![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
109 Cards in this Set
- Front
- Back
|
What is skeletal cartilage made of? |
Cartilage tissue |
|
|
Perichondrium (definition?) |
layer of dense irregular connective tissue surrounding cartilage |
|
|
What is the function of the perichondrium? |
Contains blood vessels that nutrients diffuse from to reach cartilage.
- acts like a girdle preventing cartilage from squeezing out |
|
|
What are the 3 types of cartilage? |
- Hyaline -Elastic -Fibrocartilage |
|
|
What is the function of Hyaline Cartilage? |
Provide support with flexibility & resilience |
|
|
What type of cartilage are articular cartilages, costal cartilages, respitory cartilage, & nasal cartilage? |
Hyaline Cartilage |
|
|
How is elastic cartilage different from Hyaline cartilage? |
Elastic has elastic fibers is springy like a rubber band |
|
|
What does elastic cartilage provide? |
strech and can withstand repeated bending |
|
|
Where is elastic cartilage found? |
External ear & epiglotis |
|
|
How is fibrocartilage different from Hyaline & Elastic cartilage? |
Fibrocartilage has a somewhat parrallel rows of chondrocytes alternating wiht thick collegan fibers |
|
|
What are advantages to Fibrocartilage? |
it is highly compressible with great tensile strength |
|
|
Where is fibrocartilage found? |
Sites that are under both pressure and stretch
-Pubic symphysis & menisci & intervertebral discs |
|
|
What tissue is used to lay down the Embryonic skeleton & provide new skeletal growth? |
Cartilage |
|
|
Appositional Growth (definition?) |
Growth accomplished by the addition of new layers onto those previously formed |
|
|
Interstitial growth (definiton?) |
Lacunae bound chondrocytes divide and secrete new matrix expanding cartliage from within |
|
|
What are the 2 groups of the human skeleton? |
-axial -appendicular |
|
|
Axial Skeleton (definition?) |
-forms the long axis of the body -includes bones of the skull, verterbral column, & rib cage |
|
|
Appendicular Skeleton (definiton?) |
consistws of the bones of the upper & lower limbs and the girdles ( shoulder & hip) that atttach to the axial skeleton |
|
|
How are bones classified? |
- by shape - long - short -irregular - flat
|
|
|
Long bone (definiton?) |
-longer than wide -has 1 shaft - has 2 ends that are expanded |
|
|
Which of the limb bones are not long bones? |
- Patella -wrist -ankle bones |
|
|
Short bones (definition?) |
-roughly cube shaped
ex. writst & ankle bones |
|
|
Sesamoid bones (definition?) |
-shaped like a sesame seed -special type of short bone that froms in a tendon
ex. patella |
|
|
Flat bones (definition?) |
-thin, flattened, and slightly curved
ex. sternum, scapula, ribs, and most skull bones |
|
|
Irregular bones (definition?) |
- have complicated shapes - do not fit into long, short, or flat bone catagories
ex. vertebrae & hip bone |
|
|
What are the 7 functions of bones? |
- support (leg bones support body trunk) -protection (skull protects brain) -movement (muscles use bones as leverage) -mineral & growth factor storage -blood cell formation -Triglceride storage -hormone production |
|
|
Which type of bone is external? |
Compact bone |
|
|
Compact bone (definition?) |
smooth and solid bone found on outer layer of bones |
|
|
Spongy bone (definition?) |
-honeycombe of small needle like projections -is trabeculated - found on internal layers of bone |
|
|
Trabeculae (definition?) |
- nooks and crannies texture found in spongy bone |
|
|
What fills the trabeculated spaces in living bone? |
red or yellow bone marrow |
|
|
What is the structure of short, irregular & flat bones? |
-thin plates of spongy bone covered by compact bone -covered inside & outside with connective tissue -no well defined medullary cavity -marrow is contained among trabeculae |
|
|
Periosteum (definition?) |
-white double layered membrane that covers external surface of the entire bone except joint surfaces |
|
|
Endosteum (definition?) |
- connective tisue membrane that covers internal bone surfaces -lines trabeculae & canals in bone |
|
|
What are the membranes that cover the outside & inside of the bone called? |
- Periosteum (outside) - Endosteum (inside) |
|
|
Diploe (definition?) |
- spongy bone found in flat bones
|
|
|
What is the structure of long bones? |
- 1 shaft (diaphysis) -2 bone ends (epiphysis) -Membrane -1 marrow cavity (medullary cavity) |
|

What color represents the axial skeleton? |
Orange |
|

What color represents the Hyaline Cartilage? |
Blue |
|

What color represents the appendicular skeleton? |
Beige |
|

What color represents the elastic cartilage? |
green |
|

What color represents the fibrocartilage? |
red |
|

What class of bone is this? |
long bone |
|

What class of bone is this? |
Irregular bone |
|

What class of bone is this? |
Flat bone |
|
What class of bone is this? |
Short bone |
|
|
Diaphysis (definition?) |
Saft of long bone |
|
|
What is the structure of a diaphysis? |
thick collar of compact bone that surroundes the medullary cavity |
|
|
Medullary cavity (definition?) |
marrow cavity found in long bones |
|
|
Yellow marrow (definition?) |
found in adult & contains fat |
|

