![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
79 Cards in this Set
- Front
- Back
|
Name the male accessory glands and what they contribute to semen
What's the purpose? |
Seminal vesicles - fructose
Prostate gland - alkalein substance Bulbourethral glands -mucous protect sperm in the female |
|
|
What is the main fxn/goal of the reproductive system?
|
To make gametes
male makes sperm - haploid (23 chromosomes) female makes eggs - haploid (23 chromosomes) which will fuse together to create a diploid cell (zygote) |
|
|
What is critical for ejaculation to occur
|
erection
|
|
|
what are the two types of secretion of the testes and the products?
|
endocrine = testosterone
exocrine = sperm |
|
|
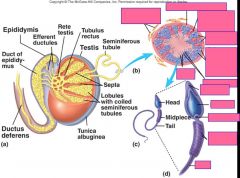
What occurs in the epididymis
|
sperm fully matures
|
|
|
where is sperm created?
|
the seminiforous tubules of the testes
|
|
|
where is testosterone created?
|
the interstitial or leydig cells of the testes
|
|
|
define and describe cryptorchidism
|
Failure of of one or both of testes to descend into scrotum
Prevents normal sperm development |
|
|
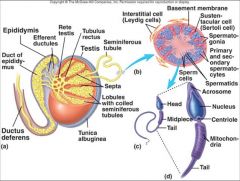
why is the basement membrane of the seminiferous tubule important?
|
b/c it keeps body fluid from entering the tubule so sperm are protected from antibodies in plasma
|
|
|
|
|
|
what are sperm called in their first stage of development?
|
spermatogonia (singular = spermatozoa)
|
|
|
what are sperm called in their second stage of development and how are they formed?
|
primary spermatocytes are formed by mitotic division of the spermatogonia
|
|
|
what are sperm called in their third stage of development and how are they formed?
|
secondary sermatocytes are formed by the first division of meiosis of the primary spermatocytes
|
|
|
what are sperm called in their fourth stage of development and how are they formed?
|
spermatids are formed by the second division of meiosis of the secondary spermatocytes
|
|
|
describe the development of the spermatid
|
Spermatids develop an acrosome and flagellum while being nourised by the sertoli cells in the seminiferous tubule
|
|
|
what and where are sertoli cells
|
cells that nourish the sperm cells and form a blood-testis barrier and produce hormones
in the seminiferous tubules |
|
|
What are the three steps in spermatogenesis?
|
1. Mitotic division - of the spermatogonia to produce two primary spermatocytes which are diploid daughter cells
2. 1st meiotic division of primary spermatocytes to form two haploid daughter cells called 2ndary spermatocytes 3. 2nd meiotic division - of the secondary spermatocytes to form two haploid spermatids |
|
|
++
|
++
|
|
|
define mitosis
|
on diploid cell (2n) divides to form two identical diploid daughter cells
|
|
|
define meiosis
|
one diploid (2n) mother cells divides into two haploid cells (1n + 1n)
|
|
|
why is the 3rd step of spermatogenesis not really meiosis?
|
because the secondary haploid daughter cells divide to form two identical haploid daughter cells. (really is mitosis)
|
|
|
describe the path of sperm once it laves the testes?
|
1. epididymis
2. Vas deferens - passes into abdominal cavity through this 3. urethra |
|
|
describe the penis
|
Three columns of erectile tissue that engorge with blood
Corpora cavernosa (2) Corpus spongiosum (1) |
|
|
what percentage of semen to the various accessory glands contribute
|
Seminal vesicles Produce about 60% of semen
Prostate gland Produces about 30% of semen Bulbourethral glands Contribute about 5% to semen |
|
|
what is the purpose of the various accessory glands secretions?
|
seminal vesicle contributes fructose for sperm energy source
prostate gland produces alkaline sub to buffer sperm against female repro tract bulbourethral gland contrubutes mucous to keep sperm grouped together to increase viability |
|
|
++
|
++
|
|
|
what is emission
|
Discharge of semen into prostatic urethra
|
|
|
testosterone is regulated through _________ feedback
describe |
negative
increase testosterone in the blood will decrease the stim hormones: GnRH in the hypothalamus and LH in the anterior pituitary |
|
|
what are the three roles of testosterone?
