring in REGULAR intervals, the intervals should be SHORTENING, INTENSITY increasing and leading to cervical dilation |
|
|
What are the major causes of ↑ urinary frequency in a pregnant patient?
|
↑ intravascular volume
↑ GFR compression of the bladder by the growing uterus (primary reason) also r/o diabetes & urinary tract infection (UTI) |
|
|
What are the characteristics of cystic fibrosis?
|
Aut Recessive disease
Disorder of chloride transport Affects the lungs & pancreas |
|
|
What are the characteristics of sickle-cell disease?
What is the screening test for sickle cell? |
Aut Recessive disease
Single point mutation in the gene for the beta chain in hemoglobin → forms hemoglobin S Causes hemolytic anemia, shortened life span and pain crisis Screening test = hemoglobin electrophoresis |
|
|
What are the characteristics of Tay-Sachs disease?
|
Aut Recessive disease
More common in Eastern European Jews & French Canadians Pts die by age 4 Severe neurologic degeneration Deficiency of hexosaminidase A enzyme Cherry-red spot on fundoscopic exam Serum screening test |
|
|
What are the characteristics of β-thalassemia?
|
Impairment of the β-chain production
Leads to an excess of alpha chains Autosomal recessive Minor (heterozygous) form that causes mild anemia Major (homozygous) form is fatal usually by age 20 |
|
|
Describe the differences between the α-thalassemias
|
Can have alterations in 4 genes
4 deletions → hemoglobin Bart, incompatible with life 3 delections → hemoglobin H disease, severe 2 deletions → α-thalassemia trait, mild anemia 1 deletion → silent carrier |
|
|
What is a common risk factor for Down syndrome?
|
↑ maternal age
|
|
|
What are the common screening tests for Down syndrome in the first trimester?
|
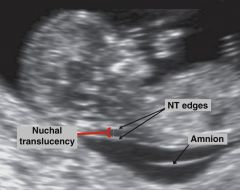
Ultrasound measuring nuchal translucency
Serum free β-hCG & pregnancy associated plasma protein A (PAPP-A) The nuchal translucency (NT) measurement is the maximum thickness of the subcutaneous translucent area between the skin and soft tissue overlying the fetal spine at the back of the neck. Calipers are placed on the inner borders of the nuchal space, at its widest portion, perpendicular to the long axis of the fetus. In this normal fetus at 12 weeks' gestation, the measurement is 2.0 mm. |
|
|
What are the common screening tests for Down syndrome in the second trimester?
|
Quad screen
Anatomic ultrasound |
|
|
What are the characteristics of trisomy 18 (Edwards Syndrome)?
|
Screen with Quad screen
Death by age 2 Abnormal ultrasound (choroid plexus) |
|
|
What are the characteristics of trisomy 13 (Patau)?
|
Death by age 1
Not found by serum screening Severely abnormal ultrasound |
|
|
What are the characteristics of Turner syndrome?
|
Female, short stature, web neck, shield chest
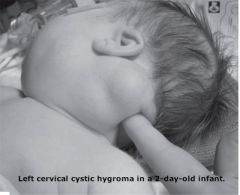
Typically present with primary amenorrhea Ultrasound with cystic hygroma No screening test available notes on cystic hygromas: CYSTIC HYGROMA (LYMPHANGIOMAS) CLINICAL SUMMARY Cystic hygromas are lymphatic malformations found most commonly in the neck in infants and children less than 2 years of age. They present as nontender, compressible, unilocular, or multilocular masses with thin, transparent walls and are filled with straw-colored fluid. Unlike hemangiomas, these lesions rarely undergo spontaneous regression. The vast majority tend to grow and infiltrate adjacent structures. |
|
|
What are the characteristics of Klinefelter syndrome?
|
Small firm testicles, infertility, gynecomastia
Mental retardation No screening test available |
|
|
When does organogenesis occur?
|
3-8 weeks after conception
(5-10 weeks gestational age) |
|
|
What is the teratogenic effect of the ACE inhibitors?
