![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
249 Cards in this Set
- Front
- Back
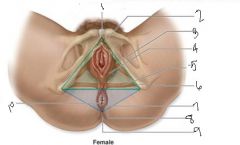
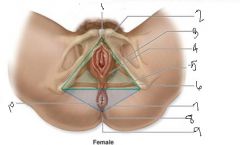
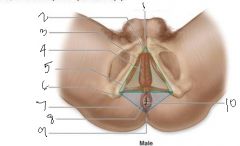
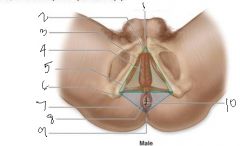
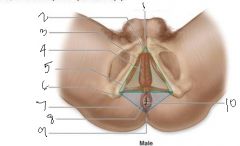
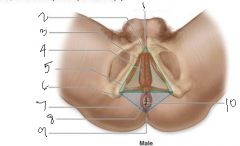
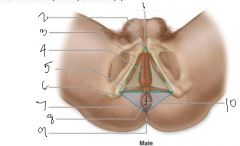
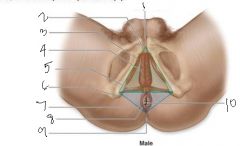
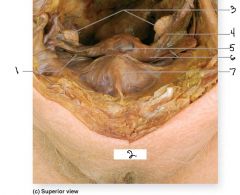
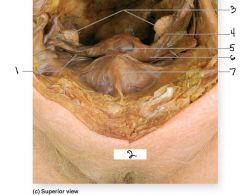
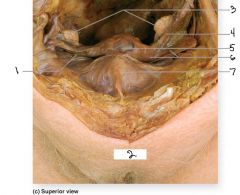
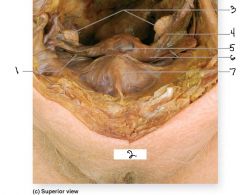
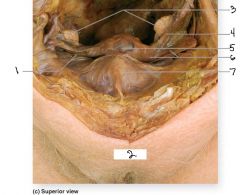
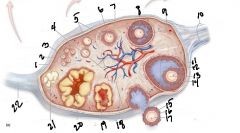
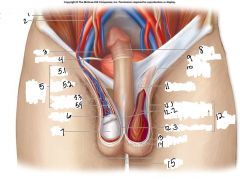
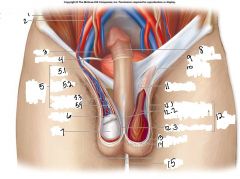
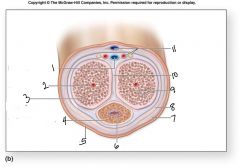
#1
|
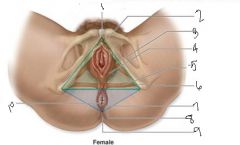
pubic symphysis
|
|
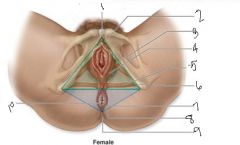
#2
|
Urogenital triangle
|
|
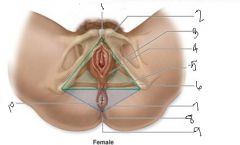
#3
|
ischiocavernosus muscle
|
|
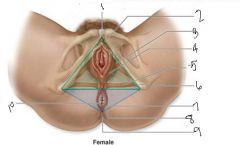
#4
|
bulbospongiosus
|
|
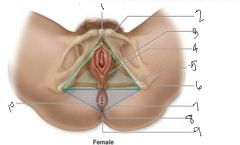
5
|
superfiscial transverse perineal muscle
|
|
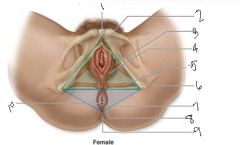
6
|
ischial tuberosity
|
|
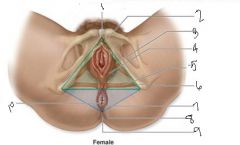
7
|
anal triangle
|
|
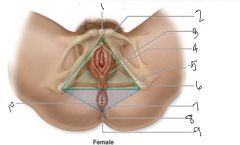
8
|
external anal sphinchter
|
|
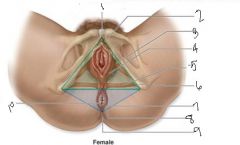
9
|
coccyx
|
|
10
|
anus
|
|
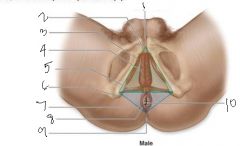
identify this picture
|
male perineum
|
|
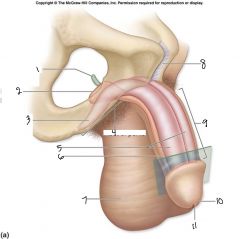
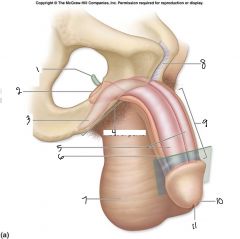
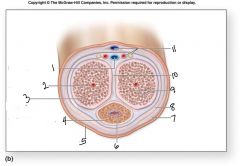
1
|
pubic symphysis
|
|
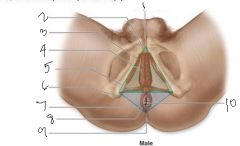
3
|
ischiocavernosus muscle
|
|
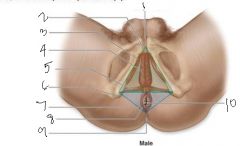
4
|
bulbospongiosus muscle
|
|
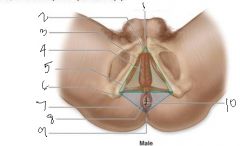
2
|
Urogenital triangle
|
|
5
|
superficial transverse perineal muscle
|
|
6
|
ischial tuberosity
|
|
7
|
anal triangle
|
|
8
|
external anal sphincter
|
|
9
|
coccyx
|
|
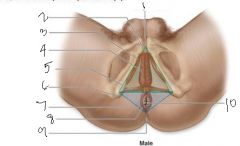
10
|
anus
|
|
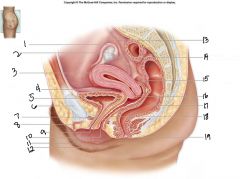
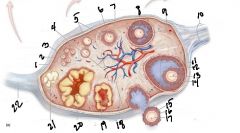
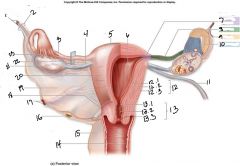
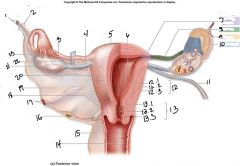
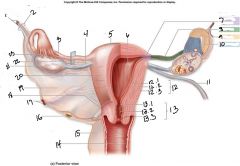