Label the parts of the long bone. |

|
|
|
Epiphysis (definition?) |
bone ends of long bones |
|
|
What is the structure of epiphysis? |
- outer shell of compact bone -inner spongy bone |
|
|
Epiphyseal line (definition?) |
remnant of epiphyseal plate |
|
|
Epiphyseal Plate (definition?) |
plate of hyaline cartilage at the junction of the diaphysis that provides for growth in length of the bone |
|
|
Nutrient foramina (definition?) |
pathway that blood vessels & nerve fibers use to reach medullary cavity from the periosteum |
|
|
Where is red marrow found? |
- Trabeculae - Diploe of flat bones - Red marrow cavities |
|
|
Bone markings: what are projections? |
bulge outward from the surface of the bone
-include: -heads -trochanters -spines |
|
|
Bone markings: what are depressions? |
dips in the surface of the bone
include: -fossae - sinuses - foramina - grooves |
|
|
Bone markings: What is the purpose of projections? |
used as a place where muscles attach and use the projection for leverage |
|
|
Bone Markings: What is the purpose of depressions? |
they allow nervess & blood vessels to pass |
|
|
What are the 5 types of cells that occupy bone tissue? |
- osteogenic cells - osteoblasts - osteocytes - bone lining cells - osteoclasts |
|
|
Of the 5 types of cells found in bone tissue, which ones are not formed from mesenchymal cells? |
osteoclasts |
|
|
Osteogenic or osteoprogeniter cells (definition?) |
- miotically active cells found in periosteum & endosteum
- differentiate into osteoblast cells or bone lining cells. |
|
|
Osteoblast cells (definintion?) |
- bone forming cells that secrete the bone matrix.
- actively miotic - play role in matrix calcification - when ostoblasts are completly surrounded by matrix they become osteocytes |
|
|
osteocytes (definition?) |
- mature bone cells that occupy lacunae that conform to their shape |
|
|
What is the function of osteocytes? |
- monitor & maintain the bone matrix - act as stress or strain "sensors," - respond to mechanical stimuli ( bone loading, bone deformation, weightlessness) |
|
|
Bone Lining Cells (definition?) |
flat cells found on bone surfaces where bone remodeling is not going on. |
|
|
What is the purpose of bone lining cells? |
- Help maintain matrix
- periosteal = bonelining cells on external bone surfaces
- endosteal = bone lining cells on internal bone surfaces |
|
|
Osteoclast (definition?) |
- giant multinuleate cells located at sites of bone resorption
- are macrophages
- break down bone |
|
|
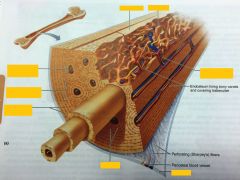
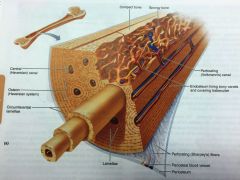
Osteon (definition?) |
-structrual unit of compact bone - elongated cylinder oriented parallel to the long axis of the bone. |
|
|
Lamella (definition?) |
bone layer such as of bone matrix in an osten of compact bone |
|
|
Haversian canal or Central Canal (definition?) |
Canal that runs through the core of each osteon & contains blood vessels and nerve fibers that serve the osteon cells. |
|
|
Volkmann's Canals (definition?) |
lie at right angles to the long axis of the bone & connect the blood & nerve supply of the medullary cavity to the central canals |
|

Label the figure. |

|
|
|
Canaliculi (definition?) |
canals that connect the lacunae to each other and to the Haversian (central) canal |
|
|
What is the funciton of the canaliculi? |
allows transportation of nurishment |
|
|
Interstitial Lamellae (defintion?) |
-incomplete lamellae that fill gaps between forming osteons
- remnants of osteons that have been cut though by bone remodeling |
|
|
Circumferencial Lamellae (definitoin?) |
- located just deep to the periosteum & just superficial to the endosteum - extends around the entire circumference of the diaphysis |
|
|
What is the function of circumferencial lamellae? |
resists twisting of the long bone |
|
|
How do trabeculae strengthen spongy bone? |
trabeculae align precisely along lines of stress & help the bone resist stress |
|
Label. |
|
|
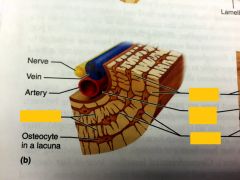
label |

