![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
167 Cards in this Set
- Front
- Back
|
Define Immunity |
The body's ability to resist infectious disease through non specific and specific mechanisms |
|
|
Define Non-specific immunity |
An inborn set of pre existing defences against pathogens |
|
|
Is Non-specific immunity present at birth? |
Yes, it offers instant protection |
|
|
Does non-specific immunity work against a wide variety of pathogens and pathogen products? |
Yes |
|
|
What lines of defense are included in non-specific immunity? |
Both First and Second lines of defense |
|
|
Where in the body are mucous membranes located? Give examples (6) |
Line all body cavities open to the exterior. Ex: respiratory tract, digestive tract, reproductive tract, urinary tract and conjunctiva |
|
|
Explain the role of intact skin as components of non-specific immunity |
Intact skin acts as a barrier and dry skin inhibits growth of most microbes. Sweat on skin contains salt that draws water out of microbes and the normal flora of skin out competes pathogens |
|
|
What does the Seabum of skin do? |
Decreases the pH which most microbes don't tolerate. Also softens skin making it less likely to tear |
|
|
Are Dendritic cells in skin phagocytes? |
Yes |
|
|
Explain the role of mucous membranes as components of Non-specific immunity. |
Cells of the mucous membranes continuously shed and the mucous made from mucous membranes trap pathogens that are easier to carry microbes out of the body |
|
|
Are the Dendritic cells in Mucous membranes phagocytes? |
Yes |
|
|
What is blood made of (2) |
Plasma and formed elements |
|
|
Define plasma |
Liquid portion of blood. |
|
|
What are formed elements composed of? |
Cells and cell fragments |
|
|
Where are blood cells formed? |
In the bone marrow |
|
|
Define a Erythrocytes |
Red blood cells that carry oxygen and carbon dioxide |
|
|
Define platelets |
Cell fragments in charge of clotting |
|
|
Define leukocytes |
White blood cells in charge of immunity |
|
|
List the 6 types of leukocytes |
1. Basophils 2. Eosinophils 3. Neutrophils 4. Monocytes 5. Lymphocytes 6. Dendritic cells |
|
|
Define Basophils |
In charge of information, allergy. |
|
|
Define Eosinophils |
Worm and fungal infections, allergy, inflammation |
|
|
Define Neutrophils |
In charge of phagocytosis |
|
|
Define Monocytes (aka Macrophages) |
In charge of phagocytosis |
|
|
What immunity does Lymphocytes take the most place? What do they include? (3) |
Specific immunity. T, B and natural killer cells |
|
|
Define Dendritic cells |
Concentrated in skin and mucous membrane. Capable of phagocytosis |
|
|
Which leaukocytes comprise the highest percentage of total leukocytes? |
Neutrophils (50%-70% of total leukocytes) & Lymphocytes (25%-45% of total leukocytes) |
|
|
List the members of the second line of defense (6) |
1. Phagocytosis 2. Extracellular killing 3. Complement 4. Interferons 5. Inflammation 6. Fever |
|
|
Define phagocytosis |
Cellular eating: clean up harmful or unwanted substances. |
|
|
Define Phagocytes |
Cell's capable of phagocytosis; phagocytic leukocytes |
|
|
What are the most important phagocytes in the body? |
Macrophages & Neutrophils |
|
|
List the steps, in order, of phagocytosis |
1. Chemotaxis 2. Adherence 3. Ingestion 4. Killing 5. Elimination |
|
|
What increases the "Adhearance" step phagocytosis? |
Antibody or Compliment bound to the object |
|
|
What decreases phagocytosis "Adhearance" step? |
Glycocalyx (capsule or slime layer) |
|
|
Define Extracellular Killing |
Cell secrets toxin (chemical) to kill helminthes, virus infected cells, and tumor cells |
|
|
How do eosinophils participate in extracellular killing? |
They attach to helminthes surface and secrete a chemical (toxin) that weakens/kills the helminth |
|
|
How do natural killer cells participate in extracellular killing? |
Screte toxins that kills virus infected cells and tumor/cancer cells |
|
|
Where are Natural killer cells found? (5) |
