![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
220 Cards in this Set
- Front
- Back
|
What is the tx for hyperparathyroidism due to parathyroid hyperplasia?
|
- remove 3.5 glands, mark the remaining half gland with surgical clip
- autotransplant from neck region to forearm |
|
|
What are the high potency neuroleptics?
|
Haloperidol (Haldol)
Fluphenazine (Prolixin, Permitil) Thiothixene (Navane) Droperidol (Inapsine) "High Five Thio after he THINX he DROPped his number for a girl" (Haldol, Fluphenazine, ThioTHIXene, Droperidol" |
|
|
LIst the low potency typical neuroleptics
|
Chlorpromazine (Thorazine)
Thioridazine (Mellaril) there's LOW (low potency) CHLORine in the Pool (chlorPromazine) after THIO gets RID of the chlorine |
|
|
List the moderate potency typical neuroleptics
|
Molindone
Loxapine Trifluorperazine "just TRI MOLin' around, there's LOX of boys around here" |
|
|
List the Atypical Antipsychotics
|
Clozapine (Clozaril, FazaClo)
Olanzapine (Zyprexa) Risperidone (Risperdal) Quetiapine (Seroquel) Aripiprazole (Abilify) Paliperidone (Invega) |
|
|
What mineralcorticoid medication is used in the treatment of aldosterone deficiencies such as adrenal insufficiency & 21-hydroxylase deficiency?
|
fludrocortisone (Florinef)
|
|
|
Where is the brain lesion?
pt presents w/ contralateral hemiballismus (rapid, unpredictable flailing movements of arm, leg) |
subthalamic nucleus
|
|
|
Where is the lesion?
pt presents with hemispatial neglect syndrome |
right parietal lobe
|
|
|
where is the brain lesion if pt presents in coma?
|
Pons - specifically reticular activating system (RAS)
|
|
|
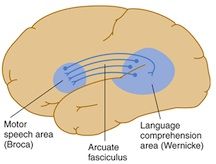
Where is the brain lesion if pt presents with poor repetition
(meaning patients can speak relatively well and have good auditory comprehension but cannot put parts of words together or conjure up words) |
termed conduction aphasia, lesion of the arcuate fasciculus, in the white matter underlying the temporal–parietal junction; this lesion disconnects Wernicke's area from Broca's area.
|
|
|
where is the brain lesion?
The patient has difficulty naming even simple objects. Repetition is impaired, but comprehension of spoken language is normal. The patient is usually aware of the deficit and appropriately concerned about it. |
Broca's aphasia caused by a lesion in the inferior frontal gyrus in the dominant hemisphere
Most lesions that involve Broca's area also involve the neighboring motor cortex. Patients are often hemiplegic, with the arm more affected than the leg. Broca's aphasia often occurs as a result of strokes, most commonly affecting the middle cerebral artery territory. |
|
|
Where is the brain lesion?
Pt has fluent speech, but repetition and comprehension are impaired. Has difficulty naming objects and produces both literal paraphasias (eg, "wellow" instead of "yellow") and verbal paraphasias (eg, "mother" instead of "wife"). Neologisms (meaningless, nonsensical words) are used commonly and speech may be circumlocutory (ie, wordy but meaningless). Patient does not appear concerned about, or even aware of speech disorder. |
Wernicke's aphasia: caused by a lesion in or near the superior temporal gyrus. Because this part of the cortex is not located adjacent to the motor cortex, there is usually no hemiplegia.
Wernicke's aphasia commonly occurs as a result of embolic strokes. |
|
|
Where is the brain lesion?
When pt is asked to touch his or her nose with a finger, the arm exhibits tremor during movement, often more marked as the target is reached. |
INTENTION TREMOR = occurs during activity.
results from a lesion affecting the superior cerebellar peduncle (or more generally, from cerebellar hemisphere) (note: this form of tremor is sometimes mistaken for limb ataxia, but the latter has no rhythmic oscillatory component) |
|
|
where is the brain lesion?
pt exhibits a tremor that occurs when the limb is at rest. |
RESTING TREMOR - tremor apparent when arm is at rest, characteristic of Parkinson's disease
results from lesion to the Basal Ganglia This tremor may appear as a "pill-rolling" maneuver—rhythmic, opposing circular movements of the thumb and index finger. There may be alternating flexion and extension of the fingers or hand, or alternating pronation and supination of the forearm. |
|
|
Pt presents with hyperorality (a tendency to explore objects by placing them in the mouth together with the indiscriminate eating or chewing of objects and all kinds of food); hypersexuality, psychic blindness, or visual agnosia, in which objects are no longer recognized; and personality changes, usually with abnormal passivity or docility.
Where is the brain lesion? |
KLÜVER–BUCY SYNDROME, bilateral amygdala lesion
|
|
|
pt presents with personality changes - where would you suspect a brain lesion to be?
|
frontal lobe
|
|
|
Pt presents with dysarthria (dysfunction of the phonation, articulation, resonance, or respiration aspects of speech)
where is the brain lesion? |
cerebellar vermis
|
|
|
Pt presents with ataxia & acalculia
|
left parietal lobe
|
|
|
at what age do physicians begin to dose dexamethasone with, or prior, to the first dose of antibiotics in cases of suspected bacterial meningitis?
|
6mos of age
|
|
|
What drugs are most commonly used in renal disease to bind phosphate in order to prevent hyperphosphatemia?
|
Calcium carbonate & calcium acetate
DO NOT used calcium citrate |
|
|
What is the classic presentation of a pt with aspirin overdose?
|
tinnitus, starts as respiratory alkalosis, then becomes mixed respiratory alkalosis and metablic acidosis with increased anion gap
other signs: hyperthermia, altered mental status, N/V, dehydration |
|
|
What is the antidote for salicyclates
|
charcoal
NaHCO3 dialysis |
|
|
What is the antidote for
beta-blockers (or verapamil) |
atropine
glucagon calcium insuline & glucose |
|
|
What is the antidote for
digoxin |
charcoal
Digoxin FAB fragments Do NOT give calcium |
|
|
What is the antidote for
Iron |
Deferoxime
|
|
|
What is the antidote for
Copper |
Penicillamine
|
|
|
What is the antidote for
tPA, streptokinase |
Aminocaproic acid
|
|