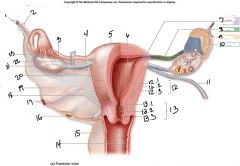
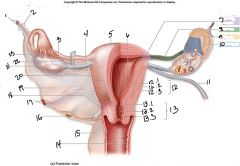
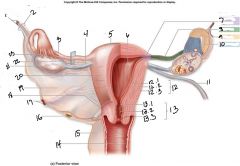
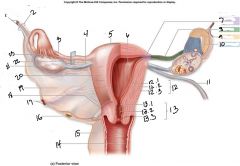
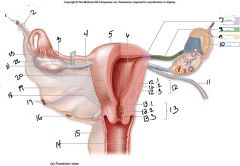
what is this a picture of
|
female reproductive system
|
|
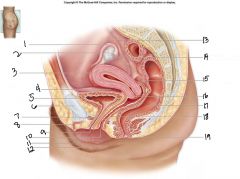
1
|
uterine tube
|
|
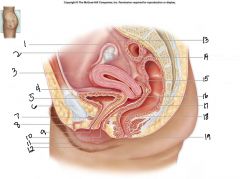
2
|
ovary
|
|
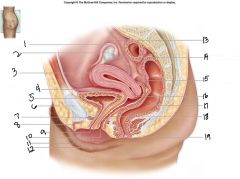
3
|
uterus
|
|
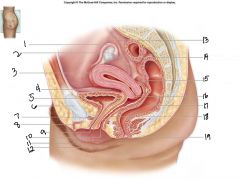
4
|
vesicouterine pouch
|
|
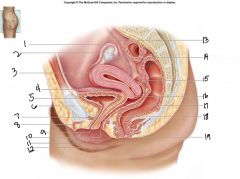
5
|
urinary bladder
|
|
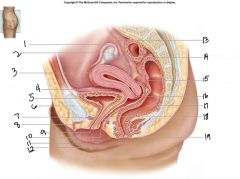
6
|
pubic symphysis
|
|
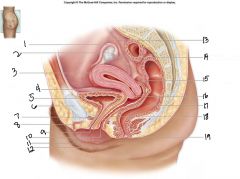
7
|
urethra
|
|
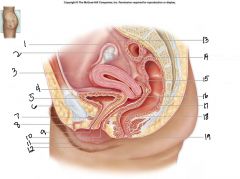
8
|
clitoris
|
|
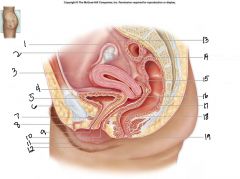
9
|
external urethral orifice
|
|
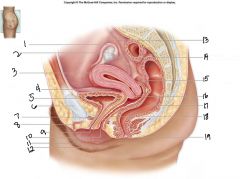
10
|
vaginal orifice
|
|
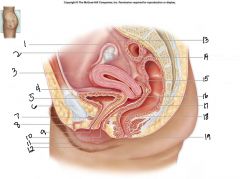
12
|
labium major
|
|
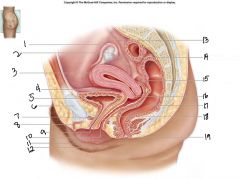
13
|
ureter
|
|
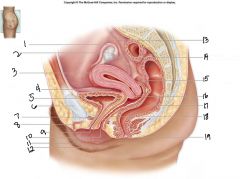
14
|
fimbriae of uterine tube
|
|
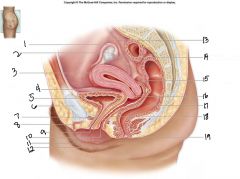
15
|
rectouterine pouch
|
|
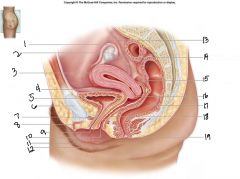
16
|
cervix of uterus
|
|
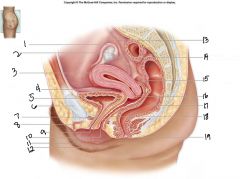
17
|
rectum
|
|
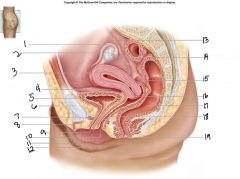
18
|
vagina
|
|
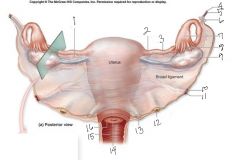
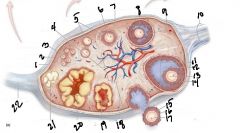
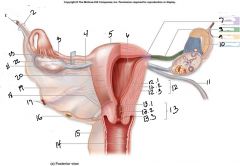
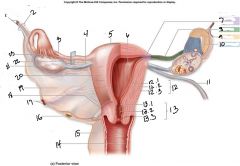
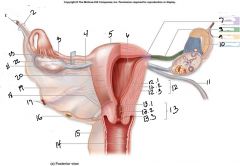
1
|
mesosalpinx
|
|
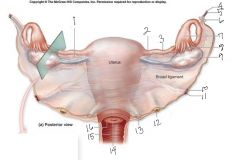
2
|
ovarian ligament
|
|
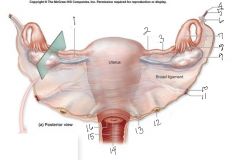
3
|
uterine tube
|
|
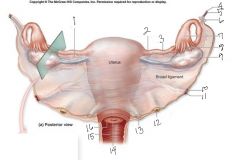
6
|
suspensory ligament
|
|
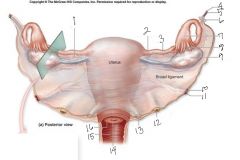
7
|
infundibulum
|
|
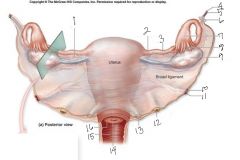
8
|
fimbriae
|
|
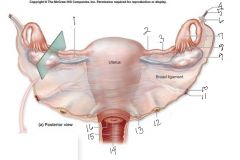
9
|
ovary
|
|
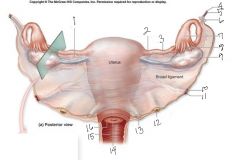
10
|
uterine artery
|
|
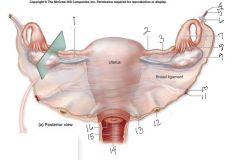
11
|
uterine vein
|
|
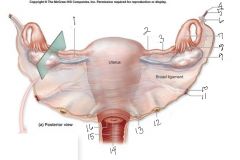
12
|
ureter
|
|
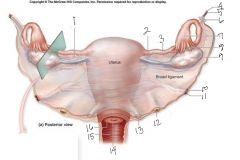
13
|
uterosacral ligament
|
|
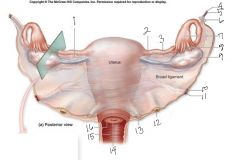
14
|
external os
|
|
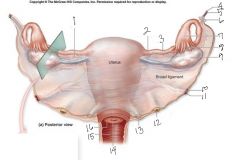