Tonsils, lymph nodes, spleen, blood and lymph |
|
|
What is a Compliment? |
30 blood proteins that work together to destroy bacteria |
|
|
Do the Compliment proteins circulate in the blood in an active or inactive form? |
Inactive form |
|
|
List the 2 pathways to activate a Compliment |
1. Classical pathway: antibody bound to antigen 2. Alternative pathway: pathogen or pathogen product |
|
|
List four things that happen when Compliment is activated |
1. Cell lysis (drills holes in pathogen or pathogen product) 2. Call other immune cells to the area 3. Increase phagocytosis 4. Increase inflammation |
|
|
What are interferons? |
Anti-viral proteins produced by some animal cells after viral infection |
|
|
Are Interferons produced by some animal cells after bacterial or viral infection? |
After viral infections |
|
|
Do Interferons interfere with Viral replication or bacterial reproduction? |
Viral replication |
|
|
Do interferons help the cell that produced them? |
No |
|
|
List the purposes of inflammation. |
1. Localize an infection; prevent the spread of a pathogen. 2. Neutralize toxins 3. Aid in repair of damaged tissue |
|
|
List the triggers of Inflammation. (5) |
1. Heat 2. Chemicals 3. UV light 4. Abrasion's, cuts. 5. Pathogens/pathogen products. |
|
|
List the signs and symptoms of inflammation. (4) |
1. Redness (due to increased circulation and Vasodilation) 2. Heat (given off by increased blood flow) 3. Swelling (increased fluid escaping into tissue) 4. Pain (stimulation of nerve endings due to swelling) |
|
|
Explain the inflammation process. |
When inflammation is triggered, damage cells release prostaglandins, histamine and leukotrienes |
|
|
How do Ibuprofin and aspirin reduce inflammation? |
Ibuprofin and aspirin are anti-prostaglandins. |
|
|
Define fever. |
Fever is a systemic response that has the body temperature above 100°F. |
|
|
What causes the hypothalamus to increase body temperature? |
Pyrogens cause the hypothalamus to increase body temperature. |
|
|
List 3 examples of Pyrogens |
1. Bacterial toxins 2. Antigen/antibody complexes 3. Pathogens |
|
|
List 5 purposes of fever |
1. Slow the growth rate/kill the pathogen 2. Increase phagocytosis 3. Increase specific immunity 4. Increase tissue repair 5. Increase effect of interferons |
|
|
Give one example of a fever reducing medication |
Tylenol |
|
|
Define specific (aka acquired) immunity |
The ability to recognize and defend against pathogens, pathogen products, and abnormal body cells. |
|
|
How do non specific and specific immunity work together to eliminate pathogens and pathogen products? |
Non specific immunity eliminates pathogens and specific immunity recognizes and defends against pathogens |
|
|
What line of defense are included in specific immunity? |
3rd line of defense. |
|
|
How can specific immunity be acquired? |
Specific immunity can be acquired naturally via infection or artificially via vaccination. |
|
|
Explain how specific immunity has memory. |
After an initial exposure, it recognizes and mounts a stronger attack on previously encountered pathogens or pathogen products. |
|
|
Explain how specific immunity is specific. |
It is specific due to the unique receptors of B and T cells. |
|
|
What type of immunity includes B cells and antibodies? |
Humoral immunity |
|
|
Give example of humoral immunity that includes B cells and the antibodies present in the body. (4) |
Blood, lymph, mucus, breast milk |
|
|
True or false: antibodies are produced by B cells. |
True |
|
|
What type of immunity includes T cells and antigens? |
Cell mediated immunity |
|
|
Cell mediated immunity targets: (3) |
1. Infected cells (virus, Parasite, bacteria) 2. Cancer cells 3. Cells of foreign grafts (tissue transplants) |
|
|
Cell mediated immunity kills via |
Chemicals |
|
|
What does the lymphatic system screen for in specific immunity? |
It screens for antigens. |
|
|
List the components of the lymphatic system |
1. Lymphatic vessels 2. Lymph nodes 3. Lymphoid organs/tissues |
|
|
What is lymph? |