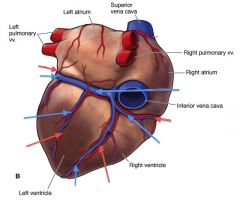
Describe the blood supply to the heart
|

see above
|
|
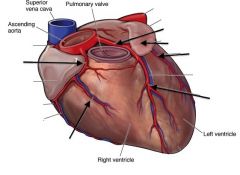
label the vessels of the heart
|
see above
|
|
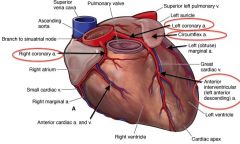
Label the vessels of the heart
|
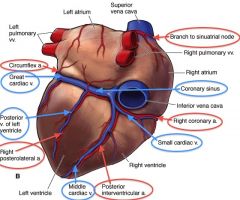
see above
|
|
|
Which coronary artery is the most common site of occlusion?
Which ECG leads correspond to this artery? |
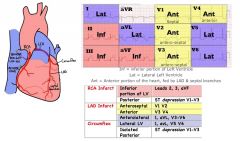
LAD
V1-V4 |
|
|
In which phase of the cardiac cycle do coronary arteries fill with blood?
|
Diastole
|
|
|
What are the equations used to find mean arterial pressure (MAP)?
|
MAP = 2/3 diastolic + 1/3 systolic
MAP = CO x TPR MAP = DBP + 1/3 Pulse Pressure (Pulse Pressure = SBP - DBP) |
|
|
What is the electrophysiological reason that a QRS complex would become widened?
|
There are a couple ways you can get a wide QRS:
1) depolarization that originates somewhere distal to the AV node , ie starting somewhere in the ventricles - and then has to travel thru both the ventricles (rather than depolarizing the ventricles at the same time) 2) delay somewhere in the interventricular conduction system - either a interventricular conduction delay or bundle branch block |
|
|
Stress testing is done as a screening test. If angina or ischemia occurs with these tests, what test should follow?
|
coronary angiogram
|
|
|
At what age should screening for hyperlipidemia begin?
|
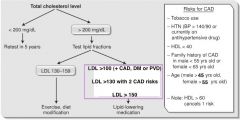
35 yrs for men
45 yrs for women earlier if pt has risk factors note: these are the ages that screening should begin, the ages in the chart reflect at which age becomes a risk factor |
|
|
At what total cholesterol value should tx begin in a pt with no risk factors?
|
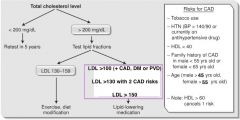
LDL>160
|
|
|
What are the two most common adverse effects of statin use, and what labs would reveal these effects?
|

hepatotoxicity - check LFTs
myopathy, myositis - check CK levels |
|
|
What lipid lowering drugs should NOT be combined?
|

statins & fibrates
they both can cause myositis and increased LFTs |
|
|
what is the first line medication to raise HDL?
|