15
|
vagina
|
|
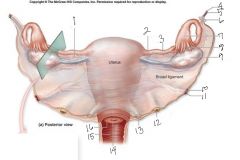
16
|
cervix
|
|
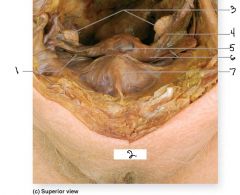
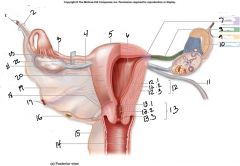
1
|
round ligament
|
|
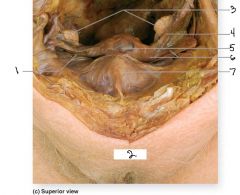
2
|
mons pubis
|
|
3
|
ovaries
|
|
4
|
uterine tube
|
|
5
|
uterus
|
|
6
|
broad ligament
|
|
7
|
urinary bladder
|
|
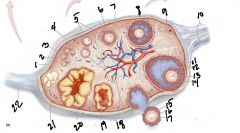
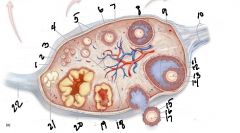
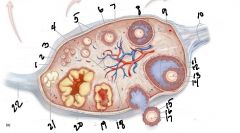
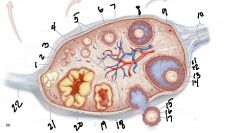
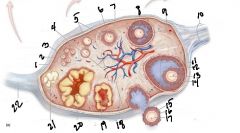
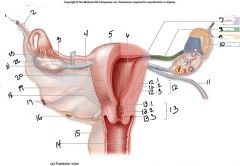
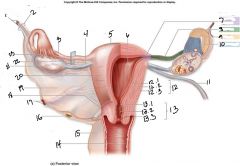
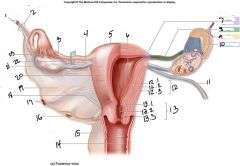
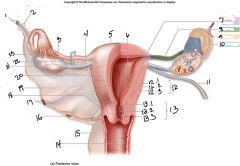
1
|
germinal epithelium
|
|
2
|
tunica albuginea
|
|
3
|
primordial follicles
|
|
6
|
primary oocyte
|
|
7
|
granulosa cells
|
|
8
|
secondary follicle
|
|
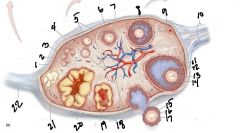
9
|
antrum
|
|
10
|
suspensory ligament of the ovary
|
|
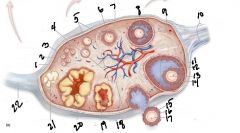
11
|
vesicular follicle
|
|
12
|
antrum
|
|
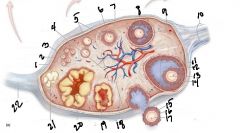
13
|
secondary oocyte
|
|
14
|
zona pellucida
|
|
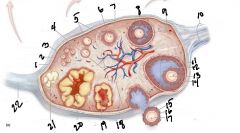
15
|
corona radiata
|
|
17
|
ovulated secondary oocyte
|
|
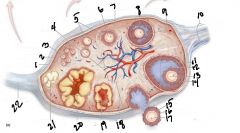
18
|
cortex
|
|
19
|
developing corpus luteum
|
|
20
|
corpus luteum
|
|
21
|
corpus albicans
|
|
2
|
suspensory ligament
|
|
1
|
ovarian blood vessels
|
|
3
|
uterine tube
|
|
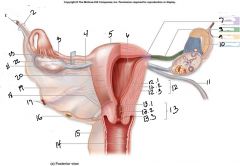
4
|
ovarian ligament
|
|
5
|
fundusof the uterus
|
|
6
|
lumen of the uterus
|
|
8
|
isthmus
|
|
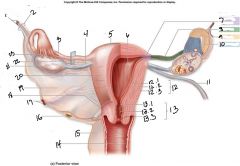
9
|
ampulla
|
|
10
|
infundbulum
|
|
12
|
wall of the uterus
|
|
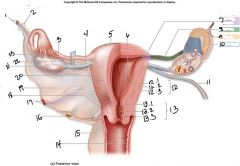
12.1, 12.2, 12.3
|
12.1-endometrium
12.2-myometrium 12.3-perimetrium |
|
13
|
cervix
|
|
13.1, 13.2, 13.3
|
13.1-internal os
13.2-cervical canal 13.3-external os |
|
14
|
vagina
|
|
15
|
transverse cervical ligament
|
|
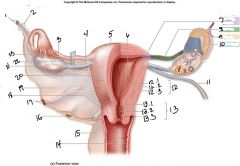
16
|
ureter
|
|
17
|
uterine blood vessels
|
|
18
|
isthmus
|
|
19
|
broad ligament
|
|
20
|
body of uterus
|
|
|
23
|
fimbriae
|
|
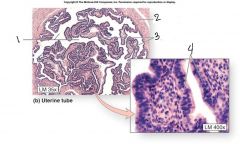
1, 2, 3, 4
|
1. lumen of uterine tube, 2. muscularis, 3. mucosa, 4. simple ciliated clomnar epithelium
