![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
101 Cards in this Set
- Front
- Back
|
What are the major components of the chest anatomy?
|
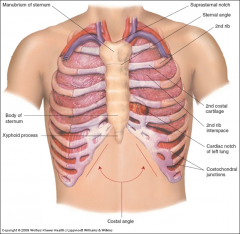
- Manubrium
- Suprasternal notch - Sternal angle (angle of Louis) - 1st and 2nd ribs - Xyphoid process |
|
|
Pectus excavatum
|
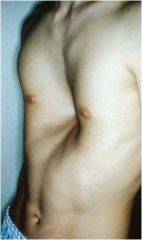
Depression in the lower sternum
|
|
|
Pectus carinatum
|

Anteriorly displaced sternum
|
|
|
Traumatic flail chest
|
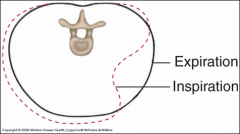
Multiple rib fractures resulting in paradoxical movements of the thorax.
On inspiration, injured area caves inward and expiration outward |
|
|
Thoracic kyphoscoliosis
|

Abnormal spine curve and vertebral rotation causing chest deformities.
|
|
|
How to palpate 2nd rib
|
From suprasternal notch, move about 5 cm inferiorly to the sternal angle and then laterally (start counting interspaces).
|
|
|
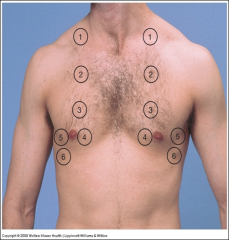
Where is a tension pneumothorax needle inserted?
|
2nd intercostal space
|
|
|
Where is a chest tube inserted?
|
4th intercostal space
|
|
|
Where do ribs articulate?
|
7th rib - last to articulate with sternum
8-10th ribs - articulate with costal cartilage 11th and 12th ribs - free floating |
|
|
How do you palpate the 12th rib?
|
Palpable posteriorly and can start counting ribs/interspaces
|
|
|
Where is a thoracentesis performed?
|
T7-T8 interspace
Palpate the inferior tip of scapula, which lies at the level of the 7th rib/interspace. |
|
|
How do you palpate C7?
|
With neck flexed, the most protruding process is usually C7.
|
|
|
How to describe locations on the chest
|
Vertical axis – note rib level by counting ribs
Circumference around the chest – bony landmarks and vertical lines |
|
|
Vertical lines on chest
|
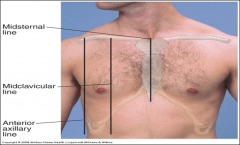
- Midsternal line
- Midclavicular line (near nipple line) - Axillary lines (anterior, midaxillary, posterior axillary) - Vertebral line - Scapular line |
|
|
Where is the apex of lung located?
|
Rises 2-4 cm above clavicles
|
|
|
Where is the base of the lung located?
|
Extends
- 6th rib midclavicular - 8th rib midaxillary - T10 spinous process posteriorly |
|
|
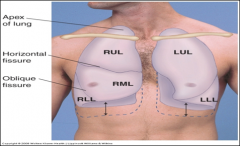
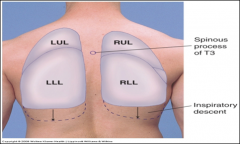
Where is oblique fissure of lung located?
|
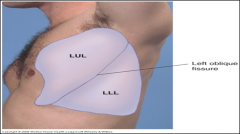
Near the spinous process of T3.
|
|
|
Where is horizontal fissure of lung located?
|
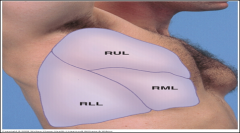
Near 4th rib to midaxillary line near 5th rib.
On right chest, must listen to the lateral chest for right lower lobe (RLL) sounds. |
|
|
Where is the tracheal bifurcation located?
|
At sternal angle anteriorly and T4 posteriorly.