niacin
|
|
|
ST segment elevation only during brief episodes of chest pain
dx? |
Prinzmetal angina
|
|
|
Pt is able to point to localize the chest pain using one finger
dx? |
musculoskeletal chest pain
|
|
|
Pt has CC of chest pain
On PE, there is chest wall tenderness on palpation dx? |
Musculoskeletal chest pain
|
|
|
Pt presents with rapid onset sharp chest pain that radiates to the scapula
dx? |
aortic dissection
|
|
|
Pt presents with rapid onset sharp pain in a 20yo and assoc with dyspnea
dx? |
Spontaneous Pneumothorax
|
|
|
Pt has chest pain that occurs after heavy meals and improved with antacids
dx? |
GERD or esophageal spasm
|
|
|
PT has sharp chest pain lasting hrs-days and is somewhat relieved by sitting forward
dx? |
Pericardiitis
|
|
|
Pt has chest pain made worse by deep breathing and/or motion
dx? |
Musculoskeletal pain
|
|
|
Pt has chest pain in a dermatomal distribution
dx? |
Zoster (varicella zoster virus)
|
|
|
What is the most common cause of non-cardiac chest pain?
|
GERD
|
|
|
Acute onset dyspnea, tachycardia, and confusion in a hospitalized pt
dx? |
Pulmonary Embolism (PE)
|
|
|
Pt c/o chest pain that began the day following an intensive new exercise program
|
musculoskeletal pain
|
|
|
Pt with chest pain is found to have widened mediastinum on CXR
dx? |
aortic dissection
next step: CT scan of chest |
|
|
What medications are used in the treatment of Prinzmetal's angina?
|
Nitrates
Calcium Channel Blockers (Verapamil, Diltiazem) **Avoid beta-blockers and aspirin (can exacerbate coronary vasospasm) |
|
|
What is the role of Percutaneous Transluminal coronary angioplasty (PTCA) in a pt with Coronary Artery Disease?:
(1) pt with stable angina, NO h/o MI ? (2) if medical therapy fails to improve a pt's stable anginal symptoms ? (3) pt with angina meets high-risk criteria ? (4) pt with severe CAD (such as significant proximal left main CAD, or 3-vessel CAD in pt with LVEF <50%) ? |
(1) COURAGE trial showed that angioplasty with stenting is NO BETTER than medical management alone
(2) PTCA (or CABG) is recommended if pt fails med tx (3) PTCA or CABG, before med tx, if pt is high risk (4) CABG is better than PTCA if pt has severe CAD |
|
|
What medication is used to treat Prinzmetal's angina?
|
Calcium Channel Blockers (Nifedipine, Verapamil)
|
|
|
Which patients are more likely to have atypical angina (or no angina) during an episode of cardiac ischemia?
|
Diabetics & women
|
|
|
How does nitroglycerin work acutely in a cardiac ischemic episode?
|
nitroglycerin dilates peripheral veins
decreases PREload, and decreases myocardial oxygen demand |
|
|
Why should relief of chest pain with nitroglycerin administration not be used as a diagnostic test for whether or not the chest pain is cardiac in nature?
|
Nitroglycerin will also relieve chest pain due to GERD & esophageal spasms
|
|
|
What is a helpful mneumonic to remember some of the drugs used to treat acute angina in the ER?
|
"MOAN"
Morphine Oxygen Aspirin Nitroglycerin |
|
|
Which vein is typically used in CABG?
|
Saphenous vein
|
|
|
Which medication types have a proven reduction in mortality following MI?
|
Beta-blockers
ACEI & ARBs Statins - shown to reduce mortality |
|
|
In what time frame do thrombolytics need to be given in a MI? how does this differ from the time frame in which they need to be given for a stroke?
|
MI - up to 12 hrs
Ischemic stroke - up to 3 hrs |
|
|
In addition to ST & T wave changes and new Q wave, what other EKG findings may indicate MI?
|
LBBB
Arrythmia (VTach, V Fib) |
|
|
What are specific labs ordered in pts suspected of having an MI?
|
serial cardiac enzymes : 3 sets of troponin- I, CK-MB taken every 8hrs
|
|
|
What electrolytes are important to optimize to prevent arrhythmias in pts suffering from an MI?
|
Keep K+ >4mEq/L
keep Mg+ >2mEq/L |
|
|
When is a post-MI pt at greatest risk for ventricular wall rupture?
|
4-8days post-MI
|
|
|
A pt that you treated 3wks ago for MI is now found to have fever, pericarditis, and an elevated ESR - dx?
|
Dressler Syndrome
|
|
|
Which coronary artery is involved with EKG changes in:
V2, V3, V4 |
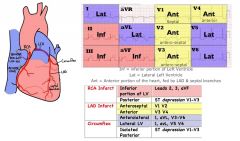
LAD - supplies anterior wall
|
|
|
Which coronary artery is involved with EKG changes in:
V1, V2, V3 |
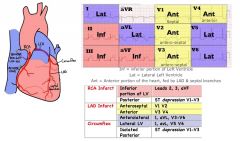
Septal Branch (distal branch of LAD) - supplies interventricular septum
|
|
|
Which coronary artery is involved with EKG changes in:
AVL, V5, V6 |
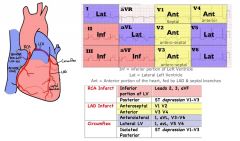
LAD or Circumflex - supplies lateral wall
|
|
|
Which coronary artery is involved with EKG changes in:
II, III, AVF |
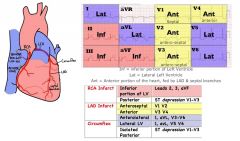
Posterior Descending Artery (PDA) or Marginal Branch - supplies inferior wall
|
|
|
HYQ: What is the most common cause of CP in a pt with sudden tearing chest pain radiating to the back?
|
Aortic Dissection
|
|
|
HYQ: What is the most common cause of death in pts with acute myocardial infarction?
|
Ventricular Fibrillation
|
|
|
Which lipid-lowering agent causes Facial flushing?
|

Niacin
|
|
|
Which lipid-lowering agent causes elevated LFTs & myositis?
|

Statins & Fibrates
|
|
|
Which lipid-lowering agents cause GI discomfort & have a bad taste?
|

Sequestrants
|
|
|
Which lipid-lowering agent have best effect on HDL?
|

Niacin
|
|
|
Which lipid-lowering agent has best effect on Triglycerides?
|

Fibrates
|
|
|
Which lipid-lowering agent has the best effect on lowering LDL/cholesterol?
|

Statins
|
|
|
Which lipid-lowering agent binds C. diff toxin?
|

cholestyramine
|
|
|
What are the recommendations for LDL levels in pts based on their CAD risk?
|
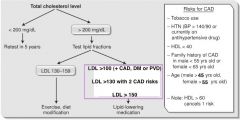
LDL <160 (if no risk factors)
LDL <130 (if pt has at least 2 risk factors) LDL <100 if pt has high risk for CAD to assess risk: Framingham Risk Assessment “A CHILD”→ Age – men > 45yr, women >55yrs Cigarette smoking Hypertension Infarct Low Levels of HDL (40mg/dL) Remember: HDL > 60 gives a bonus pt!!! Diabetes |
|
|
What is the MOA of
Streptokinase (Streptase) |
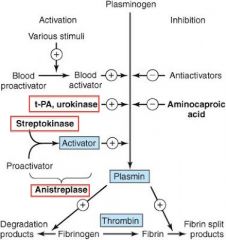
converts plasminogen to plasmin
|
|
|
What is the MOA of
Aspirin |

COX-1 and COX-2 inhibitor to prevent platelet aggregation
|
|
|
What is the MOA of
Clopidogrel (Plavix) |

blocks platelet ADP Receptor, prevents platelet aggregation
|
|
|
What is the MOA of
Abciximab? |

Glycogen IIb/IIIa inhibitor - blocks platelet aggregation
|
|
|
What is the MOA of
Tirofiban? |