|
|

1
|
endometrium
|
|

1.1, 1.2
|
1.1-functional layer
1.2-basal layer |
|

2
|
myometrium
|
|

3
|
epithelium
|
|

4
|
uterine glands
|
|

5
|
lamina propia
|
|
|
what is this a picture of
|
2 of the 3 tunics of the uterus. the perimetrium is missing
|
|

what is this a picture of
|
2 of the 3 tunics of the uterus. the perimetrium is missing
|
|
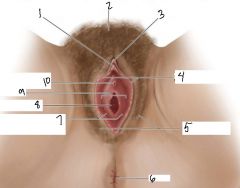
1
|
glans of clitoris
|
|
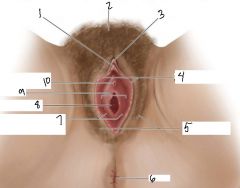
2
|
mons pubis
|
|
|
3
|
prepuce
|
|
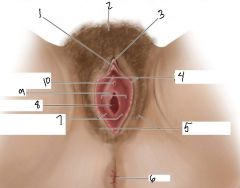
3
|
prepuce
|
|
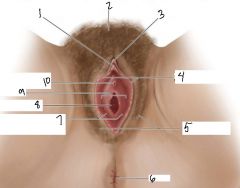
4
|
labia minora
|
|
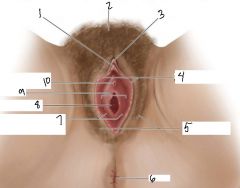
5
|
labia majora
|
|
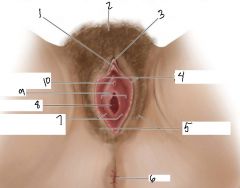
6
|
anus
|
|
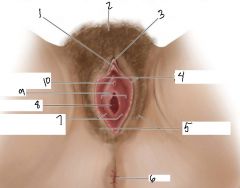
10
|
urethral opening
|
|
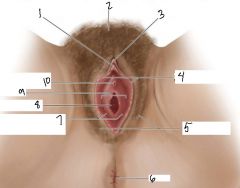
7
|
openings for greater vestibular gland
|
|
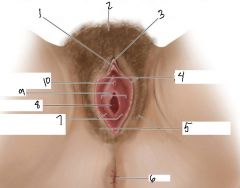
9
|
vestibule
|
|
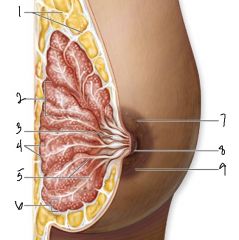
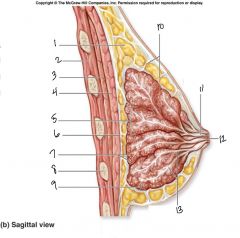
1
|
suspensory ligaments
|
|
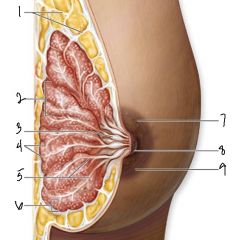
2
|
lobe
|
|
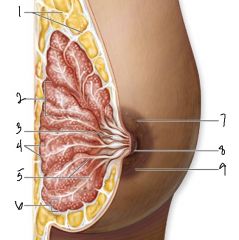
4
|
alveoli
|
|
5
|
lactiferous ducts
|
|
6
|
lobule
|
|
8, 9
|
8-nipple
9-areola |
|
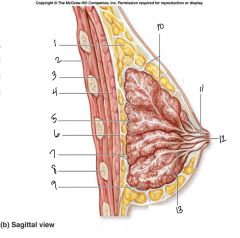
1
|
adipose tissue
|
|
2
|
intercostal muscle
|
|
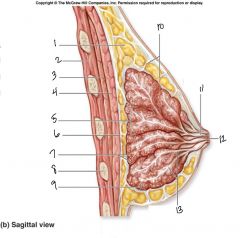
3, 4
|
3. pectoralis minor
4. pectoralis major |
|
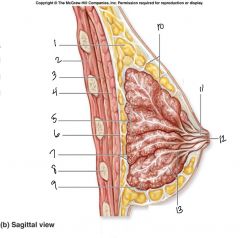
7
|
alveoli
|
|
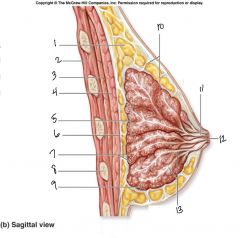
8
|
Rib
|
|
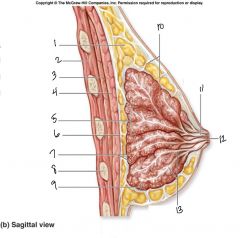
9
|
lobule
|
|
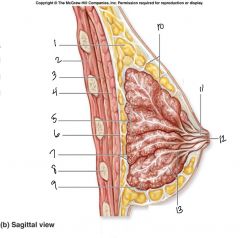
10
|
suspensory ligaments
|
|
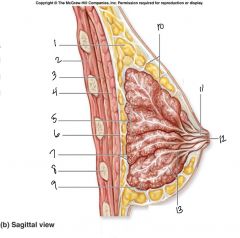
11, 12, 13
|
11. lactiferous sinus
12. nipple 13. lactiferous ducts |
|
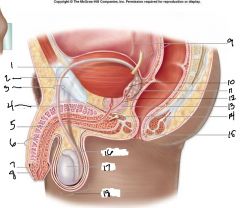
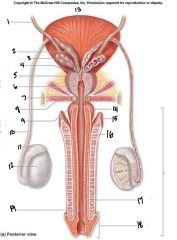
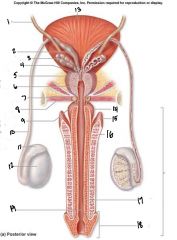
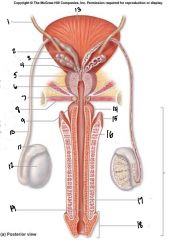
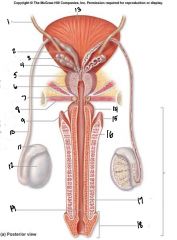
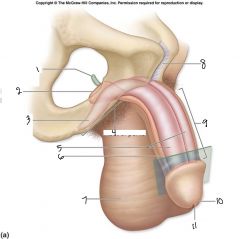
1, 2, 3
|
1. urinary bladder
2. pubic symphysis 3. ductus deferens |
|
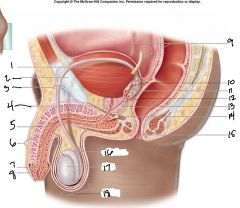
4
|
urogenital diaphragm
|
|
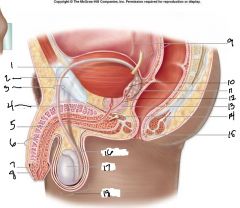
5
|
urethra
|
|
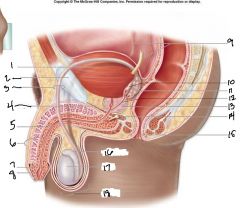
6, 7, 8
|
6. penis.