|
|
|
Common chest complaints
|
- Chest pain
- Shortness of breath - Wheezing - Cough - Hemoptysis (coughing up blood) |
|
|
Possible causes of chest pain
|
- Cardiovascular
- Pulmonary - GI - Musculoskeletal - Skin - Anxiety ... and others |
|
|
Location of cardiovascular chest pain
|
- Substernal
- Shoulder - Jaw - Neck |
|
|
Quality of cardiovascular chest pain
|
- Pressure
- Ache - Heavy - Crushing - Ripping or tearing - Sharp |
|
|
Quantity of cardiovascular chest pain
|
Mild to severe (typically more significant)
|
|
|
Timing of cardiovascular chest pain
|
- 1-20 min and intermittent (angina)
- Constant (pericarditis and dissection) |
|
|
Aggravating factors related to cardiovascular chest pain
|
- Exertion (angina/MI)
- Breathing and position (pericarditis) |
|
|
Alleviating factors related to ardiovascular chest pain
|
Rest, sitting forward (pericarditis)
|
|
|
Associated symptoms of cardiovascular chest pain
|
Dyspnea, nausea, diaphoresis (angina/MI)
|
|
|
Levine sign
|
A clenched fist over the anterior chest, typical in coronary syndrome.
|
|
|
Tracheobronchitis presentation
|
May be related to flu, upper chest, burning, mild-moderate, aggravated by cough/deep breathing, alleviated by lying on involved side
|
|
|
Pleuritic pain presentation
|
Any chest wall area, sharp/stabbing, mod-severe, constant, aggravated by cough/breathing/chest wall motion
|
|
|
Bronchospasm presentation
|
Substernal, sharp to ache, mild-severe, episodic, aggravated by cough/breathing deep, associated with wheezing/dyspnea
|
|
|
GERD presentation
|
Substernal and to back, burning/squeezing, mild-severe, worse after meals and lying down, alleviated with antacids (some)
|
|
|
Esophageal spasm presentation
|
Substernal to jaw or back, squeezing, mild-severe, aggravated with swallowing, improved occasionally with belching and antacids
|
|
|
Peptic ulcer presentation
|
Substernal to back/abdomen, ache to burn, mild-severe, initially may improve with food then worsen later
|
|
|
Gallbladder disease presentation
|
Substernal to back/abdomen, ache to burn, mild-severe, initially may improve with food then worsen later, worse with greasy meals.
|
|
|
Musculoskeletal chest pain
|
Any location on chest wall, stabbing to aching, mild-severe, lasts hours to days constant to variable, aggravated by chest motion, tender over area
|
|
|
Anxiety pain
|
Any chest wall location, ache-dull-sharp-pressure, mild-severe, variable timing usually hours-days, may follow emotion stress event (but not always)
|
|
|
Possible causes of shortness of breath (dyspnea)
|
Congestive heart failure
COPD/Chronic bronchitis Asthma Interstitial lung disease Pneumonia Pneumothorax Pulmonary embolism (blood clot) Anxiety Other: GERD (causes lung spasms), obesity, etc… |
|
|
Wheezing
|
Musical respiratory sound heard with inspiration and expiration “accordion sound.”
Cause: airway obstructive from secretions, inflammation, or foreign body |
|
|
Cough
|
Dry or productive
Cause: irritant as in mucus, pus, blood, dust, foreign bodies, heat/cold, medication (Mucinex, ACE inhibitors), other |
|
|
Hemoptysis
|
Coughing up blood from lungs (blood > mucus)
Typically bright red or rust colored Consider neoplasm until proven otherwise Always quantify amount and frequency and last episode Causes: infection, lung cancer, CHF, PE, irritant, could be postnasal, mouth, pharynx, or GI source |
|
|
Stridor
|
Audible high pitched wheezed, ominous sign of airway obstruction in the larynx or trachea.
Cause: epiglottitis, laryngeal spasm, foreign body |
|
|
Orthopnea
|
Dyspnea that occurs when patient is lying down and improves with sitting up.
Common in CHF |
|
|
Paroxysmal nocturnal dyspnea
|
Sudden dyspnea and orthopnea that awakens the patients from sleep.
|
|
|
Tachypnea/Bradypnea
|
Fast/slow respiratory rate
|
|
|
Kussmal breathing
|
Deep, labored breathing pattern
|
|
|
Cheyne Stokes respirations
|
Deep breathing alternating with periods of apnea
|
|
|
Chest inspection
|
Inspect:
- Rate, rhythm, depth and effort of breathing - Signs of distress - Skin color (cyanosis) - Stridor/wheezing - Chest movements - Chest diameter (larger in COPD) - Retractions (supraclavicular) - Tracheal deviations (indicates pneumothorax) |
|
|
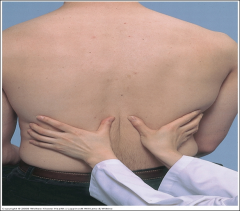
Chest palpation
|
Palpate:
- Painful areas (put finger on area of pain) - Masses - Test chest expansion - Feel for tactile fremitus |
|
|
How to test chest expansion
|
Test anteriorly with thumbs along costal margin
Test posteriorly with thumbs at T10 Watch the distance between the thumbs during inspiration and feel for symmetry Causes of abnormal expansion: - Unilateral decrease or delay in fibrosis - Pleural effusion - Lobar pneumonia - Bronchial obstruction |
|
|
Tactile fremitus
|
Palpable vibrations transmitted through the bronchopulmonary tree to the chest wall.