List some common ACE inhibitors |
Fetal tubular dysplasia
ACE Inhibitors include: Benazepril (Lotensin) Captopril Enalapril (Vasotec) Fosinopril Lisinopril (Prinivil, Zestril) Moexipril (Univasc) Perindopril (Aceon) Quinapril (Accupril) Ramipril (Altace) Trandolapril (Mavik) |
|
|
What is anencephaly vs encephalocele vs meningocele ?
|
anencephaly = Lack of formation of the upper parts of the brain
Encephalocele → cyst or defective formation of the back of the skull Meningocele → more severe form of spina bifida in which you have membranes protruding out of the spine that failed to fuse |
|
|
What is used to screen for neural tube defects?
|
NTDs are a/w: ↓ maternal folate, ↓ maternal vit B12
Seen on ultrasound: lemon & banana signs Screening test = ↑ maternal serum α-fetoprotein (MSAFP) |
|
|
When does the heart start to develop?
|
5th week of gestational age
|
|
|
What are the most common cardiac defects?
|
Atrial Septal defect (ASD)
Ventricular septal defect (VSD) Tetralogy of Fallot Transposition of the great vessels Hypoplastic left heart Patent ductus arteriosus |
|
|
What are the characteristics of Potter syndrome?
|
Bilateral renal agenesis
Anhydramnios (no amniotic fluid) Pulmonary hypoplasia Contractures of the limbs |
|
|
Patients with the carrier state of sickle-cell disease are resistant to what disease?
|
Malaria
|
|
|
When are fetuses most susceptible to teratogens?
|
During organogenesis (5-10 weeks gestational age)
|
|
|
A 32-year-old female has recently become pregnant. She had a previous child with a neural tube defect. How much folic acid should this patient take daily?
|
Normal pregnancy: 800-1000mcg
High-risk pregnancy: 4000mcg (4 mg) |
|
|
What is the most common congenital heart defect and how does it present?
|
VSD – holosytolic murmur
If small defect → asymptomatic Large defect → signs of heart failure (tachypnea, poor feeding) |
|
|
A newborn presents with upslanting palpebral fissures, epicanthic folds, and a protruding tongue. Which first trimester screens could have been used to detect this abnormality?
|
Trisomy 21 - Down’s syndrome
Nuchal translucency measurement Free β-hCG Pregnancy associated plasma protein-A (PAPP-A) |
|
|
What are the 4 tests that make up the Quad screen?
|
MSAFP, Estriol, β-hCG, Inhibin-A
|
|
|
What is the best time to check a Quad screen?
|
Between 15 -18 weeks gestation
|
|
|
What are the expected Quad screen findings for a fetus with trisomy 21?
|
High AFP → suggests Neural tube defect
Low AFP → suggests either Trisomy 21 or Trisomy 18 |
|
|
How can you tell Trisomy 21 from Trisomy 18 on Quad Screen?
|
Trisomy 21 → high β-hCG, high inhibin A
|
|
|
What are the most common first trimester screening tests for aneuploidy?
|
Nuchal translucency
Free β-hCG Pregnancy-associated plasma protein A (PAPP-A) |
|
|
What is included in the quad screen?
|
MSAFP, Estriol, β-hCG, Inhibin-A
Down Syndrome: low AFP, low estriol, high β-hCG, high inhibin-A Trisomy 18: all are low – low AFP, low estriol, low β-hCG, low inhibin-A Neural tube defects: high AFP |
|
|
When is the most common time to perform an ultrasound?
|
20 weeks gestational age (also the time you can tell sex)
|
|
|
When is it considered safe to perform an amniocentesis?
|
After 15 weeks gestational age
|
|
|
What are the potential complications of amniocentesis?
|
Fetal death 1:400
Preterm premature rupture of membranes 1-2% Infection <0.1% |
|
|
Why is chorionic villus sampling not used as often as amniocentesis?
|
Risk of fetal loss about 1%
|
|
|
Match the genetic disease with its characteristic defect
CF - Sickle Cell - Tay-Sachs - Thalassemia |
Cystic fibrosis → Disorder of chloride transport
Sickle-cell disease → Hemolytic anemia and pain crisis Tay-Sachs → Cherry-red spot on fundoscopic exam β-thalassemia → Minor (heterozygous) form causes mild anemia α-thalassemia → Hemoglobin Bart is most severe form |
|
|
What are the second trimester serum screening tests for Down syndrome?
|
MSAFP, Estriol, Free β-hCG, Inhibin-A
|
|
|
Besides the quad screen what other piece of information is very important when calculating the risk for aneuploidy?
|
Maternal age
|
|
|
What are the quad screen results for a baby with the following abnormalities?