7. glans 8. prepuce |
|
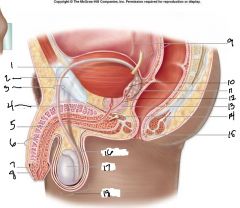
9
|
ureters
|
|
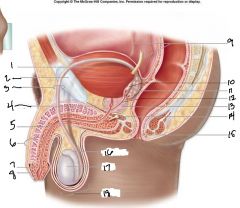
10, 11, 12
|
10. ampulla of ductus deferens
11. seminal vesicle 12. ejaculatory duct |
|
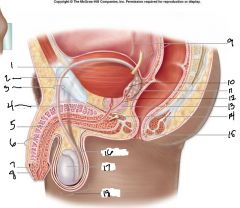
16, 17, 18
|
16. epididymis
17. testis 18. scrotum |
|
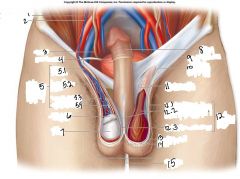
1, 2
|
1. Testicular artery
2. Testicular vein |
|
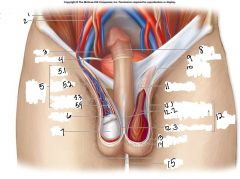
3, 4
|
3. ureter
4. urinary bladder |
|
5 structure within the spermatic cord.
5.1, 5.2, 5.3, 5.4 |
5.1 ductus deferens
5.2 pampiniform plexus 5.3 testicular artery 5.4 testicualr vein |
|
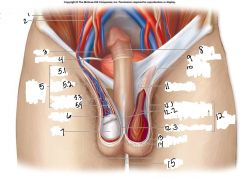
6, 7
|
6. epididymis
7. testis |
|
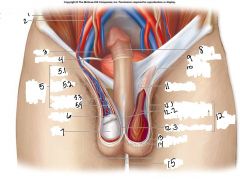
8, 9
|
8. penis
9. inguinal ligament |
|
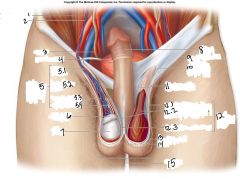
10, 11
|
10. superficial inguinal ring
11. spermatic cord |
|
12 layers of the spermatic cord
12.1, 12.2, 12.3 |
12.1 external spermatic fascia
12.2 cremaster muscle within the crematic fascia 12.3 internal spermatic fascia |
|
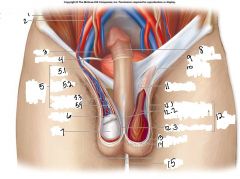
13, 14, 15
|
13. dartos muscle
14. raphe 15. scrotum |
|
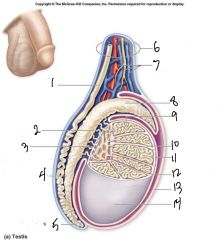
4,5
|
4. body of epididymis
5. tail of epididymis |
|
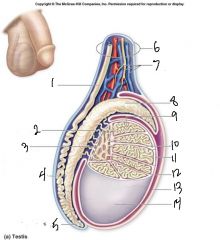
10,11
|
10. septum
11. lobule |
|
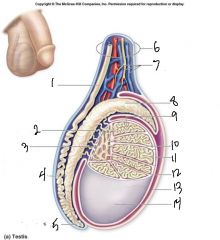
12,13,14
|
12. Visceral layer of tunical vaginalis
13. parietal layer of the tunical vaginalis 14. tunica albuginea |
|
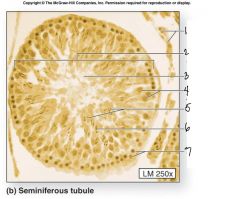
1, 2, 3
|
1. interstitial cells
2. seminiferous tubule 3. tubule lumen |
|
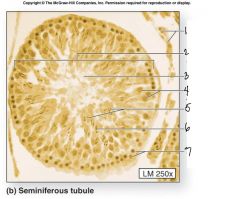
4,5
|
4. sustentacular
5. sperm cells |
|
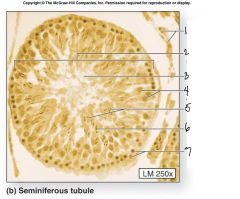
6,7
|
6. spermatids
7. spermatogonia |
|
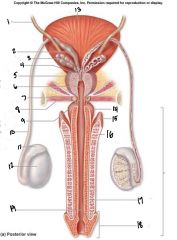
1, 13
|
1. ureter
13. urinary bladder |
|
2, 3, 4
|
2. ampulla
3. seminal vesicle 4. ejaculatory duct |
|
5, 6, 7
|
5. prostate gland
6. prostatic urethra 7. bulbourethral gland |
|
8, 9
|
8. urogenital diaphragm
9. membranous urethra |
|
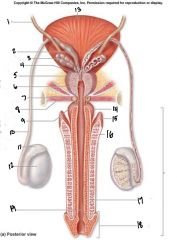
10, 11, 12
|
10. ductus deferens
11. epididymis 12. testis |
|
14, 15, 16
|
14. bulb
15. crus 16. corpus cavernosum |
|
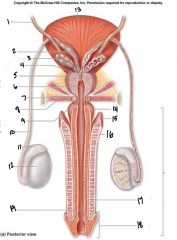
17, 18, 19 and the bracket on the right side
|
17. corpus spongiosum
18. glans 19. penile urethra - penis |
|
1,2, 3
|
1. membranous urethra
2. bulb of the penis 3. right crus of the penis |
|
4, 5, 6, 7
|
4. root of the penis
5. corpora cavernosa 6. corpus spongiosum 7. scrotum |
|
8, 9, 10, 11
|
8. pubic symphysis
9. body of the penis (shaft) 10. glans 11. external urethral orifice |
|
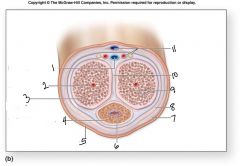
1, 2, 3
|
1. Deep dorsal vein
2. central artery 3. Corpus cavernosum |
|
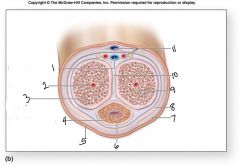
4, 5, 6
|
4. Corpus spongiosum
5. skin 6. penile urethra |
|
11
|
blue - dorsal vein
red - artery yellow - nerve |
|
7, 8, 9, 10
|
7. superficial fascia
8. deep fascia 9. venous spaces 10. tunica albuginea |
|
|
Ch 28 – Reproductive System
|
|
|
|
1 a. Compare the anatomy of female to male reproductive system, noting the similarities (homologues) as well as the differences.
|
The male and female reproductive systems are similar with respect to their fuction in producing sex cells. They begin with similar homologues but then differentiate to for the male and female reproductive systems. They also both produce sex hormones (testosterone - male; androgen and progesterone - female). they differ in external structure where the male reproductive organs exteds outside the body.
