![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
481 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Antecubital fossa |
Most common site for venipuncture? |
|
|
|
Gauge 21 & 20 Respectively |
Most common gauge used in syringe method? What is the gauge used for hemostasis or coagulation studies? |
|
|
|
median cubital vein |
Most common vein for venipuncture because it is largest and most stable |
|
|
|
Cephalic vein |
only visible vein for obese patients? |
|
|
|
Evacuated tube system |
method of blood collection that is done in a closed system and the most common method of venipuncture? |
|
|
|
None |
Red glass anticoagulant? |
|
|
|
Clot activator |
Red plastic anticoagulant |
|
|
|
Tripotassium EDTA in liquid form. Other name: SEQUESTRENE |
What is the lavender glass anticoagulant? |
|
|
|
Chelates (binds) calcium |
Mechanism of EDTA? |
|
|
|
Yellow (SPS), Blue (Citrate), Red (No Anticoag), Green (lithium heparin), Lavender (Sequestrene), Gray (sodium fluoride |
Order of Draw for normal venipuncture? |
|
|
|
Sodium citrate 3.2% |
what is the anticoagulant for Blue top? And what concentration is mostly preffered? |
|
|
|
Fe, Aldosterone, Cortisol, ACTH |
Analytes that are increased during morning ? |
Morning F.A.C.A |
|
|
Ketoacidosis |
Hallmark of DM type 1? |
|
|
|
Type 1 |
DM with absolute insulin deficiency? |
|
|
|
DM type 2 |
Relative insulin deficiency? |
|
|
|
8-10 hours ; 16 hours |
In OGTT a patient should fast within ______ but not more than _____ hours. |
|
|
|
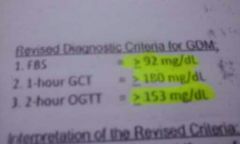
75 grams |
Glucose load for adults? |
|
|
|
1.75 g/ kg body weight |
Glucose load for children? |
|
|
|
100 g |
Glucose load for pregnant women? |
|
|
|
< 6.5 |
Glycosylated Hemoglobin (HBA1C) Normal value? |
|
|
|
2-3 months |
HBA1C measures average glucose levels for how many months? |
|
|
|
Glycated albumin |
Other name of fructosamine? |
|
|
|
2-3 weeks |
Fructosamine measures average glucose level for how many weeks? |
|
|
|
Phospholipid and unesterified cholesterol (free cholesterol) |
Lipids considered as amphoteric? |
|
|
|
3Fatty acids + 1 glycerol |
composition of triglyceride? |
|
|
|
1 glycerol , 2 fatty acids , 1 phosphate group |
composition of phospholipid? |
|
|
|
HDL |
Apo - A1 for? |
|
|
|
LDL , VLDL |
Apo B-100 for? |
|
|
|
Chylomicrons |
Apo B48 for? |
|
|
|
VLDL, LDL, HDL |
Apo E? |
|
|
|
Lipoprotein (a) |
Apo (a) for? |
|
|
|
75 Grams |
Glucose load for 2 Hour Glucose test? |
|
|
|
100 Grams |
Glucose load for 3 Hour glucose test? |
|
|
|
140-200 mg/dl |
Impaired Random Glucose (Pre-diabetic) |
|
|
|
100-126 mg/dl |
Impaired Fasting Blood Sugar (pre-diabetic) |
|
|
|
70-100 mg/dl |
Normal values of Fasting Blood Sugar? |
|
|
|
< 140 mg/dl |
Normal values of Random Blood Sugar |
|
|
|
50-55 mg/dl |
At what amount of glucose could you say that patient is hypoglycemic? |
|
|
|
Fasting Venous plasma |
Standard specimen for glucose determination? |
|
|
|
8-10 Hours |
Fasting time for FBS? |
|
|
|
10-15% |
Whole blood glucose is lower by _____ % than others |
|
|
|
7 mg/ dl/ hour |
Glucose is metabolized at a room tenperature at the rate of? |
|
|
|
2 mg/dl/ Hour |
At 4 degree celsius Glucose decreases by the rate of? |
|
|
|
Chylomicron |
what lipoprotein transports triglycerides exogenously from outside the body to inside? |
|
|
|
VLDL |
What transports triglycerides from the liver to the cells? |
|
|
|
LDL |
What transports cholesterol and has the highest cholesterol content? |
|
|
|
HDL |
Transports cholesterol reversely from cell to liver? |
|
|
|
Beta VLDL |
Floating Beta Lipoprotein found in Type Iii Hyperlipoproteinemia |
|
|
|
Lp (a) |
Sinking pre-beta lipoprotein which increases the risk of atherosclerosis? |
|
|
|
Phosphomolybdate; Phosphomolybdenum blue |
Folin - Wu is an Alkaline copper reduction method. What is the reducing agent used? End product reaction? |
|
|
|
Arsenomolybdate ; Arsenomolybdenum blue |
Reducing agent for Nelson-Somogyi and end product result? |
|
|
|
Hexokinase method |
What type of the enzymatic methods of determining glucose is the reference method? |
|
|
|
Glucose Oxidase method |
What enzymatic method is best for determining B-D-Glucose? |
|
|
|
Abell-Kendall Method |
Reference method for cholesterol measurement? |
|
|
|
Free cholesterol |
What does Abell-Kendall method measures? |
|
|
|
Green |
When Liebermann - Buchard reagent reacts with cholesterol it produces what color? |
|
|
|
Acetoacetic acid (20%) |
The only ketone body detected in serum is? |
|
|
|
150 g for 3 consecutive days |
In the OGTT test, patient is asked to consume at least how many grams of carbohydrate for how many days? |
|
|
|
FBS, Aldosterone/Renin, Triglycerides, Gastrin, Lipid profile, Insulin, GTT |
Analytes affected by fasting |
F.A.T.G.L.I.G |
|
|
Lactic Acid, Ammonia, Blood Gas |
These analytes if not chilled will result to decrease pH and pO2 |
Ice = L.A.B |
|
|
Sodium |
in case of marked hemolysis this analyte may be decreased |
|
|
|
L/S Ratio |
Test that assesses fetal lung maturity? |
|
|
|
Glucose, Fructose, Galactose |
what are the monosaccharide sugars? |
|
|
|
Oligosacharrides. Example ; Dextrins |
These are sugars with 3-10 units. Samples of which are? |
|
|
|
Glycosidic bonds |
What bond connects sugar units? |
|
|
|
Cellulose |
What is the most abundant Carbohydrate in the planet? |
|
|
|
Salivary Amylase (" Ptyalin" ) |
What enzyme is produced by the parotid gland and what is it's other name? |
|
|
|
Glucose |
The only carbohydrate that could be used directly for energy? |
|
|
|
EMP, HMP, and Glycogenesis |
3 pathways glucose could go to after entering the cell? |
|
|
|
Glycolysis |
A process in which glucose is metabolize to become pyruvate (aerobic) or lactate (anaerobic) for energy prod'n |
|
|
|
Gluconeogeneseis |
Production of G6PD from Noncarbohydrate sources is called? |
|
|
|
Hexose Monophosphate Pathway |
What pathway produces Reduced NADPH to decrease glutathione? |
|
|
|
Glycogenolysis |
Breakdown of glycogen into glucose for energy is called? |
|
|
|
Glycogenesis |
Conversion of glucose to glycogen? |
|
|
|
Lipogenesis |
Conversion of Carbohydrates to fatty acids? |
|
|
|
Lipolysis; Ketone Bodies |
Breakdown of fatty acids?End product of these process? |
|
|
|
Insulin and glucagon |
2 Hormones that control glucose metabolism? |
|
|
|
Beta cells of the pancreas |
What cells produces Insulin? |
|
|
|
Alpha cells of the pancreas |
What cells produces Glucagon? |
|
|
|
Increase glucose in Blood |
What is the stimulus for production of insulin |
|
|
|
C peptide |
what is removed from Proinsulin to become insulin? |
|
|
|
Cortisol |
What hormone helps in the gluconeogenesis and is produced in the adrenal cortex? |
|
|
|
Catecholamines |
What hormone helps in the glycogenolysis that is produced in the adrenal medulla? |
|
|
|
Somatostatin |
what hormone produced by the delta cells of the pancreas inhibits both the secretion of insulin and glucagon? |
|
|
|
Thyroid hormone |
What hormone also helps in glycogenolysis but is produced in the thyroid gland? |
|
|
|
Growth Hormone |
What hormone inhibits insulin?This is produced in the amterior pituitary |
|
|
|
Glycogenesis & Glucose uptake; Glycogenolysis & Lipolysis |
Insulin's action Increases ____________ & __________ also it Decreases ____________& _____________ |
|
|
|
Normal ratio : 1:1 (B:A) Extreme Ketoacidosis : 6:1 (B:A) |
Normal B- Hydroxybutyrate to acetoacetate ratio? What happens in DM with extreme ketoacidosis? What is the ratio? |
|
|
|
Fasting statE: TAG is high in VLDL Non Fasting State: TAG is high in CHYLOMICRON |
Where is TAG found in fasting states & non fasting states? |
|
|
|
Bacterial Meningitis |
Decreased CSF glucose (<40 g/dL) and increased WBC (Neutrophil) is a sign of what? |
|
|
|
TYPE I GSD: Von Gierke (Assctd w/ hyperlipidemia) |
Most common Glycogen Storage disorders? |
|
|
|
Adults : 40-70 Children: 60-80 g/dL |
Normal value of CSF Glucose in adults and children? |
|
|
|
B-cell (Pancreas) Funxn |
C peptide levels are meausred by immunoassay what function does it measure? |
|
|
|
21 & 23 gauge: 1 to 1.5 inches Butterfly infusion: 1/2 or 3/4 length |
Length of Needle for 21 & 23 gauge Length of needle for butterfly infusion? |
|
|
|
HLA DR3 HLA DR4 |
What HLA is associated w/ DM type I? |
|
|
|
Chlorhexidine gluconate |
Disinfectant used for blood cultures of infants? |
|
|
|
70% Alcohol added with iodophor |
what is the most common way to disinfect blood culture puncture site? |
|
|
|
Precision study -Run two controls twice for 10-20 days |
First step in method evaluation is? |
|
|
|
Mean |
The only measure of systematic error is? |
|
|
|
Galactose-1-phosphate-uridyl-transferase (most common)
GALE & GALK |
Defect in Galactosemia
Hint: 3 enzymes |
|
|
|
CV |
Percentile expression of mean? |
|
|
|
Glucose Lactate & Alcohol Sodium flouride prevents decrease of alcohol while blocking further glycolysis of lactate |
Gray top tube could be used to test what? |
|
|
|
Shewhart Levy Jennings |
Dot chart? Is? |
|
|
|
60 mmHg |
if blood pressure cuff is to be used as a tourniquet it is inflated up to? |
|
|
|
Yoden chart -Low and High standard values of other laboratories |
Twin Plot? |
|
|
|
Fructose Kinase deficiency Fk converts Fructose to Fructose-1-phosphate |
Defect in Essential Fructosuria? |
|
|
|
Deteriorating reagents -It is a gradual loss of reliability |
Main cause of trend? |
|
|
|
silica particles - 15-30 min gel separators 30 min clot activators - 5 min red stoppered tube - 60 min |
give clotting time of each
silica particles gel separators clot activators red stoppered tube |
|
|
|
Improper calibration Change in reagent |
Main cause of Shift? |
|
|
|
20 days consecutive |
If you have a new reagent how many days will you observe it? |