|
1. Negative feedback loop to regulate it's own production
2. Causes and maintains secondary sex characteristics 3. works with Sertoli cells to cause and maintain spermatogenesis |
|
|
describe male sex hormone secretion regulation
|
Hypothalamus releases
GnRH which stimulates: LH and FSH to be released from anterior pituitary: LH stimulates the interstitial cells of the testes to release testosterone FSH stimulates the growth of sertoli cells to nourish increased sperm cells |
|
|
what are the three structures involved in testosterone regulation?
|
1. hypothalamus - regulates the anterior pituitary
2. Anterior pituitary - regulates the testes 3. testes - regulates anterior pit and hypothalamus through testosterone production |
|
|
what is the difference between before puberty and after puberty?
|
before puberty there's no GnRH (small amounts of testosterone inhibit GnRH)
During puberty testosterone does not completely suppress GnRH release, resulting in increased FSH,LH, and testosterone which causes secondary sex characteristics of puberty |
|
|
++
|
++
|
|
|
Give 5 ways male and female are different in reproduction
|
1. in fem you see both + and - feedback, in males only see negative
2. in males, sex hormone production occurs constantly , in fem, it occurs cyclically 3. fem will eventually stop producing sex H, but male will produce throughout life 4. Both have erectile tissue, men have more, longer 5. fems have separate urinary and reproductive tracts, males merge |
|
|
++
|
++
|
|
|
Describe the steps for how and erection occurs
|
In the neuron, nitric oxide synthase produces nitric oxide which easily travels into the smooth muscle cells of blood vessels
In the muscle cell, NO activates guanylate cyclase, which causes the production of cGMP, the second messenger, which indirectly causes the relaxation of smooth muscle, causing vasodilation |
|
|
what is the most basal layer of the uterus? Its purpose?
|
the perimetrium - secretes lubricant to prevent friction with other organs and structures
|
|
|
what hormone is responsible for follicle maturation in females?
|
FSH
|
|
|
List the stages of follicle maturation in females
|
1.primordial follicle
2. primary follicle 3. secondary follicle 4. mature (Graafian) follicle |
|
|
describe the primordial follicle
|
contains the oocyte (gamete) surrounded by one layer of granulosa cells which produce estrogen, but only a little b/c there are so few.
|
|
|
describe the primary follicle
|
the zona pellucida develops, which is a protective barrier around the gamete, as well as an increase number of granulosa cells develop
|
|
|
describe the secondary follicle
|
fluid filled vescicles develope in the midsts of the granulosa cells, which have increased in number again
|
|
|
describe the mature (Graafian) follicle
|
all of the fluid-filled vescicles fuse together forming a large "antrum" with the oocyte pushed off to the side. The antrum is THE characteristic of the mature follicle.
|
|
|
Describe ovulation
|
the follicle ejects the oocyte along with the corona radiata - which are granulosa cells which remain around the oocyte
|
|
|
Describe what happens to the follicle after ovulation
|
the granulosa cells become corpus luteum cells and grows larger in response to LH
Corpus luteum releases P4 |
|
|
describe what the corpus albicans is
|
its the remaining dead corpus luteum cells - no more P4 released
|
|
|
what is oogenesis?
|
Oogenesis is the production of a secondary oocyte in ovaries
|
|
|
what are oogonia?
|
Oogonia are cells from which oocytes develop
|
|
|
describe primary oocytes
|
Primary oocytes are surround by granulosa cells and called a primordial follicle
|
|
|
when does a primordial follicle become a primary follicle?
|
Primordial follicle becomes a primary follicle when oocyte enlarges and cells change
|
|
|
how does a primary oocyte become a secondary oocyte?
|
Primary oocyte completes first meiotic division to produce secondary oocyte and a polar body
|
|
|
describe the vagina
describe the clitoris |
much more elastic than the uterus
erectile structure with corpora cavernosa |
|
|
The secondary oocyte fully matures and undergoes _______ division after ________________
|
meiotic division
sperm unites with the secondary oocyte |
|
|
describe the acrosome
|
it is what's responsible for species specific fertilization - key in lock only species of like kind can fertilize the egg
penetrates the egg by joining with the zona pellucida |
|
|
what are the three layers of the uterus?