|
|
|
b. Give some reasons to explain these similarities and differences.
|
They both come from the same types of cells during development but then differentiate when exposed to specific hormones. Their differences come from the function they serve. For the male the delivery of the sperm cell to the oocyte. The woman's the protection of the oocyte.
|
|
|
2 a. Trace the path of an ovum through the reproductive organs/structures. Include the different parts of the uterine/fallopian tubes.
|
The Ovum begins in the Ovary, travels through the uterine tube (passing the fimbriae, infundibulum, ampulla, isthmus, and the interstitial segement)into the uterus.
|
|
|
b. PID is pelvic inflammatory disease, caused by sexually transmitted infections, resulting in scarring and narrowing of the fallopian tubes. What problems should a patient with PID worry about?
|
Problems associated with PID are infertility, ectopic pregnancy,abcess formation and chronic pelvic pain.
|
|
|
3 a. How is the female reproductive system held in place?
|
By Ligaments such as the broad ligament, trnasverse cervical ligament and the ovarian ligament.
|
|
|
b. As women grow older, these supports weaken. What problems may appear?
|
Over time the ligaments weaken and may lead to prolapse of the reproductive organs.
|
|
|
4 a. In chronological order, describe the development of the ovum in the ovary.
|
Primordial follicle, primary follicle, secondayr follicle, vesicualr follicle, ovulated secondary oocyte, oogonium, undergoes mitosis, primary oocyte, secondary oocyte.
|
|
|
b. Do all women complete meiosis every month? Why/Why not?
|
If a woman is not producing an ovum due to menopause or pregancy they do go through meisis every month.
|
|
|
5 a. Describe the layers of the uterus.
|
The uterus consists of 3 layers for superficial to deep; perimetrium, myometrium, and the endometrium.
|
|
|
b. Briefly explain how does the endometrium support a pregnancy?
|
The endometrium is where a fertilized ovum embeds itself.
|
|
|
6 a. Compare the epithelium of the vagina to that in the uterus and to that in the fallopian tubes.
|
the uterus is lined with simple columbnar epithelium, the vagina is lined with non-keratinized stratified squamous epithelium, and the falopian tubes are lined with ciliated columbnar epithelium.
|
|
|
b. How is each epithelium appropriate for that location?
|
The cilia in the fallopian tube assist in the movement of an ovum through the tube. The Vagina is an external surface of the body that is covered in mucus. Finally, the uterus
|
|
|
7 a. Trace the path of sperms through the male and female reproductive organs/structures.
|
The sperm travels from the testes, the epididymis, the ducuts deferens, the ampulla of the ductus deferense, the seminal vesicle, the ejaculaory ducts, the urethra, then into the female reporductive system through the Vagina, then the uterus (through the exteral os, cervical canal, and the interna os.
|
|
|
b. Vasectomy is tying the vas/ductus deferens in the scrotal sac. Why is this ideal?
|
It stops the travel of the sperm before it leaves the scrotum and it is easly accessable because the structure is outside the pelvic cavity.
|
|
|
|
|
|
|
8 a. From superficial to deep, list the layers of the spermatic cord. Also, define the spermatic cord.
|
external spermatic fascia, cremasteric muscle and fascia, internal spermatic fascia,
|
|
|
b. Why is it so external? Can it change position? Why/why not?
|
It help keep the sperm cells cool and it is able to change postion because if its fleable strucutre.