|
|
|
Fructose-1,6- Biphosphate-aldolase-B-activity in kidneys, liver and intestine |
defect in Hereditary Fructose intolerance? |
|
|
|
Random Error / Imprecision |
What mainly affects Precision? |
|
|
|
Systematic Error |
What mainly affects Accuracy? |
|
|
|
in IS/BB it interferes with some reactions In TDM it absorbs some drugs causing FALSE LOW RESULTS |
Gel separators couldn't be used in IMMUNOLOGIC REAXNS & BLOOD BANK why? also couldn't be used in TDM? Why? |
|
|
|
Control values |
What is mainly plotted in the dot chart? |
|
|
|
Borosilicate glass |
most common glassware used for the reason thst it has high degree of thermal resistance? Strain point 501 degrees |
|
|
|
Fructose-1,6-biphosphate Glucose generation by liver through gluconeogenetic precursors lactate & glycerol |
defect in Fructose-1,6-biphosphate deficiency |
|
|
|
Blown out type |
Pipet with two etched rings? |
|
|
|
Inversely proportional -The higher the SD the greater the dispersion of values (LOW precision) -The lower the SD the lower the disepersion of values (HIGH precision) |
Relation of SD to Precision? |
|
|
|
Ostwald Folin |
pipet for viscous fluids with etched ring? |
|
|
|
Distilled Water - TD Mercury - TC |
Mediums used to calibrate TC & TD |
|
|
|
Positive air displacement pipet |
what pipet does not require pipet tips for use? |
|
|
|
Air displacement pipet |
pipet wherein piston does not come in contact with the fluid? |
|
|
|
Children <2.0 mm Adults < 2.5 mm |
Depth of incision for capillary puncture of adults and children? |
|
|
|
Production of TAG from FA by the liver 1.)Synthesis of VLDL (contains Apo B100 & apo E) 2.) VLDL --- LPL---> IDL 3.) IPL (Removed by liver) through Apo E or! IPL (Converted to) LDL 4.) Ch rich LDL particles got by the liver or tses for steroid synthesis or part of cell membranes |
Describe endogenous pathway |
|
|
|
lateral plantar surface of heel surface |
most common site for arterial capillary puncture? |
|
|
|
Lipids rich in Fatty Acids TAG, Fatty Acids |
Lipids that are a source of energy are? |
|
|
|
1.)HDL gets Cholesterol from tse and either reintroduce for continued metabolism or excretion 2.)LCAT esterifies chole in HDL3 to HDL2 3.) This faction could be transferred to VLDL to participate in metabolism of membrane and steroid synthesis or excreted into Bile |
Describe Reverse cholesterol pathway |
|
|
|
glucose phosphorus potassium |
if blood isn't separated with blood for 30 minutes these analytes might be unstable |
|
|
|
Increase in Potassium Decrease sodium in plasma or serum |
what happens when there is a shift in electrolytes? |
|
|
|
Icteric sample Hemolyzed sample |
What mainly affects the hexokinase method? |
|
|
|
Short Chain (4-6) Medium Chain (8-12) Long Chain (> 12)
Branched: Unsaturated (Double bond) (TRANS) Unbranched: Saturated (CIS) |
Fatty acids are classified according to length of chain
branched or unbranched. Give the classification |
|
|
|
CETP (Cholesterol ester transfer protein) -GETS TAG from apoB in exchange of GIVING cholesterol ester -Def. of this protein leads to large cholesterol laden HDL -Connects forward & reverse cholesterol transport pathways |
Another pathway of HDL? |
|
|
|
Ascorbic acid Uric Acid |
Hexokinase unlike Glucose oxidase method, is not affected by: |
|
|
|
Lipoprotein Lipase (LPL) |
Hydrolyzes TAG breaks it into FA & Glycerol is the role of? |
|
|
|
500mg /dL |
Plasma glucose increases by how much in 10% contamination of 5% dextrose? |
|
|
|
Hepatic Lipase |
Hydrolyzes TAG & phospholipids from HDL Hydrolyzes lipids on VLDL & IDL Both are roles of? |
|
|
|
300 mg/dL |
Ketone test is requested when plasma glucose reaches? |
|
|
|
False increase |
Bleach could cause?____ in glucose oxidase method? |
|
|
|
LCAT Lecithin Cholesterol Acyl Transferase |
Catalyzes the esterification of cholesterol from HDL Enables accumulation of Chole into Chole Ester in HDL Are roles of? |
|
|
|
Endothelial lipase |
Hydrolyzes phospholipids and TAG in HDL? |
|
|
|
ABCA1 ATP-Binding Cassette Protein A1 |
For efflux of cholesterol from peripheral cells into HDL |
|
|
|
Apolipoprotein |
What do you call the protein part of a lipoprotein? |
|
|
|
Its amphipathic helix |
What does apolipoprotein use to bind to lipids? |
|
|
|
MAJOR -Chylomicron -VLDL -LDL -HDL MINOR -IDL -Lp (a) / Lipoprotein A |
What are the major & minor lipoproteins? |
|
|
|
CM <0.95 kg/L VLDL 0.95 - 1.006 kg/L LDL 1.019-1.063 kg/L HDL 1.063- 1.210 kg/L |
Provide the density of each Major lipoprotein? |
|
|
|
Chylomicron Fnxn: Transports exogenous / dietary TAG to liver, muscle & fat depot |
Lipoprotein that is largest but least dense Produced from dietary fat |
|
|
|
apo B48 apo A1, apo C, apo E |
Apolipoproteins of Chylomicrons |
|
|
|
Pre Beta Lipoprotein |
Another name for VLDL? |
|
|
|
1.) TAG & Cholesterol is taken up in the intestine 2.) Chylomicrons are formed and released in the lymph nodes and blood 3.) Chylomicrons release TAG in adipose tse as they circulate 4.) LPL liberates Fatty Acids from TAG thereby reducing the skze kf chylomicrons to become remnants 5.) Remnants are taken up by the liver 6.) Free Fatty Acids are taken up by muscle and adipose tse |
Explain Dietary or exogenous pathway? |
|
|
|
VLDL |
It is a lipoprotein secreted by the liver Fnxn: transports endogenous TAG from the liver to muscle, fat, tse |
|
|
|
The amount of glucose consumed is proportional to the glucose concentration |
What is the principle of polarographic glucose oxidase? |
|
|
|
Apo B100 Apo C & Apo E |
Apolipoprotein of VLDL? |
|
|
|
Non fasting specimen B-VLDL px |
Friedewald equation is not suitable for? |
|
|
|
The amount of NADPH generated is proportional to the amount of glucose present Mutarotase is added to shorten the amount of reaction time |
In glucose dehydrogenase method what is the principle? What is added to shorten the time to reach equilibrium? |
|
|
|
LDL Fnxn: transports CHOLESTEROL to the peripheral tse |
-Lipoprotein synthesized in liver -Major end product of Catabolism of VLDL -Major source of CHOLESTEROL of tse. |
|
|
|
Plasma TAG ----------------- 5 |
How to measure VLDL? |
|
|
|
LDL |
most cholesterol rich in lipoproteins and therefore most atherogenic? |
|
|
|
LDL |
primary target if cholesterol lowering therapy and primary marker for congestive heart dse? |
|
|
|
Beta lipoprotein |
Another name for LDL? |
|
|
|
Apo B100 & apo E |
Apolipoproteins of LDL? |
|
|
|
HDL |
Smallest lipoprotein but most dense Fnxn: Transports cholesterol from tissues to the liver and more cardioprotective |
|
|
|
True |
The phospholipid part of HDL is more important than its protein or cholesterol part true or false? |
|
|
|
Apo A1 & apo A2 Apo C |
Apolipoproteins of HDL? |
|
|
|
LDL |
What lipoprotein is measured in Coronary Heart Disease? or what lipoprotein is watched out for? |
|
|
|
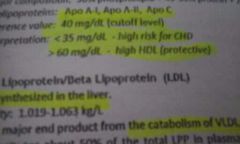
Reference value: 40 mg/dL Interpretation: <35mg/dL (High Risk for CHD) >60mg/dL (high HDL = Protective) OK! |
Ref. value for HDL? Interpretation of HDL? |
|
|
|
IDL |
VLDL remnant? |
|
|
|
Apo E III |
Defective clearance if IDL in type 3 hyperlipoproteinemia is probably due to deficiency of? |
|
|
|
Apo B100 Density: 1.006- 1.019 mg/dL |
Maj. apolipoprotein of IDL? Density? |
|
|
|
Lp (a) |
Sinking pre-B lipoprotein? |
|
|
|
When there is insulin shock or there is hyperglycemic ketonic coma |
When is Random Blood Sugar requested? |
|
|
|
Between 24 and 28th week of gestation |
Screening for gestational diabetes should be performed when? |
|
|
|
Type 2 DM -Since C peptide is a by product of production of insulin and insulin is still produced at type 2 |
At what type of DM is C peptide detectable? |
|
|
|
Nephelometry |
Machine that best measures Ag-Ab reaction? |
|
|
|
LOW Na HIGH K |
Describe the electrolyte imbalance of Na & K in DM? |
|
|
|
SD ---- x 100 Mean |
Formula of CV? |
|
|
|
5-hr OGTT -hypoglycemic "DIP" often is not seen not until after 3 hrs |
Diagnostic test for HYPOGLYCEMIA? |
|
|
|
180 mg/dL |
GLUCOSURIA occurs when the plasma levels exceeds? |
|
|
|
Acetyl coA |
Ketosis develops in DM when there is excessive synthesis of? |
|
|
|
6:1 |
In severe DM the ratio of B-hydroxybutyrate to acetoacetate becomes? |
|
|
|
Yes 6-8 HRS Fasting |
Does amino acid collection need fasting if yes how many hours? |
|
|
|
2 Hr OGTT 75 grams glucose load |
Screening test & Diagnostic test for GDM? |
|
|
|
Revised criteria for GDM? |
|
|
|
Dilantin and pentamidine |
Drugs that promote b cell dysfunction |
|
|
|
Thiazide and glucocorticoids |
Drugs that impair insulin reaction |
|
|
|
2 Hr Post Prandial Blood Sugar 2 Hr OGTT |
measurs how well fhe body metabolizes glucose? |
|
|
|
Janney-Isaacson (Single Dose) |
most commonly used GTT method? |
|
|
|
Intravenous Glucose Tolerance Test (IGTT) -0.5 g of glucose/kg body weight (given within 3 min.) |
Tolerance test for DM px w/ gastrointestinal disorders? |
|
|
|
GAD65 - Assctd w/ adults IAA (Insulin Auto Antibody) - Assctd w/ children |
autoantibodies found in DM type 1? |
|
|
|
DM Type 1 |
Brittle Diabetes? |
|
|
|
DM type 2 |
Stable Diabetes, Ketone Resistant Diabetes |
|
|
|
7 mg/dL |
Venous blood glucose is ___ LOWER than capillary & arterial blood glucose because of tse metabolism |
|
|
|
60% |
CSF Glucose is approximately ___ of the plasma cncentration |
|
|
|
true |
RBC and WBCs contribute greatly to glucose metabolism that is why more than 30 minutes of not separating serum from blood is an unacceptable sample for fbs true or false? |
|
|
|
Collect FBS Give glucose load (drink w/in 5 min) Collect after 1 hr, 2hr, 3hr respectively |
Procedure for OGTT for pregnant woman? |
|
|
|
Collect only the FBS & 2 HR sample |
Procedure for OFTT for non pregnant, adult etc |
|
|