|
Perimetrium: Serous membrane
Myometrium: Smooth muscle Endometrium: Mucous membrane |
|
|
how is milk expressed from mammae?
|
lobes release milk into lactiferous sinusus, then into lactiferous ducts in the nipple
|
|
|
what are the phases of the menstrual cycle?
|
Menses
Proliferative phase Secretory phase Menses |
|
|
define amenorrhea
menarch |
abnormal absence of menstrual cycle
1st period |
|
|
describe menopause
|
Cessation of menstrual cycles
Normal - occurs in healthy women E2 and P4 are no longer produced by the ovaries |
|
|
Describe the follicular phase
|
occurs in the ovaries from day 0 to day 14
hypothalamus releases GnRH which increases FSH release from ant. pit. FSH stimulates the growth of the follicle, and E2 release from the follicles in ovaries increases as the follicles grow |
|
|
Describe the proliferative phase
|
Occurs in the endometrium of the uterus, from Day 0 to Day 14
As more E2 is released from follicle the endometrium thickens (proliferates) |
|
|
describe the luteal phase
|
occurs in the ovaries from day 14 thru 28
In response to LH secretion from ant. pit., the corpus luteum grows and produces P4 |
|
|
describe the secretory phase
|
occurs in the uterus, in response to increased P4, the endometrium continues to thicken and develop secretory glands
|
|
|
in the female, when does negative feedback occur in sex hormone regulation?
describe |
During the follicular phase
If e2 gets too high, then GnRH decreases. If P4 gets too high, then GnRH and LH decrease |
|
|
When does positive feedback occur in sex hormone regulation?
describe |
During Ovulation
E2 gradually increases during the follicular phase due to increased LH secretion and the increased E2 secretion positively influences more LH to be secreted, thus more E2 is secreted, until it reaches a threshold level where it triggers ovulation |
|
|
++
|
++
|
|
|
Describe the negative feedback in the luteal phase
|
GnRH increases LH which stimulates corpus luteum growth, which then produces more and more P4. If P4 gets too high, it shuts down LH and GnRH, which causes the corpus luteum to die
|
|
|
++
|
++
|
|
|
what causes menses?
|
The increased levels of P4 negatively affect production of GnRH and LH, which in turn cause the corpus luteum to die and stop producing P4. Without P4, the endometrial lining can't be sustained and it is sluffed off during menses.
|
|
|
++
|
++
|
|
|
Why is it important that E2 increases gradually in the proliferative phase?
|
critical b/c it allows the timing of the cycle to continue. If it increased very fast, you'd never get to the positive feedback point of ovulation
|
|
|
why is there no menses during pregnancy?
|
the placenta releases HCG which replaces LH's function in maintaining the corpus luteum, so P4 continues to be released and the lining remains in tact
|
|
|
describe two differences btw male and female gametes
|
Oocyte can be fertilized up to 24 hours after ovulation
Sperm cells can be viable for up to 6 days in female tract sperm is fully mature upon release vs. egg which is not fully matured until after fertilization |
|
|
where does fertilization typically occur?
|
in the ampulla of the uterine tube
|
|
|
describe hormonal changes in the first trimester,
|
HCG secreted from the placenta takes the place of LH, which maintains the corpus luteum, allowing ovary to continue to secrete E2 and P4, which maintains endometrium and extends secretory phase
|
|
|
++
|
++
|
|
|
describe hormonal changes in the third trimester,
|
very little HCG is produced by the placenta, no hormones are being produced by the ovary now, and the placenta takes over producing E2 and P4
|
|
|
name some hormonal similarities and differences between male and female
|
Similar: both have GnRH, FSH, and LH
Different: females have E2 and P4, males have testosterone |
|
|
Describe P4 levels in relationship to E2 levels throughout pregnancy
|
P4 is higher than E2 all throughout pregnancy except right before delivery when an increase in E2 over P4 triggers labor
|