|
|
|
9 a. Compare the structure and meiosis of an ovum to a sperm.
|
The structure of ovum and spern are very different. Spern are designed to be mobile and have a flagellum. During meiosis the sex cells both divide and only contain half of the chromosomes that regualr cells contain. The sperm undero meiosis very rapidly.
|
|
|
b. Why is there a big difference in size and number?
|
Many more sperm are created bacause only one can reach the ovum. The rest die off.
|
|
|
10 a. Compare the hormones in the female to male reproductive system. How are they alike? Different?
|
The hormones in both male and females is produced in the gonads. The differ in that the male hormone stimulates growth in muscalture and broader shoulders. The female hormone stimuates growth of breasts and wider hips for child bearing.
|
|
|
b. Explain how the hypothalamus, pituitary, and gonads all cooperate for normal function.
|
The hypothalamus send the signal to release a specific hormone to the pituitary, The pituitary releases a hormone that stimulates the production of the male or female sex hormone.
|
|
|
11 a. What are the accessory glands in the male reproductive system? Why are they necessary?
|
the male accesory glands are the seminal vesicles, prostate gland, and the bulbourethral glands. The vagina is acidic and these glands create a seminal fluid which lesses the pH of the vagina allow the spern to survive.
|
|
|
b. Which has the highest potential to become enlarged? What problems may result with enlargement?
|
The prostate has the highest potential to become enlarged. When this happened it squeezes the urtetha closed not allowing sperm and urine to leave the body.
|
|
|
Gonads
|
primary reproductive organs that produce gamates and hormones. They also produce large amounts of sex hormones which affect maturation, development, and changes in the activity of the reproductive system organs
|
|
|
Testes
|
counterpart to ovaries, which are homologous, they are components of both reproductive system (being gonads) and the endocrine system (being endocrine glands). They produce sperm, and male sex hormones such as testosterone. They also produce LH and FSH.
|
|
|
Ovaries
|
small paired organs located near the lateral walls of the pelvic cavity. It is responsible for the production of ova and the secretion of hormones.
|
|
|
Gametes
|
Reproductive cells
|
|
|
Sperms
|
Male produces 100,000,000’s of (sperm) daily. Male gametes are stored for a short time if they are not expelled from the body within that period, they are resorbed
|
|
|
Oocytes
|
Female typically produces and releases a single oocyte monthly
|
|
|
Bulbourethral
|
secretes male mucous for lubrication
|
|
|
Vestibular
|
secretes female mucous for lubrication
|
|
|
Scrotum
|
protects some male reproductive structures.
|
|
|
Labia Majora
|
protects some female reproductive structures.
|
|
|
Glans of Penis
|
Male stimulation site. Contains autonomic nervous system axons that stimulate arousal and sexual climax feelings.
|
|
|
Clitoris
|
Female. Contains autonomic nervous system axons that stimulate arousal and sexual climax feelings
|
|
|
Androgens (Testosterone)
|
A hormone steroid produced in the testis, ovary, adrenal, and most likely, in the placenta. A small portion of the androgen is from corticoids, or adrenal cortex steroids, and from other C21 steroids, such as progesterone.
|
|
|
Progesterone
|
is a steroid hormone that primarily function is to continue to prepare the uterus for pregnancy (menstrual cycle) as well as support gestation.
|
|
|
Estrogen
|
steroid hormone, named functions ss the primary female sex hormone. The three major naturally occurring estrogens in women are estrone (E1), estradiol (E2), and estriol (E3). Estradiol (E2) is the predominate form in nonpregnant females, estrone is produced during menopause, and estriol is the primary estrogen of pregnancy. In the body these are all produced from androgens through actions of enzymes.
|
|
|
Gonadotropin-Releasing Hormone (GnRH)
|
produced by the hypothalamus and the end of the ovulation cycle, this hormone triggers a rise in FSH and LH production by the anterior lobe of the pituitary gland, this gives rise to another period of follicle development.
|
|
|
Perineum
|
Diamond-shaped area between the thighs that is circumscribed anteriorly by the pubic symphysis, laterally by the ischial tuberosities, and posteriorly by the coccyx. 2 distinct triangle bases are formed by an imaginary horizontal line extending between the ischial tuberosities of the ossa coxae.
|
|
|
Ovaries
|
produce gamates and sex hormones
|
|
|
Mesovarium
|
a thickened fold of the broad ligament, this supports and stabilizes the position of each ovary.
|
|
|
Ovarian Ligament
|
supporting ligament that extends from the lateral wall of the uterus near the attachment of the uterine tube to the medial surface of the ovary.
|
|
|
Broad Ligament
|
an extensive mesentery which encloses the ovaries, uterine tubes, and uterus. The broad ligament attaches to the sides and floor of the pelvic cavity where it becomes continuous with the parietal peritoneum.
|
|
|
Suspensory Ligament
|
extends from the lateral surface of the ovary past the open end of the uterine tube to the pelvic wall.
|
|
|
Ovarian Artery, Vein, Nerve
|
Major blood vessels travel to and from the ovary within the suspensory ligament. They extend through the mesovarium along the nerves and lymphatic vessels, and are connected to the ovary at the ovarian hilum.
|
|
|
Tunica Albuginea
|
Dense CT covering the ovaries located on the surface of the ovary .
|
|
|
Cortex
|
The interior of the ovary can be divided into a superficial cortex and a deep medulla.
|
|
|
Corpus Albicans
|
is the regressed form of the corpus luteum. As the corpus luteum is being broken down by macrophages, fibroblasts lay down type I collagen, forming the corpus albicans. This process is called "luteolysis". The remains of the corpus albicans may persist as a scar on the surface of the ovary.B77
|
|
|
Medulla
|
is a highly vascular stroma in the center of the ovary. It forms from embryonic mesenchyme and contains blood vessels, lymphatic vessels, and nerves.This stroma forms the tissue of the hilum by which the ovarian ligament is attached, and through which the blood vessels enter
|
|
|
Ovarian Cycle
|
3 phases (1) follicular (2) ovulation (3) luteal phase
|
|
|
Follicular Phase
|
occupies days 1–13 of an approximate 28-day ovarian cycle.