|
Category of OGTT? |
|
|
|
Modified folin wu methd |
Benedicts method is a modified? |
|
|
|
Citrate or Tartarate |
Benedicts test uses what as a stabilizing agent? |
|
|
|
Nelson Somogyi |
Reference chemical method of measurement of glucose? |
|
|
|
HBA1C (Glycated Hemoglobin) |
A reliable method in monitiring long term glucose control? |
|
|
|
2-3 months |
HBA1C reflects ave. blood glucose level over the previous? ___ months |
|
|
|
> or = 6.5% on at least two occassions methods should meet National Glycohemohlobin Standardization Program & DCCT method |
Before an HBA1C be diagnostic of DM it should meet what standards? |
|
|
|
Fructosamine (Glycated albumin) Useful for monitoring DM individuals w/ Chronic hemolytic anemia & Hgb Variants |
Useful for monitoring short term glucose about ___ wks |
|
|
|
IDA & Old RBC have HIGH HBA1C disorders with Shortened RBC lifespan have LOW HBA1C |
What should you consider when measuring HbA1C? |
|
|
|
Low plasma albumin (< 30 g/ L) low fructosamine |
Fructosamine should not be measured in cases of? |
|
|
|
205-285 umol/L |
NV of Fructosamine? |
|
|
|
Glomerular filtration rate |
Is a measure of the clearance of normal molecules that are not bound to proteun and are freely filtered by the glomeruli neither reabsorbed or secreted by the tubules |
|
|
|
Glomerular Filtration Rate |
It is considered as the overall indicator of the level of kidney function? |
|
|
|
150 L |
How many liters of glomerular filtrate is produced daily? |
|
|
|
Clearance |
The removal of substance from plasma into urinr over a fixed time? |
|
|
|
INVERSELY PROPORTIONAL |
Plasma concentration is _____ proportional to clearance |
|
|
|
B2-Microglobulin -Readily filtered by the glomerulus Increased in: Renal failure, MM, RA, SLE & HIV |
Plasma protein that is a light chain compinent of the HLA? Needed in the production of CD8 Cells |
|
|
|
remember: Haptoglobin is DECREASED in Intravascular hemolysis while transferrin is NORMAL or INCREASED in IDA |
remember: Haptoglobin is ____ in Intravascular hemolysis while transferrin is ___ or ___ in IDA |
|
|
|
Albumin & Transferrin |
Considered as Negative Acute Phase reactants? |
|
|
|
Transferrin |
Major contributor to B2 region in Electrophoresis? |
|
|
|
Siderophilin |
Another name for transferrin? |
|
|
|
Heme : Hemopexin Hemoglobin: Haptoglobin Iron: Transferrin |
Give the transporter fof each:
Heme Hemoglobin Iron |
|
|
|
Pseudoparaproteinemia |
In severe IDA there is INCREASED Transferrin which results to? |
|
|
|
Accumulation of iron in apoferritin or in histiocytes |
Transferrin is decreased in? |
|
|
|
Fibrinogen |
Most abundant coagulation factor? |
|
|
|
True -Fibrinogen coats cells making them sediment faster in clumps |
High levels of fibrinogen in plasma = INCREASE ESR? True or false? |
|
|
|
True -Exists as non functional precursors however |
Complement is naturally found in the plasma true or false? |
|
|
|
Complement C3 |
What form of complement is most abundant in the serum? |
|
|
|
DIC , Hemolytic anemia |
Complement is DECREASED in? |
|
|
|
CRP C-Reactive Protein |
A member of the pentraxin protein family Binds to the C-polysaccharide of the pneumococcus |
|
|
|
C Reactive protrein |
Highest plasma protein in terms of inflammation? |
|
|
|
Myoglobin |
Heme protein found in skeletal & cardiac muscles that transports oxygen from Hgb to contractile cells? |
|
|
|
Fnxn: Regulator of actin & myosin Present in: Cardiac & skeletal muscles Significance: MOST IMPORTANT MARKER FOR AMI 3 types: TROP I, C, T TROP C: Binds Ca that regulate muscle contractions TROP I & T: Almost absent in NORMAL serum |
What are the troponins? |
|
|
|
Elevates: after 1-3 Hrs Peak: 5-12 Hrs Normalize: 18-30 Hrs |
Myoglobin elevates when during AMI? |
|
|