Down Syndrome - Trisomy 18 - NTDs |
Down Syndrome: low AFP, low estriol, high β-hCG, high inhibin-A
Trisomy 18: all are low – low AFP, low estriol, low β-hCG, low inhibin-A Neural tube defects: high AFP |
|
|
Which screening tests are used for Turner and Klinefelter syndrome?
|
No screening tests – can be diagnosed with karyotype tests
|
|
|
A 17-year-old female presents with a complaint of having never had a period. She is short for her age and has immature sexual characteristics. What is the most likely diagnosis?
|
Turner Syndrome
|
|
|
After how many weeks of gestational age should an amniocentesis be performed in order to have the lowest incidence of complications?
|
After 15 weeks
|
|
|
Other than karyotype analysis what is the other use of fetal blood sampling?
|
Can be used to transfuse the fetus in cases of fetal anemia
|
|
|
When is the most common time for a prenatal ultrasound in a low-risk patient?
|
Around 20 weeks
|
|
|
Which organs are most affected by cystic fibrosis?
|
Lungs & pancreas
|
|
|
What are the characteristics of Braxton Hicks contractions (“false labor”)?
|
Irregular in duration & timing
Less severe than true labor Resolve with ambulation, hydration & analgesia Tell her to drink a big glass of water & take a walk! |
|
|
What does the “bloody show” indicate?
|
Beginning of cervical effacement
|
|
|
What important pregnancy information should be reviewed when a pregnant woman presents to labor and delivery?
|
Dating – how far along is the patient?
Ultrasound – is dating consistent? Any abnormalities? H&H – were there any signs of anemia during the preg? Blood type – if Rh neg, might require RhoGam HIV Hepatitis B Syphilis Group B Strep Glucose tolerance – any gestational diabetes? Check for prenatal care – did patient have any? Physical exam: fetal heart rate, fetal lie (Leopold’s maneuver), fetal presentation, Pelvic exam – to check for rupture of membranes |
|
|
Define PROM and PPROM.
|
PROM: rupture of membranes before labor
PPROM: rupture of membranes before 37weeks gestation |
|
|
Name the three most commonly used tests to determine rupture of membranes (ROM)
|
(1) Pooling – with speculum, check for pooling of amniotic fluid
(2) Fern test - Using a sterile speculum, swab a sample of fluid "pooled" in the vaginal vault onto a glass slide and let it air dry. Amniotic fluid yields an arborization, or "fern," pattern seen under 10x magnification. (3) Nitrazine test - Nitrazine paper has a pH turning point of 6.0. Normal vaginal pH in pregnancy is 4.5–6.0; amniotic fluid pH is 7.0–7.5. for (+) Nitrazine test: color change in the paper from yellow to blue. (4) Amnisure – a new test, more expensive |
|
|
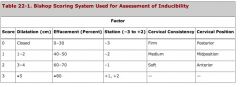
Name the components of the digital pelvic exam or Bishop score.
|
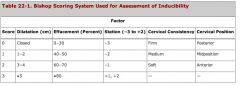
Cervical dilation (range from 0-10cm, “fully dilated”)
Cervical effacement – “thinning” of cervix Fetal station – relation of fetal head to ischemial spines of the mother (-3 to 3 station, as 5 point scale) Cervical position - range from anterior, mid, posterior Consistency of the cervix – thin to firm |
|
|
What does it mean when a cervix is fully effaced?
|
100% effacement – the cervix is as thin as the adjoining lower uterine segment
|
|
|
Fetal position is based on what?
|

The relationship of the fetal occiput to the maternal pelvis
|
|
|
Which fetal fontanelle is larger?
|
Anterior
the fontanelles are used to assess the fetal position |
|
|
A 25-year-old pregnant female at 39 weeks gestational age presents to labor and delivery. She believes that her water has broken. On pelvic exam she has some fluid in the vagina. The nitrazine paper turns immediately blue. Explain why this happens.
|
Normal vaginal secretions are acidic
Amniotic fluid is alkaline Nitrazine tests for alkaline substances |
|
|
Compare & contrast the anterior & posterior fetal fontanelles.
|
Anterior: larger & diamond-shaped
Posterior: smaller & triangle-shaped |
|
|
While examining a laboring patient you estimate that the fetal head is at the level of the maternal ischial spines. What is the station?
|
0 station
|
|
|
A 24-year-old pregnant patient presents to labor and delivery with regular contractions every 5 minutes. After a pelvic exam you calculate her Bishop score at 9. Is this patient likely to continue to a spontaneous vaginal delivery?