Glycogen IIb/IIIa inhibitor - blocks platelet aggregation
|
|
|
What is the MOA of
Ticlopidine |

blocks platelet ADP receptor
|
|
|
What is the MOA of
Enoxaparin |
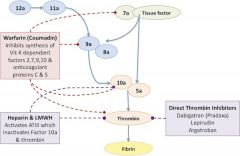
(Enoxaparin = LMWH = Lovenox)
catalyzes activation of antithrombin III |
|
|
What is the MOA of Eptifibatide?
|

Glycogen IIb/IIIa inhibitor - blocks platelet aggregation
|
|
|
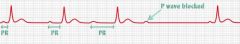
EKG shows: prolonged PR interval more than 0.2sec (5small boxes)
What type of heart block? |
1 degree heart block
|
|
|
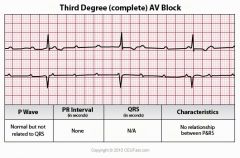
EKG shows: no relationship btw P waves and QRS
What type of heart block? |
3 degree heart block
|
|
|
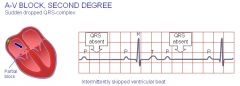
EKG shows: PR interval becomes progressively longer until a beat is dropped
What type of heart block? |
2 degree heart block, Mobitz Type 1 (Wenckebach)
|
|
|
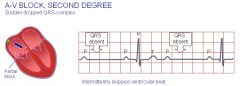
EKG shows: PR interval fixed, but with occasional blocked beats
What type of heart block? |
2nd degree heart block, Mobitz type II
|
|
|
What medications should all post-MI pts receive as outpatients?
|
- Aspirin & Clopidogrel (Plavix)
- beta-blocker (metoprolol, carvedilol) - ACEI, ARB - Statin - Aldosterone Antagonist (Spironolactone) |
|
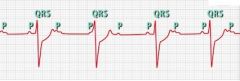
Narrow QRS not associated with p waves, rate 60
Dx? |
Third Degree Heart Block/ Junctional Rhythm
|
|
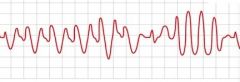
EKG shows erratic, wide QRS
Dx? |
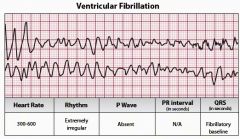
Ventricular Fibrillation
|
|
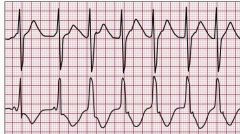
EKG show wide QRS not associated with p waves, rate >40 but <100
Dx? |
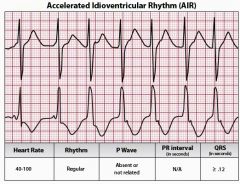
Accelerated Idioventricular Rhythm (AIVR)
Rate: Atrial not discernable, ventricular 40-100 beats/minute Rhythm: Ventricular rate regular, atrial rate not discernable P waves: Absent PRI: None QRS: > .12 May be due to: Heart disease (e.g., acute myocardial infarction, digitalis toxicity, at reperfusion of a previously occluded coronary artery), may occur During Resuscitation, Drugs (e.g., digoxin), dilated cardiomyopathy, and during Outpatient procedures (due to spinal anesthesia). |
|
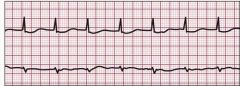
Narrow QRS not assoc with P waves, rate >100
|
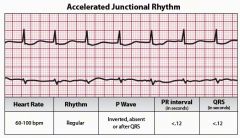
Junctional TACHYCARDIA
NOTE: the picture is acclerated junctional rhythm - it's the same except that the rate is >100bpm |
|
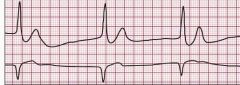
Wide QRS, not assoc with P waves, rate 20-40
|
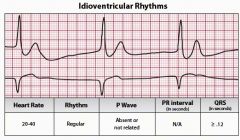
Ventricular Rhythms = Ventricular impulses come from the ventricles.
Inherent rate of ventricles is: 20-40 beats per minute can be Idioventricular Rhythm (IVR) or Ventricular Escape Rhythm |
|
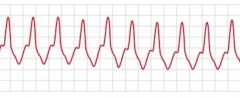
Wide QRS, not assoc with P wave, rate >100
|
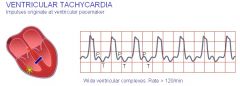
Ventricular Tachycardia (VTach)
|
|
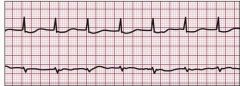
Narrow QRS not assoc with P waves, rate >60 but <100
|
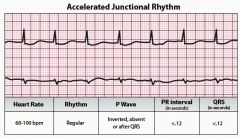
Accelerated Junctional Rhythm
|
|
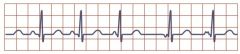
What is the diff btw a wandering pacemaker (WAP) and multifocal atrial tachycardia (MAT)?
|
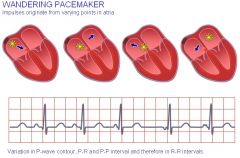
- Wandering pacemaker has atleast 3 diff P wave morphologies with a ventricular rate of <100
- Multifocal atrial TACHYCARDIA (MAT): atleast 3 diff P wave morphologies with ventricular rate >100 - Multifocal atrial bradycardia (MAB) = 3 diff P waves , vent rate <60 |
|
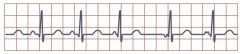
How to treat this?
|
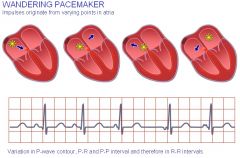
Multifocal Atrial Tachycardia (>100) or Wandering pacemaker (<100)
Acute Tx: CCB or Beta-blockers (If you have to choose between the two, go with beta-blockers) Chronic tx: catheter ablation or surgery to eliminate abnormal pacemakers |
|
|
Which heart blocks need a pacemaker?
|
2nd Degree Heart Block, Mobitz Type II
3rd Degree Heart Block |
|