|
Formula for clearance |
|
|
|
Inulin clearance |
What is the reference method for GFR? |
|
|
|
Continous IV infusion and requires timed urine collections - Too hassle Primary dose: 25mL of 10% inulin Continous infusion: 500mL of 1.5% inulin solution Reference values: M: 127 mL/min F: 118 mL/min |
Inulin clearance is not routinely done because of? |
|
|
|
Radioactive markers -125 Iothalamate -99mTc-DTFA -51cr EDTA (Don't need urine spx) -Non Labelled Isothalamate |
other substitutes for inulin clearance? |
|
|
|
Creatinine clearance |
Most commonly used clearance test? A measure of completeness of 24 hr urine collection? In normal states its excretion is almost equal to its production |
|
|
|
Advantage: Freely filtered by glomeruli and NOT reabsorbed Disadvantage: Is SECRETED by tubules |
advantage and disadvantage of creatinine clearance? |
|
|
|
Muscle mass |
Excretion of creatinine is directly related to? |
|
|
|
M: 85-125 mL/min F: 75- 112 mL/min |
reference values for creatinine clearance? |
|
|

|
Cases of increased creatinine and decrease creatinine? |
|
|
|
Urea Clearance Disadvantage: It is reabsorbed especially in high urine osmolarity & high urea conc. Could be used: in advanced renal failure since as renal function declines reabsorption of ures declines. Wheareas tubular secretion of creatinine increases Note: The faster the urine flow the less reabsorption of urea |
Urea clearance's disadvantage? when is it sensitive? |
|
|
|
it is reabsorbed |
Disadvantage of csystatin C? |
|
|
|
-Blood Urea Nitrogen -Creatinine -Blood Uric Acid |
Tests that measure Renal Blood Flow? |
|
|
|
Troponin T |
Significant marker for unstable angina (chest pain at rest) assesses early & late AMI |
|
|
|
-Excretion Test -Concentration test |
Tests for tubular function? |
|
|
|
Elevate: 3-4 Hours Peak: 10-24 Hours Normalize: 7 days (Could last up to 10-14 days) |
During AMI when will Trop T elevate? |
|
|
|
Blood Urea Nitrogen |
major end product of protein (dietary) and amino acid catabolism? this is 45% of total NPN? |
|
|
|
True |
The concentration of urea is expressed only by the nitrogen content of urea true or false? |
|
|
|
2.14 x BUN = Urea (mg%) |
To obtain the concentration of Urea from BUN? |
|
|
|
True -Since Trop T is also elevated in muscular dystrophy & renal disease it is not specific |
Trop I is more cardiac specific than Trop T true or false? |
|
|
|
8-23 mg/dL (2.9-8.2 mmol/L) |
Reference value of BUN? |
|
|
|
BUN: Creatinine 10:1 20:1 |
BUN:Creatinine ratio? |
|
|
|
BUN |
good indicator of nitrogen intake and state of hydration? |
|
|
|
Elevates: 3-6 Hrs Peaks: 12-18 Hrs Normalizes: 5-10 days |
Trop I elevates during? |
|
|
|
Improperly timed specimen |
The most common cause of error in clearance tests? |
|
|
|
Fluoride & citrate |
___ & ___ both inhibits urease and affects BUN? |
|
|
|
Isotope Dilution Mass Spectrometry (IDMS) |
Reference method for measurement of BUN? |
|
|
|
B type-Natriuretic Peptide |
Protein that is sensitive to ventricular & diastolic dysfunction? Diagnostic of CHD? |
|
|
|
Cystatin C Increased in: renal disease |
Protein that inhibits cysteine proteinase inhibitor determines GFR proposed as alternative test for Creatinine clearance test |
|
|
|
1.) Alcoholism, Chronic Renal Failure, Steroid treatment - Prealbumin 2.)Cystic Fibrosis - Albumin 3.)Inflammation, Pregnancy, Contraceptive use- A1-Anti Trypsin 4.)Neural tube disorder & Down Syndrome -A1 Fetoprotein 5.)Stressful conditions, myoglobinuria - Haptoglobin 6.)Nephrotic syndrome,Diabetes, liver dse- A2 Macroglobulin 7.)Renal Failure, MM, RA,SLE,HIV- B2- Microglobulin 8.)Hemochromatosis, IDA - Transferrin 9.)Inflammatory conditions- Complement 10.)Acute Rheumatic fever, AMI, RA, Gout, Bacterial & viral infxn - CRP |
Review: Give the INCREASED Plasma protein in each situation 1.) Alcoholism, Chronic Renal Failure, Steroid treatment 2.)Cystic Fibrosis 3.)Inflammation, Pregnancy, Contraceptive use 4.)Neural tube disorder & Down Syndrome 5.)Stressful conditions, myoglobinuria 6.)Nephrotic syndrome,Diabetes, liver dse 7.)Renal Failure, MM, RA,SLE,HIV 8.)Hemochromatosis, IDA 9.)Inflammatory conditions 10.)Acute Rheumatic fever, AMI, RA, Gout, Bacterial & viral infxn |
|
|
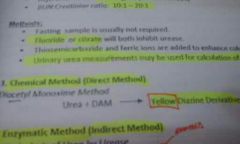
End product: Yellow |
Direct method of measuting BUN? |
|
|

Urea + Urease = NH3(ammonia) + CO2 |
Enzymatic method or indirect method to measure BUN? |
|
|
|
1.)Poor Nutrition - Prealbumin 2.)Active Nephrotic Syndrome - Albumin 3.)Emphysematous pulmonary dse & juvenile hepatic cirrhosis- A1-Antitrypsin 4.)Intravascular hemolysis & hemoglobinuria- Haptoglobin 5.)Wilson's Disease, Menkes Dse - Ceruloplasmin 6.)Extensive coagulation - Fibrinogen 7.)DIC, Hemolytic anemia & malnutrition - Complement |
Review: Give the plasma protein DECREASED in each situation 1.)Poor Nutrition 2.)Active Nephrotic Syndrome 3.)Emphysematous pulmonary dse & juvenile hepatic cirrhosis 4.)Intravascula hemolysis & hemoglobinuria 5.)Wilson's Disease, Menkes Dse 6.)Extensive coagulation 7.)DIC, Hemolytic anemia & malnutrition |
|
|

|
Comditions with increased and decreased BUN? |
|
|
|
Creatinine |
End product of muscle metabolism derived from creatine (a-methyl guanidoacetic acid) |
|
|
|
Creatinine: Not affected by protein diet ; not easily removed by dialysis BUN: Affected by protein diet & easily removed by dialysis |
Advantage of creatinine to BUN |
|
|
|
Creatinine -As gestation progresses more creatinine id excreted by the fetus in the amniotic fluid (2mg/dL) |
a measure of fetal kidney maturity? |
|
|
|
Male: 0.9-1.3 mg/dL Female: 0.6-1.1 mg/dL |
Reference value of creatinine? |
|
|
|
icteric and hemolyzed |
in measuring creatinine avoid?__ &___ spx |
|
|
|
Isotope dilution mass spectrometry |
Reference methid for measurement of creatinine? |
|
|
|
Chemical Method = Direct Jaffe Method Princple: Creatinine + Alk. picrate rgt = Red Orange tautometer of creatinine picrate |
Principle of Chemical method for Creatinine measurement |
|
|
|
Reference value of HDL? |
|
|
|
Type 2 Hyperlipidemia / Familial Hypercholesterolemia |
Type of lipid disorder where there is defect of LDL receptor? |
|
|
|
Dysbetalipoproteinemia / Type 3 Hyperlipidemia |
Lipid disorder where there is rich B-VLDL There is presence of abnormal broad band between VLDL & LDL? Presence of apo E2/2 (Rare form of apo E) |
|
|