|
|
|
What is an osteoid? |
organic part of the cell matrix |
|
|
What are the major mineral salts found in bone tissue? |
- calcium - phosphate |
|
|
Before week 8 what is the skeleton of a human embryo constructed of? |
hyaline cartilage |
|
|
When does bone tissue begin to form in a human embryo? |
- 8 Weeks |
|
|
Endochondral Ossification (definition?) |
- bone develops by replacing hyaline cartilage - = cartilage bone or endochondral bone |
|
|
Intamembranous Ossification (definition?) |
a bone developes from a fibrous membrane
- = membrane bone |
|
|
Which bone in the human body form using endochondral ossification? |
all bone below the skull except clavicals |
|
|
Which bone in the human body form using Intramembranous ossification? |
the skull & clavicals |
|
|
What are the steps for bone formation using endochondral ossification? |
setting stage: 1) starts with a hyaline cartllage model 2) blood vessels infiltrate the perichondrium converting it to vascularized periosteum 3) vasculariztion results in mesenchymal cells differentiating into osteoblasts
Formation: 4) periosteal bone cartilage forms 5) cartilage @ primary ossification site calcifies 6) periosteal bud invades the internal cavities forming spongy bony 7) Diaphysis elongates & medullary cavity forms 8) Epiphysis ossifies 9) Secondary ossification site appear in epiphysises shortly before or after birth. |
|
|
Periosteal bud (definition?) |
a collection of elements that contain a nutrient artery & vein, nerve fibers, red marrow elements, ostogenic cells, & osteoclasts |
|
|
What are the 4 steps in intramembranous Ossification? |
1) ossification center appears in fibrous connective tissue.. - mesechymal cells cluster and differentiate into osteoblasts
2) Osteoid is secreted within the fibrous membrane and calcifies - osteoblasts become osteocytes 3) Trabeculated bone & periosteum form 4) Lamellar bone replaces thickened Trabeculae forming compact bone, red marrow appears |
|
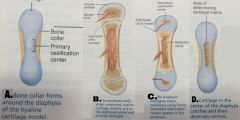
Put steps of endochondral ossification in order. |
|
|
|
What is hypercalcemia? |
- high blood levels of Calcium - leads to excell deposits of calcium salts in blood vessels, kidneys, & other soft organs hampering thier funciton |
|
|
What is Wolff's law? |
- healthy bone will adapt its internal structure in response to mechanical stresses |
|
|
What are the 3 ways to classify a fracure? |
- position of the bone ends after fracture - displaced fracture = bone ends are out of normal alignment.
- Completness of break - complete fracture = bone is broken through - incomplete fracture = bone has not broken through
- if the bone ends penetrate the skin - compound fracture = do penetrate - simple fracture = do not penetrate |
|

What type of fracture is this? |
comminuted fracture |
|
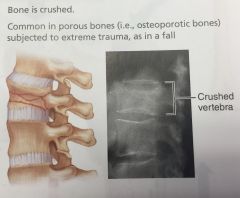
What type of fracture is this? |
Compression fracture |
|
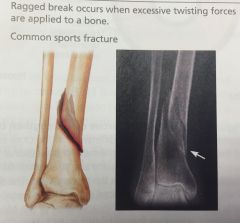
What type of fracture is this? |
Spiral Fracture |
|
What type of fracture is this? |
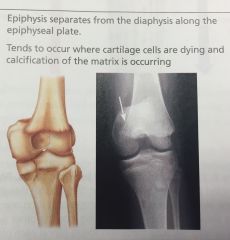
Epiphyseal fracture |
|
What type of fracture is this? |
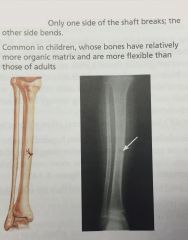
Green stick fracture |
|
What type of fracture is this? |
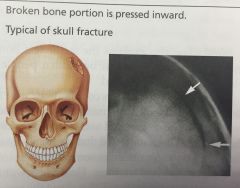
Depression fracture |
|
|
What are the 4 major stages of repair? |
- Hematoma forms (blood vessels clot, bone cells die causing pain, swelling, & inflammation)
- Fibrocartilagenous callus forms - Capilaries grow - phagocytic cells clean debris - fibroblast, cartilage & osteogenic cells begin reconstruction - fibroblasts create collagen that connects bone ends
- Bone remodelling happens - bony callus is remodeled -excess materials are removed - compact bone is laid down |
|
|
Osteomalacia (definition?) |
- disorders where bone are poorly mineralized - bones are soft & weak - symptom is pain when bone is weight bearing - caused by insufficient calcium in diet or vitamin D dificiency |
|
|
Ricket (definition?) |
- Children's version of Osteomalacia - is more sever than osteomalacia because bones are still growing - symptoms; - bowed legs - deformities of the pelvis, skull, & rib cage -epiphyseal plates can't calcify so they continue to widen -caused by insufficient calcium in diet or Vitamin D deficiancy. |
|
|
Osteoporosis (definition?) |
- group of diseases where bone resorption outpaces bone deposits
-bones become so frabile that a sneeze can break them |
|
|
Paget's Disease (definition?) |
- excessive haphazard bone deposit & resorption - new bone (pagetic bone) is hastily made & has abnormal high ratio of spongy bone to compact bone -creates spotty weakening of bone. |