How would you treat this?
|
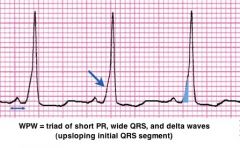
Wolff-Parkinson White (WPW) - a type of Supraventricular tachycardia due to AV reentry (often thru Bundle of Kent)
Treatment: Amiodarone (class 3) Procainamide (class 1A) Beta-blockers (Class 2) CCBs (class 4) Do NOT give Adenosine |
|
|
What endocrine disorder can cause atrial fibrillation?
|
hyperthyroidism (check TSH!)
|
|
|
A pt is in the hospital and begins to have atrial fibrillation with RVR (rapid ventricular rate). This pt has had chronic atrial fib previously. What study should be performed before the pt can be cardioverted?
what meds can be used in the meantime? |
transesophageal echocardiogram (TEE)
beta-blockers, CCBs (NON- dihydropyridines - ie Diltiazem, Verapamil, amlodipine), Digoxin |
|
|
Why must heparin be started in conjunction with Warfarin?
|
Warfarin causes temporary hypercoagulable state by depleting protein C & protein S
so heparin is used for ~3-5 days |
|
|
Type of heart block in which the PR interval is progressively lengthened with each beat until a ventricular beat is dropped:
|

2nd degree heart block, Mobitz type 1 (wenckeback)
mneumonic: Wencke is #1, and Warns you before he drops a beat |
|

Which type of Heart block?
PR interval prolonged more than 0.2 sec (5 small boxes) |
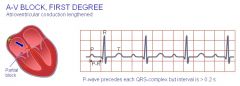
1st degree heart block
|
|
Which type of Heart block?
No relationship btw P waves and QRS complexes |
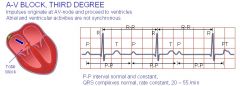
3rd degree heart block
|
|
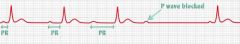
Which type of Heart block?
PR interval becomes progressively longer until a beat is dropped |
2nd degree Heart block, Mobitz Type 1 (Wenckeback)
Remember: Wenckeback is #1, and he gives you a Warning (or Wink) before he drops a beat |
|

Which type of Heart block?
PR interval is fixed, but with occasional blocked beats |
2nd degree heart block, Mobitz Type 2
|
|
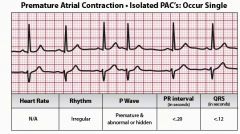
HYQ: What is the treatment for premature atrial contractions (PAC) or premature ventricular contractions (PVC)?
|
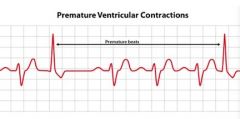
these are not pathological, observation is all that's needed
may be related to caffeine intake (cut down on the caffeine!) or hyperthyroidism PAC occurs when a site within the atria discharges before the next SA node is due to discharge PVC is when a site within the ventricle discharges early, and causes a weird looking QRS complex. PVCs become concerning when there are >3 PVCs in a minute |
|
|
HYQ: What is the DOC for acute-onset atrial fibrillation with RVR in a pt with WPW?
|
Electrocardioversion or Procainamide (Class 1A)
|
|
|
HYQ: An EKG shows complete independence of P waves and QRS complexes. What is the next step in management?
|
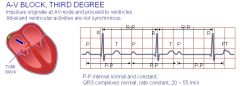
Pacemaker
(3rd degree heart block) |
|
|
HYQ: What type of heart block -
PR interval is progressively lengthened with each beat until a ventricular beat is dropped? |
2nd degree heart block, Mobitz Type 1 (Wenckebach)
|
|
HYQ: What is the DOC in paroxysmal supraventricular tachycardia?
|
- Carotid Massage (avoid in someone with carotid artery disease - you could dislodge a plaque and cause a stroke)
- Valsalva maneuvers - IV adenosine is DOC |
|
|
Which drug is avoided in Wolff-Parkinson White but used in all other forms of paroxsymal supraventricular tachycardia?
|
IV Adenosine
|
|
|
What EKG finding may indicate a very early sign of Heart Failure?
|
Left Ventricular Hypertrophy
|
|
|
Whats a normal range for the ejection fraction?
|
55-75%
|
|
|
Which type of cardiac dysfunction can be thought of as the ventricle being a floppy, wet bag trying to squeeze blood (decreased contractility)
|
systolic dysfunction
|
|
|
Which type of cardiac dysfunction is like trying to force 1.5L of Coke into a 1L bottle? (decreased ventricular compliance)
|
Diastolic dysfunction
|
|
|
What medications are important in the OUTPATIENT tx of CHRONIC CHF?
|
- ACEI/ ARBs
-Beta-blockers -Loop Diuretics - Aldosterone Antagonists (Spironolactone) - Digoxin - Aspirin |
|
|
What is the ACUTE tx for exacerbations of CHF?
|
"LMNOP"
Lasix/ Loop Diuretics Morphine Nitrates Oxygen Positioning/ Pressors |
|
|
When should a physician consider a biventricular pacemaker in a CHF pt?
|
ejection fraction <35% for >3 months
|
|
|
HYQ: Which antiarryhtmic should be avoided in pts with preexisting lung disease?
|
Amiodarone
|
|
|
When should PVCs be concerning?
|
>3 PVCs per min
- optimize Mg++ and K+ levels - consider a beta-blocker |
|
|
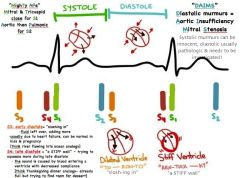
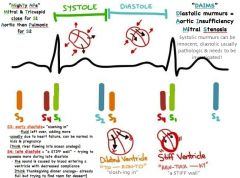
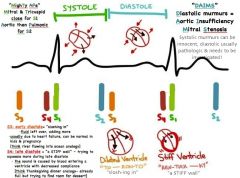
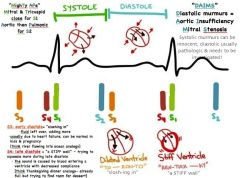
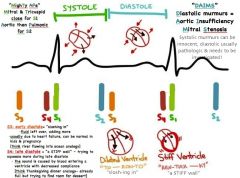
Which heart valves should blood be flowing thru during systole?
|
aortic & Pulmonic
|
|
|
What are the systolic heart murmurs?
|
aortic stenosis
pulmonic stenosis mitral regurgitation tricuspid regurgitation VSD |
|
|
What heart valves should blood be flowing thru during diastole?
|
Tricuspid & mitral
|
|
|
What are the diastolic heart murmurs?
|
tricuspid stenosis
mitral stenosis aortic regurgitation pulmonic regurgitation |
|
|
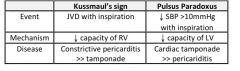
Explain the difference btw Kussmaul's sign and Pulsus Paradoxus
|
see above
|
|
|
in what condition will having the pt perform the Valsalva maneuver while auscultating the heart will increase the murmur?
In what condition will it decrease the murmur? |