|
Reference value of LDL? |
|
|
|
<1:1 Diabetes insipidus >1:1 Glomerular Disease |
Urine:Serum osmolality of <1:1 and >1:1 means |
|
|
|
Osmolal gap |
The difference between measured and calculated plasma osmolality is? |
|
|
|
Molecular studies |
Pink top and white top tubes are used for? |
|
|
|
Enzymes |
proteins that hastens chemical reactions measured in terms of activity and NOT by absolute values |
|
|
|
Enz conc. -The higher the conc. the faster the reaxn Substrate conc. -The more subst. the faster the reaxn Cofactors -Nonprotein entities that bind to enz for reaxn to occur Inhibitors -Decrease enz. activity Isoenzymes -Same reaxn diff amino acid sequence -Enz activity is enhance by fractionizing isoenz. Temperatures -37 degrees (Optimal) -40-50 degrees (Denatured enz) -60-65 degrees (Inactivated enz) Hydrogen Ion Conc. for pH -pH 7-8 (Optimal) Storage - -20 degrees (Preservation of enz for longer period) -2 to 8 ideal storage temp for substrate and coenzymes -RT ideal for LDH (LD4&5) Hemolysis -Increased enz conc. Lactescence or milky spx -Decreased enz conc. |
Factors that affect activity of enzymes? |
|
|
|
Coenzyme -Organic compound (Secobd substrates) -Essential to achieve absolute enz activity -Example: NAD & NADP Activators -Inorganic ions -Alters the spatial configuration of the enzymes for proper substrate binding -Examples: Ca, Mg, Cl,Zn Metalloenzyme -Inorganic attached to molecule -Example:Catalase, cytochrome oxidase |
What are thr cofactors? |
|
|
|
Competetive -Substrate and inhibitor compete gor active site -Addition of substrate makes it reversible -Dilution of serum lessens the inhibitor Noncompetitive -The inhibitor binds to another site DOES NOT compete with the substrate in the active site -Addition of substrate DOES NOT stop inhibition Uncompetitive -Inhibitor binds to enz-substrate complex -Addition of substrate ONLY INCREASES inhibition |
Types of inhibitors |
|
|
|
E.C 3.1.3.2 - ACP E.C 3.1.3.1 -ALP E.C.2.6.1.2- ALT E.C.2.6.1.1.- AST E.C.3.4.15.1- Angiotensin Converting Enz E.C.1.1.1.49- G-6-P-D E.C.1.1.1.27 - LDH E.C.3.1.3.5 - 5' Nucleotidase |
E.C 3.1.3.2? E.C 3.1.3.1?
E.C.2.6.1.2? E.C.2.6.1.1.?
E.C.3.4.15.1?
E.C.1.1.1.49?
E.C.1.1.1.27?
E.C.3.1.3.5? |
|
|

|
Classofication of enzy? |
|
|
|
Active site- where substrate binds Allosteric site- other sites than actibe site where receptor may bind |
What is active site & allosteric site? |
|
|
|
Apoenzyme(enzyme) + Prosthetic group (coenzyme) = Holoenzyme |
What is a holoenzyme |
|
|
|
Emil Fisher |
Who proposed the lock and key theory? |
|
|
|
Kochland proposed this theory -Substrate binds to active site |
Who proposed induce fit theory?What is it? |
|
|

|
Reference value of LDL? |
|
|
|
abetalipopriteinemia (Bassen-Kornzweig syndrome) |
Lipid disorder where there is a defective apo B synthesis? VLDL, LDL, Chylomicrons are absent in plasma Presence of acanthocytes Fat malabsorption due to fat solunle vitamins |
|
|
|
Hypolipoproteinemia |
apo B deficiency Decresead LDL & TC? |
|
|
|
Niemann Pick Disease |
Accumulation of sphingomyelin in the bone marrow, spleen & lymph node |
|
|
|
Tangier's Disease |
Rare disease where there is complete absence of HDL due to mutation of ABCA1 Gene on chromosome 9 |
|
|
|
Type 1 Hyperlipidemia / Familial Hyperchylomicronemia -Since LPL not only hydrolyzes TAG but also converts chylomicrons to chylomicron remnant its deficency leads to accumulation of chylomicrons in plasma |
LPL Deficiency leads to? |
|
|
|
LCAT Deficiency |
LCAT gene mutation leads to? |
|
|
|
Fisher eye |
What is a milder form of LCAT deficiency? |
|
|
|
Tay Sachs Disease |
deficiency of hexosaminidase A which results to accumulation of sphingolipids in the brain? |
|
|
|
Chylomicron Retention Disease (Andersen's Disease) |
Deficiency of apo B48 is? |
|
|
|
Chylomicrons : 80-95% TAG LDL: 6-8% Free Cholesterol HDL: 40-55% Protrein |
Values you need to remember in the chemical composition of Lipoproteins? |
|
|
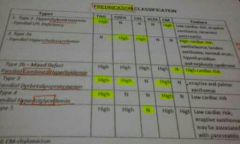
Type 1 "Chylomicronemia" HIGH: TAG & CM Type 2a: "Cholesterolemia" HIGH: LDL & Cholesterol Type 2b: "COMBINED" ONLY NORMAL: CM Type 3: "DYSBETALIPO" HIGH: VLDL, TAG, Cholesterol Type 4: "TRIGLYCEREMIA" HIGH: TAG, VLDL Type 5: ONLY NORMAL: LDL |
Summarize Fredrickson classification of Hyperlipidemias |
|
|
|
High HDL = Low CHD High LDL = High CHD |
Relation of HDL & LDL to CHD? |
|
|
|
Immunohlobulins & vWF |
Only proteins that are not synthesize by the liver is? |
|
|
|
Requires automated equipment Principle: Serum id mixed w/ alkaline picrate and the rate of change in absorbance is measured between 2 points Interferences: a-keto acids & cephalosporins |
What is kinetic jaffe method? |
|
|
|
Interference: Negative interference are Bilirubin & Catecholamines 2 ENZYMATIC METHODS 1.)Creatinine Aminohydrolase (Creatininase) CK Method -Not widely used because requires large amount of enz d because requires large amount of enz Enz in order: Creatinine aminohydrolase, CK, PK, LDH End product: Lactate + NAD 2.)Creatinase-H2O2 Method -Potential to replace jaffe -Not affected by acetoacetate & cephalosporins Enz used: Creatininase, Creatinase, Sarcosine oxidase, peroxidase Endproduct: Benzoquinonemine dye (Red) |
what are the eenzymatic methods to measure creatinine?Interferences in measurement? |
|
|
|
Isotope dilution mass spectrometry |
Still the reference method for measurement of Creatinine? |
|
|
|
True |
Plasma creatinine conc. is assctd with Abn. renal fnxn but is relatively insensitive since it will only increase when there is > 50% renal deterioration true or false? |
|
|
|
Azotemia -ELEVATED conc. of nitrogenous substances like UREA & CREATININE in blood Uremia -MARKED ELEVATION in plasma urea and other nitrogenous substance -accompanied by ACIDEMIA & ELECTROLYTE IMBALANCE (K elevation) -Anemia (NORMOCHROMIC & NORMOCYTIC) -BURR CELLS & ELLIPSOIDAL CELLS |
Disease related with renal blood flow? |
|
|

|
Formula for calculating VLDL? |
|
|
|
PRE-RENAL (Low GFR) -DIMINISHED glomerular filtration w/ NORMAL renal fnxn Causes: Dehydration (High BUN plasma crea is N), Shock, congenital heart disease RENAL(Low GFR) -Damaged w/in kidneys -Striking BUN level, slow rising plasma crea, anemia & electrolyte imbalance Causes: Acute/ Chronic renal dse, glomerulo nephritis POST RENAL(Low GFR) -Urinary tract obstruction -Urea is HIGHER than crea due to back diffusion of ure to the circulation Causes: Renal calculi(nephrolithiasis) cancer of GUT |
Types of azotemia? |
|
|