|
Yes, a bishop score ≥8 has a high likelihood of progressing to a spontaneous delivery
|
|
|
How does electronic fetal monitoring affect infant mortality and cesarean section rates?
|
Does not affect infant mortality
↑ C-section rates |
|
|
What pattern is needed for a fetal heart tracing to be considered reactive?
|
2 accelerations
at least 15 beats/min over the baseline last for at least 15 sec within 20 minutes |
|
|
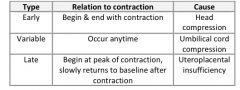
Describe early decelerations - what causes early decelerations?
|
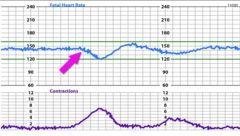
gradual decrease in FHR with onset to nadir >30sec; deceleration begins with a contraction, and the nadir occurs at the same time as the peak of the contraction
caused by head compression during contractions no clinical significance & allow labor to continue |
|
|
Describe late decelerations - what causes them?
|
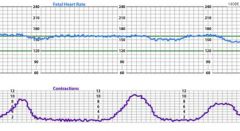
symmetrical & gradual decrease & return of FHR - onset to nadir >30sec; assoc with contractions, delayed in timing and nadir occurs after the peak of contractions
cause = Uteroplacental insufficiency |
|
|
Describe variable decels - what causes them?
|
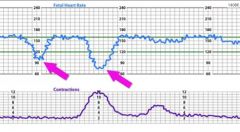
Variable = abrupt decrease in FHR ; drop by >15bpm, last >15sec and <2 min duration
When a/w contractions, their onset, depth and duration vary with contractions - mostly result from cord compression |
|
|
When is the use of a fetal scalp electrode contraindicated?
|
Maternal hepatitis, HIV
fetal thrombocytopenia |
|
|
How do you calculate Montevideo units?
|
Average of the variation of intrauterine pressure from the baseline x number of contractions in a 10min period
|
|
|
What are the three major maternal changes that take place prior to delivery?
|
Contractions
Lightening (caused by decent of the fetal head) Bloody show |
|
|
When a patient presents to labor and delivery, what important pregnancy information should you get from her medical records?
|
Look at G & Ps
Dating Blood pressure history Labs → CBC, blood type, HIV, hep B, syphilis, GBS, glucose loading tests Recurrent UTIs or proteinuria Quad screen for genetic abnormalities |
|
|
A 25-year-old G1P0 female presents at 35 weeks gestational age with potential rupture of membranes. She denies any vaginal bleeding, abdominal pain or contractions. Her nitrazine and fern tests are positive. What is her likely diagnosis?
|
Preterm Premature ROM (PPROM)
|
|
|
What is the benefit of an intrauterine pressure catheter over an external tocometer?
|
External tocometer → records the frequency of contractions but not accurate in determining the strength/pressure of the contractions
IUPC → can record the actual pressure produced by each contraction |
|
|
Compare and contrast the three types of fetal heart rate decelerations.
|
see above
|
|
|
What instructions should you give a patient who is experiencing Braxton Hicks contractions?
|
Drink water, ambulate, rest
|
|
|
What are the five components of the pelvic exam or Bishop score, and what are the values for each?
|
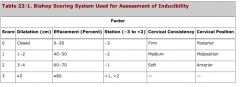
Cervical dilation (0-10cm)
Cervical effacement (0-100%) Fetal station (-5 to +5 or -3 to +3) Cervical position (anterior, mid, posterior) Consistency of the cervix (firm – soft) |
|
|
Name the five bones that comprise the fetal head, and what makes up the anterior and posterior fontanelles.
|
2 frontal bones, 2 parietal bones, 1 occiput
anterior fontanelle → formed by the junction btw the 2 frontal bones & the 2 parietal bones = diamond-shaped Posterior fontanelle → formed by the junction btw the 2 parietal bones & the occiput - Triangle-shaped |
|
|
Why is the use of continuous electronic fetal monitoring in a low risk patient potentially controversial?
|
No trials have proven reduction in:
Mortality Rate of cerebral palsy Stillbirth Low apgar scores NICU admission Neurological injury |
|
|
When is the use of a fetal scalp electrode contraindicated?