Fluid that leaks out of the circulatory system |
|
|
What is the function of a lymph nodes in specific immunity question? |
Lymph nodes receive lymph from the lymphatic vessel and if an antigen is found, a specific immune response is mounted |
|
|
What is the function of lymphoid organs in specific immunity? |
Lymphoid organs include the spleen which filters blood and therefore removes pathogens. |
|
|
Explain how the lymphatic system is involved in specific immunity. |
Lymphatic vessels are a one way system. They return fluid that leaks out of the circulatory system (lymph) and into tissues back to the circulatory system. |
|
|
True or false: B and T cells in the lymph nodes screen the lymph for antigens |
True |
|
|
Define antigen. |
Molecule that triggers a specific immune response; antibody generator. |
|
|
Define epitope. |
The small part of an antigen that stimulates a specific immune response. |
|
|
Note: the specific immune system does not respond to the entire antigen just portions of them; these are called epitopes. Most antigens have several Epitopes. |
---- |
|
|
List the 2 types of antigens. |
1. Exogenous antigens 2. Endogenous antigens |
|
|
Define exogenous antigens. |
They are introduced into the body from outside microbes or environmental substances.They can be phagocytized by a phagocyte. |
|
|
Define Endogenous antigens |
They are generated within cells due to an infection by a microbe or due to the cell becoming cancerous. |
|
|
Name 3 things that reproduce/ Replicate inside body cells and produce endogenous antigens. |
1. Protozoa 2. Bacteria 3. viruses |
|
|
Name 4 examples of Exogenous antigens |
1. Bacterial toxins 2. Flagella 3. Pili 4. Bacterial cell wall components |
|
|
True or false: infected or abnormal cells must display these endogenous antigens on their membrane for the immune system to see. |
True |
|
|
Where do B cells arise in the body? Where do they mature? |
Arise in the red bone marrow and mature there as well. |
|
|
Do B cells leave the maturation area in an active or inactive state? |
Inactive state |
|
|
Where are inactive B cells found in the body? |
Found in the lymph nodes, lymphoid organs/tissues, and a small percentage circulate in the blood. |
|
|
Is a B cell receptor capable of binding more than one type of antigen? |
No |
|
|
What is the major function of B cells? |
The major function of B cells is the production of antibodies. |
|
|
Why is each B cell unique? |
Each B cell is unique because of their unique BCR. |
|
|
During clonal selection and activation of B cells: what selects the appropriate B cell? |
An antigen |
|
|
During colonel selection and activation of B cells: How specifically is the appropriate B cell selected? |
Since the antigen selects and binds to a BCR, it is very specific. |
|
|
During colonel selection and activation of B cells: By what process are clones produced? |
Clones are produced once activated B cells divide by mitosis. |
|
|
During clonal selection and activation of B cells: What types of T cells aid in the activation of B cells? |
T helper 2 cells |
|
|
During colonel selection and activation of B cells: List the 2 types of cells that B cell clones become |
1. Plasma cells 2. Memory B cells |
|
|
Define Plasma cells that some B cell clones become |
Plasma cells secrete antibodies in the body and produce 2,000 antibodies per second and function for 4-5 days. |
|
|
Define memory B cells that some of the B cell clones become. |
Memory B cells wait in case the same antigen is encountered again. They don't secrete antibodies. Can multiply quickly to produce more memory B cells and plasma cells if the same antigen is encountered again in the future. |
|
|
Define antibody. |
Proteins that bind to an antigen and tag it for the immune system to destroy |
|
|
What are the antigen binding sites on an antibody identical to? |
Identical to the activated BCR |
|
|
What cell produces antibodies? |
Plasma cells |
|
|
Where are antibodies found in the body? |
In the flydis in search of their specific antigen |