Low BUN:Crea - Usually affected by problems in Protein, liver(producer of protein), and in reabsorption of Urea High BUN:Crea (Increased crea) - usually affected by damaged kidneys since defect in renal fnxn increases crea High BUN:Crea (N crea) -If crea is unaffected or kidneys are unaffected |
Causes of Low BUN: Crea High BUN:Crea (N crea) High BUN:Crea (increased Crea) |
|
|
|
Primary Structure |
Structure of proteins that is linear and determines the identity, binding capacity, and recognition ability |
|
|
|
<20 ug/ min |
Normal excretion rate of albumin present in urine? |
|
|
|
Purine (adenine & guanine) catabolism -Formed from xanthine by the action of xanthine oxidase in the liver and intestine |
Blood Uric acid comes from? |
|
|
|
secondary structure |
winding of the polypeptide chain |
|
|
|
Glomerular or Tubular dyafunction |
Proteinuria (> 0.5g/day) usually results from? |
|
|
|
Monosodium Urate |
A weak acid at pH 7.4 >95% of Blood Uric acid exists as? |
|
|
|
Catabolism of INGESTED nucleoproteins Catsbolism of ENDOGENOUS nucleoproteins Transformation of ENDOGENOUS purine nucleotides |
Blood uric acid is derived from 3 sources what are they? |
|
|

|
Reference value (uricase) |
|
|
|
Tertiary Structure |
Responsible for the 3D structure of proteins Folding pattern Responsible for physical and chemical properties |
|
|
|
Quaternary Structure |
Association of 2 or more polypeptide chain to form a functional protein molecule |
|
|
|
Lipoprotein X -Apo C & Albumin |
Abnormal lipoprotein found in obstructive jaundice & LCAT deficiency -Specific and sensitivr indicator of cholestiasis |
|
|
|
Albumin - Only single polypeptide chain |
Which protein has no Quaternary structure? |
|
|
|
HYPERURICEMIA 1.)Gout -Deposition of Uric acid in joints -Birefringent crystals ib synovial fluid is definitive -High risk for nephrolithiasis 2.)increased nuclear metabolism -Leukemia, lymhpoma, polycythemia,multiple myeloma, hemolytic & megaloblastic anemia -allopurinol drug (for treatment) 3.)Chronic renal dse - decreased GFR, imcreased tubular secretion -BUA >10 mg/dL could cause urinary calculi 4.)Lesch Nyhan Syndrome(Inborn error of Purine metabolism) -Deficiency of hypoxanthine guanine phosphoribosyl transferase (HGPT) HYPOURICEMIA 1.) Fanconi's syndrome 2.) Hodgkins 3.) Wilson's Disease |
Disease related to Blood Uric Acid? |
|
|
|
Spx: Fasting sample is preferred for diagnosis Anticoagulant NOT used: Potassium oxalate Maj. Interferences: Bilirubin and Ascorbic acid |
When measuring BUA what are the px prep? Major interferences? Anticoagulant that SHOULD NOT BE USED |
|
|
|
Simple proteins |
This are types of proteins that when polypeptide chains are hydolyzed they yield only amino acid |
|
|
|
Fibrous (E.g Fibrinogen, Collagen, Troponin) Globular (E.g Hgb, Plasma proteins, enz, peptide hormones) - Compact no space for water inside |
2 shapes of simple proteins? |
|
|
|
Conjugated proteins |
Type of protein where there is a combination of protein (apoprotein) & non protein moiety (prosthetic group) |
|
|
|
Lamellar body |
Phospholipids is produced by pneumocytes type II as? |
|
|
|
Sphingomyelin |
The only phospholipid not produced from glycerol but instead from sphingosine is? |
|
|
|
Sphingomyelin |
wjatvis an essential component of cell membranes (RBC and Nerve sheath) |
|
|
|
Live and spleen |
In Niemmann pick disease (Lipid storage disorders) sphingomyelin accumulates where? |
|
|
|
Lecithin/Phosphatidyl choline -70% Sphingomyelin- 20% Cephalin- 10% |
give the forms of phospholipids and their corresponding percentage |
|
|
|
1.)Chemical method Principle: Reduction-Oxidation (RED-OX)
Uric acid + Phosphotungstic acid ---- NaCN/ Na2CO3---> Tungsten blue + Allantoin + CO2
a.)NaCN = Folin, Brown, Newton, Benedict
b.)Na2CO3= Archibald, Henry, Caraway
2.)Enzymatic method Principle: Uric acid has a maximum peak of absorption 293mm allantoin does not. The DECREASE in absorbance is proportional to the concentration of uric acid
Uric Acid + O2 ---Uricase--> Allantoin + CO2 + H2O |
2 methods od measuring BUA? |
|
|

L/S of > or = 2
|
Mature lung function correlates at an L/S ratio of what? |
|
|
|
Isotope dilution mass spectrometry (IDMS) |
The reference method for uric acid measurement? |
|
|
|
< 39 weeks |
Fetal lung maturity should be done in ____ wks |
|
|
|
Anabolism - Synthesis Catabolism - Breakdown |
What is anabolism & catabolism? |
|
|
|
Nitrogen balance |
A balance between catabolism & anabolism? |
|
|
|
NEGATIVE Nitrogen balance |
When CATABOLISM exceeds anabolism it is called? |
|
|
|
POSITIVE nitrogen balance |
When ANABOLISM exceeds catabolism this is called? |
|
|
|
Transthyretin |
Another name for prealbumin? |
|
|
|
True |
Sphingomyelin serves as the reference method during the 3rd trimester of pregnancy because its concentration is constant as opposed to lecithin true or false? |
|
|
|
-Prealbumin, Albumin -Globulin -A1-Antitrypsin, A1-Fetoprotein, -Hemopexin, Haptoglobin, Ceruloplasmin -A2-macroglobulin -Transferrins, complements, C-Reactive Protein -Immunoglobulins |
Summarize the plasma proteins? |
|
|
|
2 days |
Half life of transthyretin?(prealbumin) |
|
|
|
1st : Albumin 2nd: Prealbumin |
Most abundant protein in CSF? 2nd? |
|
|
|
1st: Albumin 2nd: Globulin |
Most abundant protein in serum? |
|
|
|
EXCRETION TEST 1.) Para amino hippurate test (Diodrast test) 2.)Phenolsulfonthalein dye test CONCENTRATION TEST 1.)SG 2.)Osmolality Direct method: Freezing point Vapor pressure Indirect method: 1.86 x Na + Glucose + BUN ----------- ------ 18 2.8 |
What are the test that measures tubular function ? |
|
|
|
Transport T4 & Retinol (Vit.A) Used to detect malnutrition Confirm if spx is really CSF |
Functions of Prealbumin? |
|
|
|
18-45 mg/dL |
Reference value for Prealbumin? |
|
|
|
Loss of concentrating ability of kidney Equivalent to glomerular filtrate |
SG of 1.010 means? |
|
|
|
-A general transport protein -Maintains osmotic pressure -Reservoir for circulating amino acids -Negative acute phase reactant |
Functions of albumin? |
|
|
|
There are radiographic dyes present |
High SG >1.030 means? |
|
|
|
Cystic Fibrosis |
Albumin is a sensitive, highly prognistic marker in cases of? |
|
|
|
1.005-1.030 |
Reference value of SG? |
|
|
|
Active Nephrotic Syndrome |
Lowest plasma albumin levels are seen in? |
|
|
|
3.0-5.0 g/dL |
Reference value of Albumin? |
|
|
|
SG- Measures total number And Mass of particles
Osmolality- only measures the number of solute particles present/kg of solvent (moles/kg solvent) Osmolality More accurate than SG in measuring tubular funxn |
Difference between SG and Osmolality? |
|
|
|
Absolute specificity: One enz one substrate one reaction Group Specificity: One enz. combine with All substrate in a chem. gr. Bond Specificity:enz. reacting w/ specific chemical bonds |
Enzyme kinetics Provide description of each: Absolute specificity: Group Specificity: Bond Specificity: |
|
|
|
Zero Order Kinetics: Reaction rate depends on Enzyme concentration
First Order Kinetics: Reaction rate DIRECTLY PROPORTIONAL to Substrate concentration |
What is:
Zero Order Kinetics
First Order Kinetics |
|
|
|
Fixed Time- Reactants combined, reaction proceeds for a designated time, reaction is stopped and measurement is made Continous monitoring/Kinetic assay- Multiple measurements of change in absorbance. More preferred |
2 general methods to measure enzymatic reactions? |
|
|
|
International Unit (IU) umol of substrate/ min Katal Unit mole of substrate/min |
2 Units for expressing enzymatic activity? |
|
|
|
CHANGES IN: Substrate concentration Product concentration Coenzyme concentration |
Enzymes are measurd in terms of? |
|
|