INCREASE - with hypertrophic obstructive cardiomyopathy & Mitral Valve Prolapse (MVP)
DECREASE: - aortic stenosis - pulmonary stenosis - tricuspid & mitral regurgitation - aortic & pulmonic regurgitation - tricuspid & mitral stenosis QUICK HIT: Standing & the Valsalva & leg raise maneuvers diminish the intensity of ALL murmurs EXCEPT MVP & hypertrophic cardiomyopathy - these maneuvers decrease left ventricular volume SQUATTING increases the intensity of ALL murmurs except MVP & Hypertrophic Cardiomyopathy Sustained Handgrip increases the intensity of MVP murmur, but diminishes the intensity of Hypertrophic cardiomyopathy - sustained handgrip increases systemic resistance |
|
|
What 4 murmurs are possible during diastole?
|
mitral/ tricuspid stenosis
aortic/ pulmonic regurgitation |
|
|
50 yo M comes to the ER with symptoms of CHF. He is a known alcoholic and his exam is notable for having both systolic & diastolic murmurs. What is the true diagnosis of this man's disease?
|
Dilated cardiomyopathy
|
|
|
A 66yo M presents to the ER c/o CP, esp with the action of breathing. 4wks ago he had an MI, and now he is afraid he is having another one. The pt seems most comfortable sitting up & leaning forward. Altho proper w/u for acute MI must be performed, what is the likely cause of his pain?
|
Dressler's syndrome - Pericarditis
|
|
|
What will cardiac catheterization show in a pt with chronic constrictive pericarditis?
|
equal pressures in all 4 chambers
|
|
|
What is Beck's triad, what condition do you see it with, and what are the EKG findings associated with this condition?
|
Triad: hypotension, distended neck veins, distant heart sounds
Dx: Cardiac Tamponade EKG: low voltage sinus tachycardia Tx: pericardiocentesis, STAT |
|
|
Which heart murmur is assoc with syncopal episodes?
|

aortic stenosis
|
|
|
Which valve is most frequently damaged in rheumatic heart disease?
|
mitral valve
|
|
|
What is the classic appearance of the heart on a CXR of a patient with pericardial effusion?
|

enlargement of cardiac silhouette - Globular heart - "water bottle" shaped heart
|
|
|
In what scenarios might you see Kussmaul's sign (increased JVD with inspiration)
|
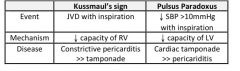
constrictive pericarditis
Restrictive cardiomyopathy R ventricular infarct massive PE |
|
|
What disease has signs of heart failure + diabetes mellitus + elevated LFTs?
|
Hemachromatosis
|
|
|
In which etiology of restrictive cardiomyopathy is the pathology reversible with phlebotomy?
|
hemachromatosis
|
|
|
What is the next step in the w/u of a low-grade systolic murmur in an otherwise healthy asymptomatic patient?
|
no further workup necessary
|
|
|
What is the next step in teh w/u of a diastolic murmur in an otherwise healthy, asymptomatic pt?
|
echocardiogram
|
|
|
Short systolic murmur at the apex that decreases with squatting and is sometimes assoc with a benign chest pain and lasts only a few seconds - Dx?
|
Mitral valve prolapse
|
|
|
When might subclinical mitral stenosis from rheumatic heart disease become clinically apparent?
|
when blood volume is increased
|
|
|
What commonly causes heart failure in young pts?
|
myocarditis
|
|
|
What is the tx for cardiac tamponade?
|
immediate pericardiocentesis
|
|
|
What medications are important in the outpt management of chronic CHF?
|
ACEI/ ARBs
Beta-blockers Loop Diuretics Aldosterone Antagonists Digoxin Aspirin |
|
|
What is the acute tx for exacerbations of CHF?
|
LMNOP
Loop Diuretics Morphine Nitrates Oxygen Position/ Pressors |
|
|
Diastolic murmur heard best at LLSB, that increases with inspiration
|

Tricuspid Stenosis
|
|
|
Late diastolic murmur with an opening snap (no change with inspiration)
|

Mitral Stenosis
|
|
|
Systolic murmur heard best in second right interspace
|

aortic stenosis
|
|
|
systolic murmur heard best in second left interspace
|

Pulmonic stenosis
|
|
|
Late systolic murmur best heard at apex
|

mitral valve prolapse
|
|
|
Diastolic murmur with a widened pulse pressure
|

aortic regurgitation
|
|
|
holosytolic murmur that is louder with inspiration at the left lower sternum
|

tricuspid regurgitation
|
|
|
holosystolic murmur heard at the apex and radiates to the axilla
|

mitral regurgitation
|
|
|
What is the treatment for premature atrial contractions?
|
observation
|
|
|
Crescendo-decrescendo systolic murmur best heart in 2nd-3rd right interspace close to sternum
|