|
|
List 7 things that occur when antibody binds to an antigen. |
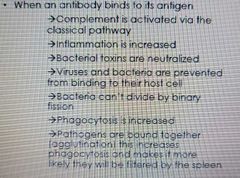
|
|
|
List the 5 classes of antibodies |
1. IgM 2. IgA 3. IgD 4. IgG 5. IgE |
|
|
Define IgM |
The first antibody produced. Short lived. (5%-10% circulating antibodies) |
|
|
Define IgA |
Found in respiratory tract, GI tracts, tears, saliva, colostridium, and in breast milk first produced. (10%-15% of circulating antibodies) |
|
|
Define IgD |
Acts as a B cell receptor on B cells. (0.2% of circulating antibodies) |
|
|
Define IgG |
Principle component of secondary antibody responses. Booster shots increase this antibody. (80% of circulating antibodies) |
|
|
Define IgE |
Allergic responses; lysis of helminthes. (Less than 0.1% of circulating antibodies) |
|
|
What do the classes of antibodies depend on for production? (3) |
The type of pathogen, portal of entry, and antibody functions. |
|
|
Define Primary Antibody Response |
The 1st time the antigen is encountered. There is a lag as it takes time to select and activate the correct inactive B cell. Memory B cells are produced. |
|
|
Define Secondary Antibody Response |
2nd and any additional times the antigen is encountered. There is a rapid response due to memory B cells. |
|
|
Where do T cells arise in the body? |
In red bone marrow |
|
|
Where do T cells mature? |
The Thymus |
|
|
Do T cells leave the maturation area in an active or inactive state? |
Inactive |
|
|
Where do inactive T cells circulate? |
In the Lymph, blood, lymph nodes and lymphoid organs/tissues |
|
|
Is a T cell receptor capable of binding more than one type of antigen? |
Yes |
|
|
Does a T cell receptor bind the antigen (epitope) directly? Explain |
No the TCR only binds epitope associated with MHC protein |
|
|
List the 2 types of T cells |
1. Cytotoxic T cells 2. Helper T cells |
|
|
Define Cytotoxic T cells. What do they have? |
Have a TCR and a CD8 coreceptor protein. Cytotoxic T cells recognize and kill infected and abnormal cells. |
|
|
Define Helper T cells What do they help? |
Have a TCR and a CD4 coreceptor protein. Helper T cells help in humoral and cell mediated immunity. |
|
|
What exactly are CD4 and CD8 coreceptors? |
Proteins found on the surface of Helper T cells (CD4) and Cytotoxic T cells (CD8) |
|
|
What is MHC? What does it let your immune system know? |
One of the proteins that dots the surface of our body cells. It helps your immune system determine self versus non self. |
|
|
List the 2 classes of MHC. |
1. MHC 1 2. MHC 2 |
|
|
What is the function of MHC? |
MHC proteins in a cell membrane mark a cell as "self." |
|
|
What type of cells display MH1 proteins? What type of cells recognize MH1 proteins? |
Found on the surface of all nucleated body cells (all cells but red blood cells) and is recognized by cytotoxic T cells. |
|
|
What type of cells display MH2 proteins? What type of cells recognize MH2 proteins? |
Found on the surface of antigen presenting cells (APC's) and is recognized by helper T cells. |
|
|
What specifically does MHC 1 display in its groove? |
"Non" self epitopes |
|
|
What specifically does MHC 2 display in its groove? |
Exogenous antigens. |
|
|
What cells display both MHC1 and MHC2? |
Antigen presenting cells (APC's) |
|
|
List the 2 things that cell mediated immunity is used to fight. |
1. Infected cells 2. Abnormal cells |
|
|
To be activated, a helper T cell must recognize epitope with ___________? |
MHC 2 |
|
|
To be activated, a cytotoxic T cell must recognize epitope with ______ |
MHC 1 |
|
|
Pathogens enter via a ______? |
Portal of entry |
|
|
An ______ phagocytizes the pathogen |
APC |
|
|
Inside the APC, the antigen is sent to the lysosome and broken down by the _______ in the lysosome into ______ |
Enzymes; epitopes |
|
|
Epitopes are displayed on the surface of the APC in the groove of _____ |
MHC 2 |
|
|
The APC migrates to the nearest _____ or ______ |
Lymph node or lymphoid organ/tissues |
|
|