|
Causes of elevated plasma enzyme levels |
|
|
|
Michaelis Menten Constant |
What is Km? in enzyme |
|
|
|
In order to achieve zero order kinetics you must have >99Km An enz. DO NOT alter the FREE ENERGY or DIRECTION of the reaction but it alters the ENERGY OF ACTIVATION by forming a metastable intermediate the ES COMPLEX |
An enzyme accelerates the rate of reaction
A constant change in absorbance per unit of time only occurs in zero order kinetics
In order to achieve zero order kinetics you must have ____Km
An enz. DO NOT alter the ___ or ____ of the reaction but it alters the ______ by forming a metastable intermediate the ES COMPLEX |
|
|
|
enzymes are used as REAGENTS |
In first order kinetics the enzymes are used as ____ to measure a specific analyte |
|
|
|
Substrate or Product |
Endpoint measurement determines the conc. of ___ or ____ at a specific time after addition of the sample (bedside glucose testing) |
|
|
|
Liver - in healthy sera ALP is derived here Bone- High in children, growth, adults older than 50, increases w/ osteoblastic activity Placental- In normal pregnancy increased ALP is detected 16-20 wks Intestinal- Depends on blood secretor or H gene status B and O has high intestinal ALP A and AB has low intestinal ALP |
Major sources of ALP? |
|
|
|
The liver Especially in obstructive jaundice |
If ALP is elevated the main contributor faction is? |
|
|
|
The liver Especially in obstructive jaundice |
If ALP is elevated the main contributor faction is? |
|
|
|
Pagets Disease (Osteitis deformans)
-Bone ALP isoform B1x was detected in serum of Dialysis patients |
Highest elevation of Bone ALP occurs in what condition? |
|
|
|
Regan -Most heat stable ALP (65 Degrees in 30 minutes) -Inhibited by: Phenylalanine Nagao -Variant of regan ALP -inhibited by: L-Leucine & Phenylalanine |
2 carcinoplacental ALP |
|
|
|
Electrophoresis -Most anodal: Bone and Liver ALP -Least anodal: Intestinal ALP -Use NEURAMIDASE & WHEAT GERM LECTIN to separate Bone and liver ALP Heat Fractionation/Stability Test -56 degrees for 10-15 min -Most Heat Stable: Placental ALP -Most Heat Labile: Bone ALP Decreasing order of stability: Placental, intestinal, liver, bone Chemical Inhibition Test -Usage of Phenylalanine, 3M Urea, Levamisole Inhibited by Phenylalanine reagent: Placental & Intestinal ALP Inhibited by 3M Urea: Bone ALP Inhibited by Levamisole: Bone and Liver ALP |
methods to measure ALP? |
|
|
|
Bowers and Mc Comb
-pH environment of 10.15 - read at 405nm -Since Phosphorus is innhibitory to ALP, AMP Buffer is added to bind phosphorus |
Most specific method of measuring ALP, IFCC recommended method? |
|
|
|
Zinc is a component Of ALP and Magnesium is the enzyme activator |
___ is a component of ALP and ___ is the enz activator |
|
|
|
Diffirentiating whether a tumor in pineal body is a pinealoma or a germ cell tumor |
Placental Alkaline Phosphatase is useful in? |
|
|
|
Diffirentiating whether a tumor in pineal body is a pinealoma or a germ cell tumor |
Placental Alkaline Phosphatase is useful in? |
|
|
|
Liberates inorganic phosphate from organic phophate ester with the concomitant production of alcohol |
Function of ALP? |
|
|
|
Same with ALP except it is active at pH 5.0 |
Function of ACP? |
|
|
|
Presence of seminal fluid |
ACP > 50 IU/L indicates what? |
|
|
|
-For detection of Prostate carcinoma -After surgical treatment of prostate cancer ACP falls faster than PSA . -Also used in forensic studies during rape cases -Seminal fluid (>50 IU/L) ACP activity could persist up to 4 days |
Diagnostic significance of Measuring ACP? |
|
|
|
Thymolphthalein monophosphate is the specific subatrate of choice for quantitative endpoint reaxnA-Naphthyl PO4 is preferred for continoud monitoring methods |
____ is the specific subatrate of choice for quantitative endpoint reaxn
____ is preferred for continoud monitoring methods |
|
|
|
ACP activity in bones is assctd w/OSTEOCLASTS ALP activity in bones is assctd w/ OSTEOBLASTS |
ACP activity in bones is assctd w/____
ALP activity in bones is assctd w/___ |
|
|
|
Transfer of amino acid from Aspartate to a-keto acids w/ formation of oxaloacetate & glutamate |
Funxn of AST? |
|
|
|
Cytoplasm -More predominant form in the serum Mitochondrial |
2 isoenzyme of AST? |
|
|
|
Major Tissue Source: Cardiac Tissue, Liver and Skeletal Muscle Other Sources: Kidney, Pancreas, RBC |
Tissue sources of AST? |
|
|
|
AST on AMI Rise: 6-8 Hours Peak:24 hours Elevate: 5 days |
With regards to AMI what is thr rising, peak and normalizing point of AST? |
|
|
|
-Evaluation of myocardial infarction, hepatocellular disorders, and skeletal muscle involvement -Used for monitoring therapy w/ potentially hepatotoxic drugs a result of more than three times the upper border of normal should signal cessation of therapy |
Diagnostic significance of AST |
|
|
|
Karmen Method -Uses malate dehydrogenase (MD) and monitors change in avsorbance at 340 nm |
Method used to measure AST? |
|
|
|
Tranfer of amino group from Alanine to a-keto glutarate with the formation of glutamate and pyruvate Highest concentration in liver more liver specific than AST |
Funxn of ALT? |
|
|
|
Maj. tse source: LIVER Other sources: Kidney, pancreas, RBC, Heart, skeletal muscles, lungs |
Tissue source of ALT? |
|
|
|
Coenzyme: pyridoxal phosphate (vit. B6) Hemolysis should be avoided, increases AST 10x |
Aminotransferases (AST & ALT) requires what as coenzyme? |
|
|
|
Acute hepatitis |
Highest elevation of Transaminases (AST &ALT) Is seen in? |
|
|
|
>1.0 |
In acute hepatitis the De Ritis ratio? (ALT:AST) |
|
|
|
At end stage cirrhosis the transaminase levels are LOW due to massive tissue destruction |
At end stage cirrhosis the transaminase levels are ___ due to massive tissue destruction |
|
|
|
Breakdown of Starch and glycogen |
What is the function of Amylase? |
|
|
|
Amylase |
Smallest enzyme in size? |
|
|
|
S-type (ptyalin) P-type(amylopsin) |
Earliest pancreatic marker -Amylase P3- is the most predominant pancreatic amylase isoenzyme So what are the 2 isoenzymes of amylase? |
|
|
|
Maj. tse source: Acinar cells of the pancreas and the salivary glands Other tissue source: Adipose tse, Fallopian tubes, small intestine, and skeletal muscles |
Tissue sources of amylase? |
|
|
|
Acute pancreatitis (AMS Reaxn) Rise: 2-12 hours Peak:24 hours Normalize:3-5 days |
AMS levels in acute pancreatitis? Rise, peak and normalize when? |
|
|
|
Parotitis |
What is another name for salivary gland inflammation? |
|
|
|
SG- Measures total number And Mass of particles
Osmolality- only measures the number of solute particles present/kg of solvent (moles/kg solvent) Osmolality More accurate than SG in measuring tubular funxn |
Difference between SG and Osmolality? |
|
|
|
Urea, chloride, sodium |
3 most prevalent solute excreted in concentration tests? |
|
|
|
Total protein - Serum Albumin = Serum Globulin |
How to compute for the serum globulin? |
|
|
|
Solute |
Osmolality is more of a measure of? |
|
|
|
Plasma: 275-295 mOsm/kg 24hr urine: 300-900mOsm/kg |
Reference value of Osmolality in plasma and 24 hr urine |
|
|
|
An INCREASE in osmolality (solute) DECREASES freezing point and vapor pressure |
An INCREASE in osmolality (solute) _____ freezing point and vapor pressure |
|
|
|
1:1 |
Normal ratio of Urine:Serum osmolality? |
|
|
|
Glucose; stored as Glycogen |
The only carbohydrate to be used directly for energy or stored as _____ |
|
|
|
insulin |
Glucose enters the muscle cells with the aid of? |
|
|
|
Pyruvic acid Lactic acid Acetylcoenzyme A |
Glucose metabolism generates what 3 products? |
|
|
|
Carbon dioxide Water Adenosine Triphosphate |
Oxidation of glucose generates what products? |
|
|
|
Sucrose |
The most common nonreducing sugar? |
|
|
|
Endocrine: Release Glucagon, Insulin, Somatostatin (From Alpha, Beta, Delta Cells of the islets of langerhans respectively) Exocrine: Release of Pancreatic amylase to break ingested complex carbohydrates |
Pancreas as an endocrine does what?As an exocrine? |
|
|
|
true |
In early cirrhosis Total protein becomes normal because the increase of globulin makes up for the loss of albumin true or false? |
|
|
|
2.3-3.5 g/dL |
Ref. value of globulin? |
|
|
|
Fat Muscle Liver |
insulin is primarily stored where? |
|
|
|
High glucose levels in blood |
Trigger of insulin release? |
|
|
|
TLC followed by densitometric quantitation |
What instrumentation is used to measure L/S ratio? |
|
|
|
Increase Glycogenesis Lipogenesis Glycolysis Decrease Glycogenolysis |
Functions of Insulin? |
|
|
|
25-50 pg/mL |
Fasting plasma glucagon are normally ? |
|
|
|
A1-Antitrypsin |
Plasma protein that neutralizes trypsin like enzymes Major inhibitor of protease activity : Prevents self destruction of tissues 90% of the A1-globulin band |
|
|
|
Hydroxyl group of the A-ring |
Cholesterol is amphipathic what is its hydrophilic part? |
|
|
|
Estrogen |
Transport and excretion if cholesterol is facilitated by? |
|
|