Aortic stenosis
|
|
|
Rumbling late diastolic mumur with an opening snap
|

Mitral stenosis
|
|
|
Pansystolic (aka holosystolic) murmur best heard at the 4th-6th left intercostal spaces
|

Tricuspid regurg or VSD
|
|
|
Continuous machine-like murmur
|

PDA
|
|
|
high pitched diastolic murmur
assoc with widened pulse pressure |

aortic regurgitation
|
|
|
Explain the ABCDEs of Trauma assessment
|

|
|
|
What are the classic physical findings in a basilar skull fracture/
|
Raccoon eyes
Battle’s sign – bruising over mastoid process Hemotympanum CSF from nose (rhinorrhea) or ears (otorrhea) |
|
|
What is Cushing’s triad (4*)
|
1. Hypertension
2. Bradycardia 3. Bradypnea |
|
|
What interventions can be used to lower intracranial pressure in a head injury patient?
|

|
|
|
What is the treatment for anterior spinal cord syndrome following a traumatic injury?
|

|
|
|
A pt involved in a motorcycle accident arrives in the ER on a stretcher with his neck in a hard cervical collar. His left leg and foot are mangled. His GCS is 15 & in between his moans of pain he asks to have the uncomfortable collar removed b/c his neck isn’t bothering him. Can you remove the collar?
|
NO!
|
|
|
A patient presents to the ER after being involved in a motor vehicle collision (MVC). He doesn’t open his eyes or make any sounds, but he does withdraw to painful stimuli. What is his Galsgow coma score (GCS)? What needs to be done?
|
GCS = 6
Next step: intubation |
|
|
Another MVC victim arrives to the ER. He is able to carry on a conversation and even comment on how nice one of the nurses’ hair looks. He is able to move all of his extremities on command, and he had a significant periorbital ecchymosis and surround superficial scrapes. What is his GCS? What radiological study does he definitely need?
|
GCS = 15
Next step: noncontrast CT of head |
|
|
Yet another motor vehicle collision victim presents to the ER with a profusely bleeding wound to the leg. She is complaining loudly about her pain. What is your next step in assessment?
|
Next need to assess breathing (you know the airway is patent b/c she is talking) to assess breathing, auscultate the lungs
|
|
|
What imaging is commonly utilized in an MVC pt with no neck pain & low risk of cervical injury in order to r/o cervical fracture?
|
Cervical XRAY series – A/P, Lateral, Open-mouth odontoid
|
|
|
What imaging is required to definitely r/o C-spine fracture?
|
Cervical CT scan
|
|
|
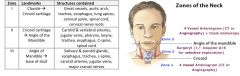
What are the different zones of the neck and structures contained in each zone?
|
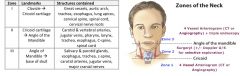
|
|
|
What work-up is indicated for a penetrating injury to the different zones of the neck when the platysma has been violated?
|
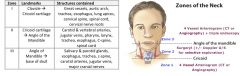
Airway, breathing, circulation
Very low threshold for intubation in these patients Asses for injury to the lung, esp in zone I injuries Oxygen, 2 large bore IVs (eg 14 gauge), type & cross blood If unstable as a result of this injury or obvious bleeding or rapidly expanding hematoma → stat to the OR for surgical exploration (Do not explore the wound in the ER). While waiting, do the following: Direct pressure to any bleeding sites If bleeding persists, consider placing a Foley cath into the wound & fill with normal saline to control bleeding If stat surgery consult is delayed & bleeding persists, consider attempt to explore wound & clamp bleeding Zone I – assess with 4 Vessel Arteriogram (CTA) Zone II – Surgical Exploration or (Doppler U/s + selective exploration) (Institution dependent) Zone III – 4 Vessel Arteriogram (CTA) + triple endoscopy |
|
|
What CXR findings might indicate a ruptured thoracic aorta?
|
Widened mediastinum, loss of aortic knob, pleural cap, deviation of the trachea and esophagus to the right, and depression of the left main stem bronchus
|
|
|
(5*) What are the signs of tension pneumothorax? What is the treatment?
|
Signs: absent breath sounds and hyperresonance to percussion (hollow sound) on the affected side, distended neck veins, hypotension
Treatment: Immediate chest tube placement If delay in chest tube placement, needle decompression on the affected side (2nd or 3rd IC space at midclavicular line or 5th IC space at midaxillary line) |
|
|
What is a flail chest and what is the classic presentation?
|
Flail chest is a free-floating portion of the chest wall that moves paradoxically to the rest of the chest wall (inward motion with inspiration) and results from 3 or more sequential rib fractures
Patient may have muscle splinting due to pain which may conceal the paradoxical motion of the chest wall Mechanism of injury is usually direct impact of the steering wheel or crush injury |
|
|
What is the treatment for a flail chest?
|
Oxygen supplementation
Close monitoring for early signs of respiratory compromise (placing an object (ie sandbag) to the affected region to stabilize the segment is no longer done due to the consequence of restricting chest expansion) BiPAP by mask or endotracheal intubation with mechanical ventilation Analgesia for pain (otherwise patient may become hypoxic from limiting breathing due to pain |
|
|
What are the initial steps in the management of an abdominal stab wound presenting to the ER?
|

|
|
|
What are the next steps in the management of blunt abdominal trauma in a patient with stable vital signs?
|
Airway, breathing, circulation (primary survey then secondary survey)
Establish IV access at two sites with large bore IVs NG tube and Foley *****CT of abdomen & pelvis Stat H&H +/- Blood type & cross |
|
|
What are the next steps in the management of a patient with blunt abdominal trauma and unstable vital signs?
|