|
|
|
How to feel for tactile fremitus
|
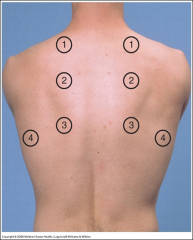
Ask patient to repeat words “99” or “1-1-1," while using bony part of palm or ulnar surface of hand and compare symmetry of left to right.
Decreased when transmission of vibrations from the larynx to chest is impeded. Causes of decreased transmission - Chest wall size (barrel chest) - Obstructed bronchus - COPD - Pleural effusion - Fibrosis - Pneumothorax - Tumor Causes of increased transmission - Unilateral pneumonia |
|
|
Chest percussion
|
- Perform side to side to assesses for asymmetry
- Test extent of diaphragmatic excursion - Locate upper border of liver |
|
|
How to percuss chest
|
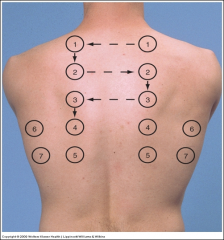
- Perform from side to side to assess for asymmetry
- Strike using the tip of your tapping finger - Use lightest percussion that produces a clear note Percussion establishes whether underlying tissues (5-7 cm deep) are air-filled, fluid-filled, or solid Percussion notes - Flatness (soft) - Dullness (medium) - Resonance (loud) - Hyperresonance (very loud) - Tympany (loud) |
|
|
How to test diaphragmatic excursion
|
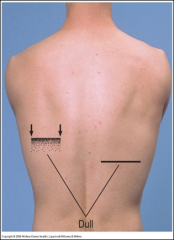
Find level of diaphragmatic dullness during quiet respiration – percuss downward until dullness replaces resonance, confirm laterally and medially.
Estimate the extent of diaphragmatic excursion by determining the distance between the level of dullness on full expiration and the level of dullness on full inspirations (normal 5-6cm). Abnormal high level causes - Pleural effusion, atelectasis or diaphragmatic paralysis |
|
|
Chest Auscultation
|
Most important exam technique for assessing air flow through the tracheobronchial tree.
Together with percussion, it helps to assess the condition of surrounding lungs and pleural space. Listen to the breath sounds with the diaphragm of a stethoscope after instructing the patient to breathe deeply through an open mouth. Use the pattern suggested for percussion, moving from one side to the other and comparing symmetric areas of the lungs. Listen to at least one full breath in each location. |
|
|
How to auscultate the chest
|
Always listen to bare skin (not through clothing or gowns which can generate confusion sounds)
Listen to sounds generated by breathing Listen for adventitious sounds (added) - timing, location, persistence Transmitted Voice Sound Tests - Bronchophony - Egophony - Whispered pectoriloquy |
|
|
Vesicular breath sounds
|
Soft and low pitched
Usually heard over most of both lungs |
|
|
Bronchial breath sounds
|
Louder and higher in pitch
Usually heard over the manubrium Bronchovesicular or bronchial sounds heard in distant locations, suspect air-filled lung replaced by fluid or solid tissue mass. |
|
|
Bronchovesicular
|
Intermediate intensity and pitch
Usually heard over the 1st and 2nd interspaces Bronchovesicular or bronchial sounds heard in distant locations, suspect air-filled lung replaced by fluid or solid tissue mass. |
|
|
Tracheal
|
Very loud, high pitched
Heard over the trachea in the neck |
|
|
Types of adventitious sounds
|
Discontinuous sounds
- Crackles Continuous sounds - Wheeze - Rhonchi - Friction rub - Stridor |
|
|
Asthma
|
Airways characterized by variable and reversible inflammation, mucous plugging, and bronchial smooth muscle constriction.
|
|
|
Clinical presentation of asthma
|
Timing - acute onset with symptom free periods, nocturnal symptoms are most common.