A match happens when APC displaying ______ in ______ match ______ helper T cell _____ and _____ coreceptor |
Epitopes; MHC 2; Inactive; TCR; CD4 |
|
|
Once a match happens, the APC secretes ______. The active helper T cell divides by _____ to produce _____. |
Cytokines; mitosis; clones |
|
|
Some of the helper T cell clones become _______ T cells and wait for future encounters with the same antigen |
Memory |
|
|
The majority of helper T cell clones become ____ and _____ cells |
T helper 1 (TH1) ; T helper 2 (TH2) |
|
|
T helper _____ cells produce cytokines that activate other immune cells |
1 |
|
|
T helper _____ cells produce cytokines that activate B cells and stimulate antibody production by plasma cells |
2 |
|
|
When a cell is infected with a pathogen it displays _______ epitopes on its surface in the grove of MHC _____ |
Pathogen; 1 |
|
|
When a cell is abnormal it displays I AM _____ epitopes on its surface in the groove if MHC |
Abnormal; 1 |
|
|
A match happens when infected/abnormal epitope in MHC1 matches _____ cytotoxic T cell ___ and CD__ coreceptor |
Inactive; TCR; CD8 |
|
|
Activated T helper _____ cells produce chemical signals that help activate the cytotoxic T cell. |
1 |
|
|
The activated cytotoxic T cells divides by ______ to produce _____ |
Mitosis; clones |
|
|
Some of the cytotoxic T cell clones become _____ cells and wait for future encounters with the same antigen. |
Memory T |
|
|
The majority of the cytotoxic T cell clones go in search of more of the same infected/abnormal cells and kill via _____ |
Chemicals |
|
|
When does active immunity develop? What does it produce? |
Develops when the immune system responds to an antigen. Produces antibodies against the antigen. |
|
|
When does Passive Immunity develop? |
Develops when an antibody enters from an outside source. |
|
|
How long does passive immunity last? |
Days to weeks. |
|
|
How long does active immunity take to develop? |
Takes hours to days to develop |
|
|
Passive Immunity can be acquired _____ via Ig_ transfer from mom to fetus and Ig_ transfer via colostrum and breast milk |
Naturally; IgG; IgA |
|
|
Active immunity can be acquired naturally via ___ or artificially via _______________ |
Infection; exposure to the antigen in a vaccine |
|
|
Define vaccination. |
Inoculation with a weakened or dead microbe or microbe product to generate immunity and prevent infectious disease. |
|
|
Define immunization. |
Making an individual resistant to a disease via vaccine. |
|
|
Give the _____ to produce _____ against the antigen and ____ B and T cells. |
Antigen; antibodies; memory |
|
|
Define herd immunity. |
A form of immunity that occurs when the vaccination of a significant portion of a population provides a measure of protection for individuals who have not developed immunity. |
|
|
What is the percentage of vaccination rate needed for heard immunity to be effective? |
95% |
|
|
Define attentuated vaccine. |
Weaken a virus in the lab so that the virus cannot cause disease. Can give lifelong immunity in just one- two doses due to strong humoral and cell mediated immune responses. |
|
|
Define inactivated vaccine. |
Kill the pathogen using chemicals, heat, radiation. Booster shots will be required. |
|
|
Define toxoid vaccines. |
Bacterial exotoxin is the main cause of illness. Inactivate the toxin with formalin. Formalin will alter the epitopes slightly so booster shots will be required. |
|
|
Define subunit vaccines. |
Includes only parts of the pathogen. |
|
|
Define conjugate vaccine. |
The pathogen is a bacteria that produces a capsule that covers the entire bacterium. Capsules are not very antigenic. |
|
|
Define mRNA vaccine. |
mRNA sequence is generated for the antigen. The mRNA is covered in a lipid for delivery. Once delivered, cells will transcribe and translate the mRNA into protein. The presence of the epitope will stimulate a specific immune response. |
|
|
List the 5 ingredients in vaccines. |
1. Suspending fluid. 2. Stabilizers. 3. Preservatives. 4. Adjuvants. 5. Small amount of the culture material |