|
|
|
Inhibin
|
is a protein complex that inhibits FSH secretion.
|
|
|
Polar Body
|
is a cell structure found inside an ovum. It is also known as a polar cell.Production of polar cells occurs during oogenesis. To conserve nutrients, the majority of cytoplasm is segregated into either the secondary oocyte or ovum, during meiosis I or meiosis II, respectively. The remaining daughter cells generated from the meiotic events contain relatively little cytoplasm and are referred to as polar bodies. Eventually, the polar bodies degenerate.
|
|
|
Ovulation
|
occurs on day 14 of a 28-day ovarian cycle and is defined as the release of the secondary oocyte from a vesicular follicle. Only one ovary ovulates each month.
|
|
|
Luteal Phase
|
occurs during days 15–28 when the remaining follicle cells in the ruptured vesicular follicle turn into a corpus luteum. Secretes progesterone and estrogen that stabilize and build up the uterine lining, and prepare for possible implantation of a fertilized oocyte. Has a life span of about 10–13 days if the secondary oocyte is not fertilized it regresses and becomes a corpus albicans.
|
|
|
Menarche
|
The first menstrual period, usually occurring during puberty
|
|
|
Pregnancy
|
is the carrying of one or more offspring, known as a fetus or embryo, inside the uterus of a female
|
|
|
Implantation
|
is an event that occurs early in pregnancy in which the embryo adheres to the wall of uterus. At this stage of prenatal development, the embryo is a blastocyst. It is by this adhesion that the fetus receives the oxygen and the nutrients from the mother to be able to grow.
|
|
|
Human Chorionic Gonadotropin (hCG)
|
is a glycoprotein hormone produced in pregnancy made by the developing embryo soon after conception and later by the syncytiotrophoblast (part of the placenta). It helps to prevent the disintegration of the corpus luteum of the ovary and thereby maintain progesterone production that is critical for a pregnancy in humans. hCG may have additional functions; for instance, it is thought that hCG affects the immune tolerance of the pregnancy.
|
|
|
Menopause
|
is the time in a woman’s life when menstruation (having a period) ends. It is part of a biological process that begins, for most women, in their mid-fifties. During this time, the ovaries gradually produce lower levels of natural sex hormones—estrogen and progesterone
|
|
|
Oviducts = Uterine/Fallopian Tubes
|
Uterine/Fallopian Tubes
|
|
|
Mesosalpinx
|
is part of the lining of the abdominal cavity in higher vertebrates, specifically the portion of the broad ligament that stretches from the uterine tube to the level of the ovary.
|
|
|
Infundibulum
|
The end of the mammal oviduct nearest to the ovary is the infundibulum of uterine tube
|
|
|
Fimbriae
|
a fringe of tissue near the ovary leading to the fallopian tube.
|
|
|
Ampulla
|
is the second portion of the uterine tube. It is an intermediate dilated portion, which curves over the ovary. It is the most common site of human fertilization.
|
|
|
Uterus
|
provides mechanical protection, nutritional support and waste removal for the developing embtyo and fetus. Contractions in the muscular wall of the uterus help to eject the fetus at birth after maternal oxytocin levels increase to initiate the uterine contractions of labor. Site for menstruation. If an oocyte is not fertilized or after a baby is expelled, the muscular wall of the uterus contracts and sheds its inner lining as menstruation. It is composed of 3 tunics. Perimetrium, Myometrium, endometrium.
|
|
|
Fundus
|
is the rounded portion of the body superior to the attachment of the uterine tubes.
|
|
|
Body
|
also known as corpus is the largest region in the uterus.
|
|
|
Isthmus
|
The ampulla leads to a short segment adjacent to the uterine wall.
|
|
|
Cervix
|
of the uterus projects about 1.25 CM into the vagina. The distal end of the cervix forms a curving surface surrounding the external opening of the uterus.
|
|
|
Cervical Canal
|
a constricted passageway that opens into the uterine cavity of the body at the internal os.
|
|
|
Internal & External Os
|
The external os leads into the cervical canal from the cervix.
|
|
|
Round Ligaments
|
arise on the lateral margins of the uterus just inferior to the base of the uterine tubes. They extend anteriorly passing through the inguinal canal before ending in the CT of the external genetalia.
|
|
|
Perimetrium
|
The outer tunic of most of the uterus is a serosa called the perimetrium. It is continuous with the broad ligament
|
|
|
Myometrium
|
Is the thick, middle tunic of the uterine wall formed from three intertwining layers of smooth muscle. In the nonpregnant uterus, the muscle cells are less than 0.25 millimeters in length during the course of a pregnancy, smooth muscle cells increase both in size and in number.
|
|
|
Uterine Cycle
|
known as the menstrual cycle. The menstrual phase occurs approximately during days 1–5 of the cycle. This phase is marked by sloughing of the functional layer and lasts through the period of menstrual bleeding.
|
|
|
Proliferative Phase
|
follows, spanning approximately days 6–14. The initial development of the functional layer of the endometrium overlaps the time of follicle growth and estrogen secretion.
|
|
|
Secretory Phase
|
which occurs at approximately days 15–28. During the secretary phase, increased progesterone secretion from the corpus luteum results in increased vascularization and development of uterine glands.
|
|
|
Menstruation
|
If the oocyte is not fertilized, during the secretory phase, the corpus luteum degenerates, and the progesterone level drops dramatically. Without progesterone, the functional layer lining sloughs off, and the next menstrual phase begins.
|
|
|
Vagina
|
is a thick-walled, fibromuscular tube that forms the inferior-most region of the female reproductive tract and measures about 10 centimeters in length in an adult female. The vagina connects the uterus with the outside of the body anteroventrally, and functions as the birth canal. It is also a female copulatory organ, as it receives the penis during intercourse. It serves as the passageway for menstruation. The vaginal wall is heavily invested with both blood vessels and lymphatic vessels. The vagina’s relatively thin, distensible wall consists of three tunics: an inner mucosa, a middle muscularis, and an outer adventitia
|