Symptoms - cough, shortness of breath, wheezing, tightness Aggravating factors - allergens, irritants, infections, stress |
|
|
Physical exam findings of asthma
|
Inspection - respiratory retractions if severe, cyanosis, tripod position
Palpation - diminished tactile fremitus Percussion - occasional hyper-resonance Auscultation - wheezing of variable intensity, rhonchi, prolonged expiration |
|
|
Atelectasis
|
A collapse or plugging of the airway resulting in obstruction of airflow and lung tissue collapse into an airless state.
|
|
|
Physical exam findings of atelectasis
|
Inspection - possible tachypnea and diminished chest wall motion (if lobar)
Palpation - diminished or absent fremitus, tracheal shift toward involved side Percussion - dullness over area Auscultation - diminished or absent breath sounds, egophony and whispered pectoriloquy in RUL atelectasis |
|
|
Bronchiectasis
|
A rare chronic obstructive lung disease characterized by localized and irreversible dilation or widening of part of the bronchial tree.
Tissues don't move well, can't get CO2 out effectively. |
|
|
Physical exam findings of bronchiectasis
|
Inspection - tachypnea, respiratory distress, clubbing, cyanosis, wasting
Palpation - no consistent findings Percussion - no unusual findings if no exacerbating cause (pneumonia) Auscultation - crackles usually coarse, rhonchi |
|
|
Chronic Obstructive Lung Disease (COPD)
|
Characterized by over-distention of air spaces distal to terminal bronchioles, with destruction of alveolar septa and airway obstruction (generic term for a broad category of conditions).
Includes emphysema and chronic bronchitis. |
|
|
Clinical presentation of COPD
|
Timing - slow progressive dyspnea and cough
Setting - history of smoking or pollutants, familial deficiency in alpha1 antitrypsin Symptoms - cough, dyspnea, scant mucous production Aggravating factors - exertion, infections |
|
|
Physical exam findings of COPD
|
Inspection - distress, tachypnea, tripod, cyanosis, clubbing, barrel chest
Palpation - decreased fremitus Percussion - diffusely hyperresonant Auscultation - crackles, wheezes and rhonchi associated with bronchitis |
|
|
Chronic bronchitis
|
A chronic obstructive disease characterized by inflammation of the bronchi, mucous production, and cough.
|
|
|
Clinical presentation of chronic bronchitis
|
Timing - slow progressive dyspnea
Setting - history of smoking or pollutant exposure Symptoms - chronic productive cough, wheezing, recurrent infections Aggravating - infections, exertion, irritants, smoking |
|
|
Physical exam findings of chronic bronchitis
|
Inspection - tachypnea, shallow respirations
Palpation - normal fremitus Percussion - resonant Auscultation - vesicular sounds, occasional scattered rhonchi, wheeze, or coarse crackles (early inspiratory) |
|
|
Left-sided congestive heart failure
|
Failure of the heart pump function resulting in increased pressure in the pulmonary veins causing congestion and interstitial edema.
|
|
|
Clinical presentation of CHF
|
Timing - progressive dyspnea or sudden pulmonary edema
Setting - history of heart disease or predisposing factors Associated symptoms - cough, orthopnea, paroxysmal nocturnal dyspnea (PND), occasional wheezing Aggravating factors - exertion, lying flat |
|
|
Physical exam findings of CHF
|
Inspection - tachypnea, tachycardia (CO=HRxSV), distress, edematous state
Palpation - normal fremitus Percussion -resonant Auscultation - late inspiratory crackles (especially bases), possible wheezes, vesicular sounds |
|
|
Pleural effusion
|
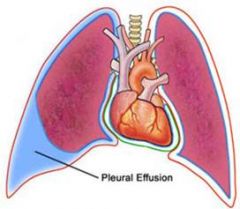
Fluid accumulation in the pleural space which separates air filled lung from the chest wall.
|
|
|
Clinical presentation of pleural effusion
|
Timing - insidious to rapid
Setting - congestive heart failure, malignancy, infectious Associated symptoms - dry cough, dyspnea, pleurisy, orthopnea Aggravating factors - exertion and lying flat |
|
|
Physical exam findings of pleural effusion
|

Inspection - diminished or delayed wall motion on affected side
Palpation - decreased fremitus Percussion - dull to flat over fluid Auscultation - decreased to absent over fluid, pleural friction rub, bronchophony/whispered pectoriloquy |
|
|
Pneumothorax
|
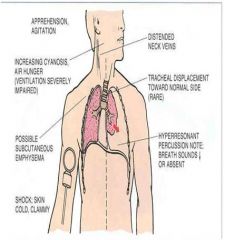
Condition when air leaks into the pleural space, usually unilateral.