|
Reference value of cholesterol? |
|
|
|
A1 Fetoprotein |
Most abundant protein in fetal serum? |
|
|
|
13th wk of Gestation |
Peak period of A1-Fetoprotein? |
|
|
|
7th to 8th month of pregnancy |
A1-Fetoprotein is detectable in serum of mothers during? |
|
|
|
Progestin,Estrogen,Aldosterone Glucocorticoids, mineralocorticoids |
Cholesterol is the precursor of the 5 major steroids: |
|
|
|
Neural tube disorders Down syndrome |
Diagnostic significance of AFP? it could detect? |
|
|
|
Hemopexin |
Binds heme? |
|
|
|
Cholesteryl ester- 70% Free cholesterol- 30% |
How much of the cholesterol is a Cholesterol ester and how much is a free cholesterol? |
|
|
|
Haptoglobin |
Binds hemoglobin and prevents its loss together with iron in the urine |
|
|
|
Ceruloplasmin |
Binds copper? Imparts blue color to protein? |
|
|
|
Esterified by: LCAT (Lecithin Cholesterol Acyl Transferase) -transfer if fatty acids from lecithin to cholesterol which results in the formation of lysolecithin and cholesterol ester
Re-esterified by: ACAT |
Cholesterol ester undergoes esterification by ____ Excess cholesterol is re esterified by ___ |
|
|
|
Wilson's Disease |
Kayser Fleisher rings is found where? |
|
|
|
A2-Macroglobulin |
Largest major non imunoglobulin protein in plasma? |
|
|
|
Apo-A1 |
What is the activator of LCAT? |
|
|
|
Hydrophobic & Hydrophilic (Phospholipid, Free Cholesterol) - Are located at the surface of lipoprotein Hydrophobic (Cholesterol ester) - Are located inside the lipoprotein |
Principle of the arrangement of lipids in the lipoproteins? |
|
|
|
True |
Total cholesterol is rather measured than its forms true or false? |
|
|
|
Cholesterol & HDL |
Only lipid component not affected by fasting state is? |
|
|
|
Dehydration and Oxidation of cholesterol to form a colored compound |
Principle of the Chemical method of measuring cholesterol? |
|
|
|
Liebermann buchard ¤ End product: GREEN color ¤Rgt: MONOsulfonic acid
Salkowski Reaction ¤ End Product: RED color ¤Rgt: DIsulfonic acid |
2 chemical methods of measuring cholesterol? |
|
|
|
SHOULD NOT BE: Hemolyzed: Falsely increase Icteric: 5-6%mg Increase (Biliribin absorbs light at 500 nm) |
Precautions in Total cholesterol measurement? Specimen should not be ___ & ___ |
|
|
|
Ascorbic acid = FALSE DECREASE |
Ascorbic acid usually causes false ___ in Enzymatic methods of measurement for glucose & cholesterol |
|
|
|
Measure the amount of HYDROGEN PEROXIDE produced |
Currently the most common method of quantifying cholesterol oxidase is measuring the amount of ____ produced |
|
|
|
Abell-Kendall , Levy, and Brodie Method 1.)Hydrolysis w/ alcoholic KOH 2.)Hexane extraction 3.)Liebermann-Burchardt color reagent |
reference method for enzymatic measurement of cholesterol is? |
|
|
|
LPL - Lipoprotein lipase Epinephrine & Cortisol |
Breakdown of TAG is facilitated by? |
|
|
|
Glomerular proteinuria / Albuminuria |
most common type and serious type of proteinuria? |
|
|
|
12-14 hours |
Fasting requirement of TAG? |
|
|

|
Reference value of Triglyceride? |
|
|
|
Glomerular proteinuria - albuminuria Tubular proteinuria -low molecular mass proteins due to defective reabsorption Overload proteinuria -hemoglobinuria, myoglobinuria, BJP Post renal proteinuria -Potein from UTI caused by infxn, bleeding or malignancy |
Types of proteinuria? |
|
|
|
Triglycerides & Colesterol -Fasting TAG > or = 200 mg/dL is indicative of risk for coronary heart disease because of atherogenic VLDL remnants |
___ & ____ are the most important lipids in the management of coronary heart disease |
|
|
|
B-VLDL -Has Density of VLDL but migrates to LDL (B region) in electrophoresis -There is accumulation of IDL because of failure to fully convert VLDL to LDL |
"abnormally migrating B-VLDL" "Floating B lipoprotein" "VLDL Rich in Cholesterol" Are all descriptions of? |
|
|
|
B-VLDL |
Found in Type 3 htperlipoproteinemia or dysbetalipoproteinemia? |
|
|
|
LDL -It is only estimated through FRIEDEWALD EQUATION |
Between TC, TAG, HDL & LDL what IS NOT directly measured? |
|
|
|
Microalbuminuria |
An early indicator of glomerular dysfunction and precedes nephropaty assctd w/ DM type 1? |
|
|
|
ALBUMIN: CREATININE 30:300 ug/mg -2 out of 3 spx w/in a 3-6 month period with abnormal findings |
A patient is said to have a microalbuminuria if he/she has an albumin: crea ratio of? |
|
|
|
Ultracentrifugation & Enzymatic cleavage |
Lipemic samples could be pretreated by? |
|
|
|
Total Cholesterol - HDL = Non HDL |
Formula for lipoproteins? |
|
|
|
Colorimetric method (Van Handel & Zilversmith) Fluirometric method (Hantzsch Condensation) |
chemical methods of measuring triglyceride? |
|
|
|
Glycerol Kinase method
-Hydrolysis of TAG to free fatty acids and glycerol -Phosphorylation of glycerol to glycerolphosphate
-Disappearance of NADH is measured at 340 nm |
enzymatic method of measuring triglyceride? |
|
|

|
Reference value of microalbuminuria? |
|
|
|
10 to 30 mg/dL (2/3 of the CSF total protein) |
CSF Albumin is how much of the CSF total protein? |
|
|
|
Coomassie Brilliant Blue dye |
What dye is used to measure CSF protein? |
|
|
|
Oligoclonal Banding: Presence of 2 or more IgG bands in the y region Condition: Multiple Sclerosis Indication: Inflammation w/in the CNS |
What is CSF oligoclonal banding? what condition is it seen? It indicates what? |
|
|
|
Supporting medium: Agarose Gel Stain: Coomassie Brilliant Blue |
Supporting medium of electrophoresis abd stain for oligoclonal binding |
|
|
|
Elevated levels of homocysteine & methionine in blood and urine Cystathionine B-Synthetase is impaired |
What is homocystinuria? |
|
|
|
Modified Guthrie Test |
Screening test for homocysteinuria? |
|
|
|
Deficient: A-ketoacid Decarboxylase Screening test: Modified Guthrie Test Accumulation of: Branched Amino Acid (Leucine, Isoleucine, Valine) Diagnostic test: Amino Acid Analysis (HPLC)
|
What is maple syrup urine disease?
Deficient?
Screening test?
Accumulation of?
Diagnostic test?
|
|
|
|
Deficient: Phenylalanine Hydrolase (Phenylalanine hydrolase converts phenylalanine to tyrosine)
Clinical features: Severe mental retardation Screening test: Guthrie Bacterial Inhibition Assay (B.subtilis spores) + Result: Bacterial growth if phenylalanine is >4mg/dL |
Phenylketonuria
Deficient: Clinical Feautures: Screening test: |
|
|
|
potassium phosphate lactate |
factors affected by vigorous hand exercise during veni? |
|
|
|
Glucose cholesterol electrolytes TAG |
analytes that needed basal state collection? |
|
|
|
Glucose, BUN, Creatinine Na, K, Cl CO2 Calcium |
Basic metabolic panel |
|
|
|
Collecting duct |
The final site of either concentrating or diluting urine? |
|
|
|
Nephron |
Functional unit of kidney? |
|
|
|
Ascending loop of Henle |
Part of Kidney that is impermeable to water? |
|
|
|
Ascending loop of Henle |
Part of Kidney that is impermeable to water? |
|
|
|
Basic Metabolic Panel + Phosphorus & albumin |
Renal Function panel? |
|
|
|
Hgb = Increased by 1g/dL
Hct= Increased by 3.5% |
1 Unit of Whole Blood or PRBC increases Hgb by? Hct by? |
|
|
|
Random Donor -From different donors pooled -Takes 4-6 units before it has therapeutic effects -Adv: Cheap -Disadv: From different donors has antigens -QC: 5.5×10^14 Single Donor Platelet -1 unit for therapeutic effect -Less Antigenic -Expensive (12-25k) -QC: 3.0×10^11 |
Differentiate Single from random donor platelet conc |
|
|
|
Whole --> Soft --->PRBC (For RBC Blood Spin loss) \ --> PRP-->Hard Spin / \ / \ <---FFP<--Freeze <--PPP Platelet | @ -18¤C conc. | --->Thaw @1-6-->Centrifuge degrees / \ / \ Cryo Cryo preci super pitate nate
*Cryoprecipitate- For Factor I,XIII, VIII |
How to prepare blood components? |
|