|
Maternal hepatitis or HIV
Fetal thrombocytopenia |
|
|
Describe the cardinal movements of labor (these are fetal movements that are necessary to move the baby through the birth canal)
|
Engagement: descent of the baby’s head below the plane of the pelvic inlet
Descent: downward passage of the presenting part through the pelvis Flexion: fetal head will flex in order for the smallest diameter of the head to pass through the maternal pelvis Internal rotation: rotation of the presenting part from its original position to the anterioposterior position as it passes through the pelvis Extension: occurs once the fetus has descended to the level of the introitus. Fetal head is delivered by extension & rotates around the symphysis pubis External rotation: fetal head rotates to the correct anatomic position in relation to the fetal torso Expulsion: anterior shoulder rotates under the symphysis pubis, after which the rest of the body usually delivers without difficulty |
|
|
Define the first stage of labor.
|
Interval btw the onset of labor & full cervical dilation
|
|
|
What are the two divisions of the first stage of labor?
|
Latent phase: early stage of labor, ends about 3-4cm of cervical dilation, slower pattern
Active phase: occurs btw 3-4 cm to 10cm of cervical dilation, occurs more rapidly than latent phase |
|
|
What term is used when either the baby is too big or the pelvis is too small for normal vaginal delivery?
|
Cephalopelvic disproportion (CPD)
|
|
|
What occurs during the second stage of labor?
|
Time period btw complete cervical dilation & the delivery of the infant
|
|
|
Define hypertonus and tachysystole.
|
Hypertonus: a single contraction lasting more than 2 min
Tachysystole: greater than 5 contractions in a 10min period Note: treatment for either of these conditions → terbutaline |
|
|
When should the patient begin to push during labor?
|
When the cervix is fully dilated
When the mother feels the urge to push |
|
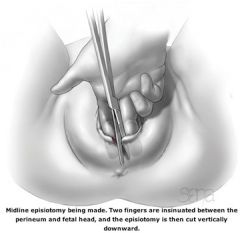
Episiotomies have been found to increase the risk of what complications?
|
3rd & 4th degree lacerations
|
|
|
Notes: techniques in delivering the baby:
|

Ritgen maneuver → heel of delivering hand is used to relieve pressure on the perineum – fingers placed btw the anus & coccyx and lift the fetal chin anteriorly
Or → place your hand on the vertex to maintain the fetal head in a flexed position and then control the speed of the crowning as the baby is coming out – just gentle pressure to make sure the baby doesn’t pop out (which is when you get the bad tears) then use other hand to “lip” the perineum over the fetal head |
|
|
What should be done immediately after the head is delivered?
|
Neonatal suctioning: studies have shown no benefit to neonatal suctioning on the perineum (did not reduce rate of meconium aspiration syndrome) – no need for suctioning unless there are signs of respiratory obstruction
Check for nuchal cord |
|
|
After bulb suction and checking for nuchal cord what is the next step in delivery?
|
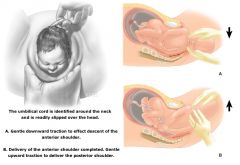
Place a hand on each parietal eminence of the baby’s head
Gently use downward traction to help slip the anterior shoulder under the pubic symphysis |
|
|
The 3 Ps:
|
Power
Passenger Pelvis |
|
|
A 29-year-old G3P2 patient is in the active phase of the 1st stage of labor. She is currently on Pitocin to help augment her labor. The continuous fetal heart rate monitor has recorded a late deceleration. What simple measures can immediately be taken to help this situation?
|
- Late decelerations = think uteroplacental insufficiency
- Stop the oxytocin (Pitocin) - Face mask oxygen - Turn onto left side to ↓ Inferior Vena Cava (IVC) compression to ↑ uterine perfusion |
|
|
A 31-year-old G2P1 patient is in active labor when she has 6 contractions in a 10-minute span. What is the diagnosis, and what can be given to the patient to help relax the uterus?
|
Dx: tachysystole
Tx: terbutaline |
|
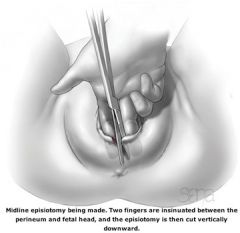
What are some indications for episiotomy?
|
(1) High risk of severe perineal lacerations
(2) Soft tissue dystocia (3) Facilitate deliver of a possibly compromised fetus |
|
|
How long does the 1st stage of labor last in a nulliparous and a multiparous woman?
|
Nullip: avg 10-12hrs
multip avg 6-8hrs |
|
|
A 23-year-old G1P0 patient has dilated to 5 cm and is at 50% effacement. She has an adequate contraction pattern with over 200 Montevideo units, but her cervical dilation nor her effacement have changed in over 2 hours. What is her diagnosis?