Tension – when pneumothorax leads to significant respiratory and circulatory impairment (emergency) Spontaneous – primary or secondary types |
|
|
Clinical presentation of pneumothorax
|
Timing - rapid onset
Setting - trauma, chronic lung disease, surgery, tall, thin male Associated symptoms - dyspnea, respiratory distress, pleurisy Aggravating factors - exertion |
|
|
Physical exam findings of pneumothorax
|

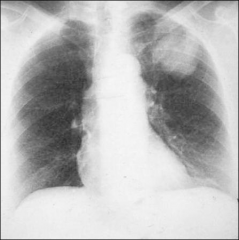
Inspection - tachypnea, cyanosis, distress, tracheal deviation away from pneumothorax
Palpation - decreased to absent fremitus Percussion - hyperresonant Auscultation - decreased to absent, possible friction rub X-ray - dark space is a pneumothorax |
|
|
Hemothorax
|
A condition in which blood accumulates in the pleural cavity, typically associated with trauma or malignancy.
|
|
|
Clinical presentation of hemothorax
|
Timing - rapid to insidious
Setting - trauma to the chest or associated with mass Associated symptoms - shortness of breath, shock, distress, flail chest Aggravating factors - none specific |
|
|
Physical exam findings of hemothorax
|
Inspection - distress/shock, cyanosis, unequal chest rise, tachypnea, tracheal deviation away from affected side
Palpation - decreased or absent fremitus Percussion - dullness over area Auscultation - absent or diminished sounds on affected side |
|
|
Tuberculosis
|
A granulomatous inflammatory disease due to infection with mycobacterium tuberculosis.
|
|
|
Clinical presentation of TB
|
Timing - insidious
Setting - Immune illness (HIV), exposure to locations, poverty Associated symptoms - cough, dyspnea, night sweats, fever, weight loss, blood tinged sputum |
|
|
Physical exam findings of TB
|
Inspection - weight loss, clubbing
Palpation - decreased fremitus Percussion - dullness Auscultation - post-tussive rales |
|
|
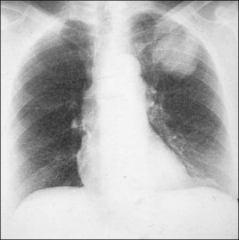
Pneumonia
|
Infection and inflammation of the parenchyma from the bronchioles to the alveoli.
|
|
|
Clinical presentation of pneumonia
|
Timing - acute illness, onset varies with cause
Setting - varied Associated symptoms - cough, sputum production, fever, pleuritic pain Aggravating factors - none specific |
|
|
Physical exam finding of pneumonia
|
Inspection - febrile, distress, labored respiration
Palpation - increased fremitus, bronchophony, egophony, and whispered pectoriloquy Percussion - dull over consolidated area Auscultation - bronchial sounds over consolidated area, late inspiratory crackles |
|
|
Diffuse interstitial lung disease (ILD)
|
Abnormal widespread infiltration of cells, fluid, and collagen into interstitial spaces between alveoli
Includes sarcoidosis, asbestosis, cystic fibrosis and pulmonary fibrosis. |
|
|
Clinical presentation of ILD
|
Timing - progressive dyspnea varies with cause
Setting - varied on cause (occupational exposure, familial) Associated symptoms - weakness, fatigue, minimal cough, hemoptysis Aggravating factors - exertion |
|
|
Physical exam findings of ILD
|
Inspection - non specific unless extra pulmonary signs present, clubbing, cyanosis, barrel chest
Palpation - non specific to decreased fremitus Percussion - resonant Auscultation - non specific crackles and rhonchi |
|
|
What is the leading cause of preventable death in the US?
|
Tobacco abuse
|
|
|
What steps in an H&P should you take regarding tobacco abuse?
|
Remember the 5 “A”s
Ask about smoking at each visit Advise patients regularly to stop smoking using a clear, personalized message – be sure to document Assess patient readiness to quit Assist patients to set stop dates and provide educational materials for self-help Arrange for follow-up visits to monitor and support patient progress No screening for lung cancer is recommended. |
|
|
Lung cancer
|
Generally referring to bronchogenic carcinoma, cancer of the bronchial epithelial structures.
Causes - tobacco, asbestos, radiation, and noxious inhaled agents |
|
|
Symptoms of lung cancer
|
Cough
- Wheezing - Shortness of breath (SOB) - Hemoptysis - Dizziness on exertion (DOE) - Pleurisy - Weight loss Hemoptysis in the setting of weight loss and cough is lung cancer until proven otherwise. |