|
|
|
What is the treatment for a retroperitoneal hematoma?
|

|
|
|
What is the next step in managing an expanding hematoma in the neck?
|
Intubation
|
|
|
A trauma patient arrives in the ER after being the driver in a high speed collision. Airway is intact, but on inspection of the chest, a portion of his chest wall seems to move in the opposite direction than it should when he breathes. What is the problem here?
|
Dx: Flail chest – suggests multiple rib fractures
|
|
|
While you were observing the odd chest movements above, the mental status and BP of the patient plummeted. Quickly you listen for chest sounds, which are absent on the anterior right side. This area is hyper-resonant to percussion, and there may be some deviation of the trachea to the left. What now?
|
Dx: Tension pneumothorax
Tx: large gauge hollow needs into the 2nd intercostal space, midclavicular line, then place chest tube |
|
|
A psychiatric patient stabbed himself in the umbilicus with a knife. The patient is tachycardic and hypotensive. The wound appears to penetrate the abdominal wall. What is the next step in management?
|
Patient needs to go to the OR – evaluate for injury to intraabdominal structures
|
|
|
A MVC victim has evidence of significant blunt trauma. On the way to the CT scanner, his BP plummets. What is the next step?
|
Bypass CT scanner & pt needs to go to the OR
|
|
|
What is the immediate treatment for a patient with a pelvic fracture?
|

|
|
|
What are the classic signs of urethral injury? What study can be used to confirm this?
|
Look for blood at the urethral meatus, a high-riding “ballotable” prostate, or absence of palpable prostate
If signs of injury → retrograde cystourethrogram to r/o injury prior to Foley catheter placement |
|
|
What is the classic sign for a bladder injury? What study can be used to confirm this?
|
Hematuria is most frequently seen in bladder injuries
A Retrograde cystourethrogram can be used to diagnose the bladder injury and determine if it is an intraperitoneal or extraperitoneal rupture If extraperitoneal rupture → Foley catheter for 10 – 14days If intraperitoneal ruptures → Urgent laparotomy for bladder repair |
|
|
What antibiotic prophylaxis should be provided for rape victims? What other prophylatic measures should also be taken?
|

|
|
|
What is the next step in the evaluation of a male trauma patient with blood at his urethral meatus & a high riding prostate? What is contraindicated?
|
Next step: retrograde urethrogram
Contraindications: do NOT attempt to place a foley! |
|
|
What should be done to evaluate an extremity trauma?
|
Full sensory & motor exam
|
|
|
What should you be looking for in a fetal ultrasound in the pregnant patient that has been involved in a MVA?
|
Placental abruption
|
|
|
Since bleeding between the fetus & mother is a concern in trauma, what actions should be taken once the patient and the fetus are stabilized?
|
Test mother’s Rh status
|
|
|
What criteria must be met before a pregnant trauma pt can be discharged from the hospital? (Hint: these are essentially the opposite of the symptoms found in placental abruption)
|
1. Contraction frequency ( < 1 every 10 min)
2. Normal fetal heart tracing 3. Absence of vaginal bleeding & abdominal pain |
|
|
What antibiotics should be given in a case of sexual assault?
|
Ceftriaxone, Azithromycin, Metronidazole
|
|
|
What are some classic signs of physical abuse?
|
Multiple bruises, inconsistent/vague history
Burns/ bruises in shapes of objects Rib, skull, long bone fractures |
|
|
HYQ: What radiographic study is used to diagnose injury to the urethra?
|
Retrograde cystourethrogram
|
|
|
HYQ: Chest trauma + hypotension + JVD + distant heart sounds → what is the next step in the management of this patient?
|
Dx: Cardiac tamponade
Tx: Pericardiocentesis; pericardial window |
|
|
HYQ: Chest trauma + hypotension + JVD + respiratory distress → what is the next step in the management of this pt?
|
Dx: Tension Pneumothorax
Next steps: needle decompression of the chest & placement of a chest tube |
|
|
HYQ: What is the next step in the evaluation of penetrating injuries to the different zones of the neck?
|
Zone 1: 4 –Vessel arteriogram
Zone 2: surgical exploration Zone 3: CT angiogram + triple endoscopy |
|
|
HYQ: What is the next step in the evaluation of penetrating injuries to the different zones of the neck?
|
Zone 1: 4 –Vessel arteriogram
Zone 2: surgical exploration Zone 3: CT angiogram + triple endoscopy |
|
|
HYQ: What interventions are effective in the management of elevated intracranial pressure?
|
Elevate head of bed to 30°
Intubate/ hyperventilate temporarily Mannitol Decompressive craniectomy |
|
|
What is the next step -
Pelvic fracture + DPL shows blood in the pelvis |
Emergent laparotomy
|
|
|
What is the next step :
Pelvic fracture + DPL shows urine in the pelvis |
Urgent laparotomy
|
|
|
What is the next step
Pelvic fracture + DPL shows nothing + hemodynamic instability |
Angiography with possible embolization
|
|
|
What is the next step
Blunt abdominal trauma + unstable vital signs + FAST shows fluid in pelvis |
Emergent Laparotomy
|
|
|
What is the next step
Blunt abdominal trauma + unstable vital signs + FAST shows no fluid in pelvis |
Angiography with possible embolism
|
|
|
What is the next step
Blunt abdominal trauma + unstable vital signs + FAST inconclusive |
DPL
|
|
|
What is the next step
Blunt abdominal trauma + stable vital signs |
CT of abdomen & pelvis
|
|
|
What is the next step
Abdominal stab wound + hypotensive or signs of peritonitis |
Emergent laparotomy
|
|
|
What additional studies can be performed in the case of a stable patient with an abdominal stab wound that penetrated the peritoneum?
|
Diagnostic laparotomy best
DPL Upright CXR Diagnostic Ultrasound Contrast CT of the abdomen & pelvis |