|
Active phase arrest
|
|
|
What are the potential positive and negative effects of delayed cord clamping?
|
Positive: more blood is transferred from the placenta to the infant
Negative: potential ↑ risk of polycythemia & neonatal jaundice |
|
|
What is the benefit of collecting cord blood?
|
Can test the baby’s blood type & Rh status
|
|

What are the 3 classic signs of placental separation?
|
1. Lengthening of the umbilical cord
2. A gush of blood from the vagina signifying separation of the placenta from the uterine wall 3. A change in the shape of the uterine fundus from discoid to globular with elevation of the fundal height |
|
|
According to the 2000 Cochrane review, why is active management beneficial over expectant management when delivering the placenta?
|
↓ risk of maternal blood loss
↓ postpartum hemorrhage ↓ incidence of prolonged 3rd stage of labor |
|
|
What is the definition of a retained placenta?
|
Placenta that has not delivered within 30 min after the baby
|
|
|
Describe the different types of lacerations that can occur during delivery.
|
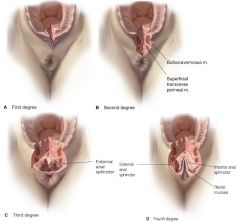
1st degree: involves the mucosa or skin
2nd degree: extends into the perineal body 3rd degree: extends into the anal spincter 4th degree: extends into the mucosa |
|
|
What is the fourth stage of labor?
|
2 hour period after the delivery of the placenta
|
|
|
What should always be done when applying cord traction during active management of placenta delivery?
|

The other hand should secure the uterus to prevent uterine inversion
|
|
|
A 22-year-old G1P0 patient is in the active phase of labor. She is dilated to 6 cm and is 50% effaced. Her external tocometer shows a consistent contraction pattern. She has not dilated for over 2 hours. What is the next step in her management?
|
Intrauterine pressure catheter (IUPC) – to measure the pressure of her contractions (the “power”)
Can then be given oxytocin to augment labor |
|
|
List the minimum gear and materials you will need for a vaginal delivery
|
Gowned, gloved, goggled
Two clamps Scissors Suction bulb DeLee suction trap Sterile towels |
|
|
Describe the 4 stages of labor.
|
1st Stage: Interval btw onset of labor & full cervical dilation
Latent phase: beginning of labor to 3-4cm of cervical dilation Active phase: 4-10cm of cervical dilation 2nd Stage: time period between complete cervical dilation and the delivery of the infant 3rd Stage: begins after delivery of the infant and ends with the delivery of the placenta 4th Stage: 2hr period after the delivery of the placenta |
|
|
Match the type of laceration with its corresponding degree.
|
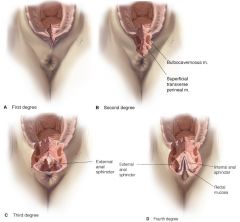
1st degree: involves the mucosa or skin
2nd degree: extends into the perineal body 3rd degree: extends into the anal spincter 4th degree: extends into the mucosa |
|
|
What is the difference between expectant and active management of placental delivery?
|
Expectant → Passive
Delivery of the placenta without uterotonic agents, cord clamping, or cord traction Active management: Early cord clamping Controlled cord traction Administration of a uterotonic agent |
|
|
What is considered an abnormally prolonged 2nd stage of labor?
|
Nullip: if >2hrs or >3hr with epidural
Multip: if >1hr or >2hrs with epidural |
|
|
What are the next several management steps after the head of the infant is delivered?
|
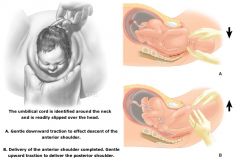
Evaluate for nuchal cord (reduce nuchal cord if needed)
Place a hand on each parietal eminence of the baby’s head Gently use downward traction to help slip the anterior shoulder under the pubic symphysis Deliver the rest of the baby |
|
|
After the baby is born and no signs of fetal distress are apparent, what should be encouraged?
|
Early interaction with mother (skin to skin)
Early initiation of breastfeeding |
|
|
What are the potential positive and negative effects of delayed cord clamping?
|
Positive effects: more blood is transferred from the placenta to the infant – ↓ rate of neonatal anemia
Negative effects: potential ↑ risks of polycythemia, neonatal jaundice |

