![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
436 Cards in this Set
- Front
- Back
|
Canadian C-Spine Rule Exclusion Criteria |
Non-trauma GCS < 15 Unstable vital signs Age < 16 Acute paralysis |
|
|
Canadian C-Spine Rules High Risk Factors |
Age > 65 Dangerous mechanism (fall from > 3 feet; Axial load; MVA > 100km) Paraethesia in extremities
IF YES TO ANY OF ABOVE - RADIOGRAPHY
|
|
|
Canadian C-Spine Rules Low Risk Factors |
Simple rear-ended MVA Sitting in ED Ambulatory at any time Delayed onset of neck pain Absence of midline tenderness
IF YES, & CAN ACTIVELY ROTATE NECK 45 deg LEFT & RIGHT - NO RADIOGRAPHY |
|
|
Contraindications to Nasal Intubation |
Absolute: Base of skull # Significant bleeding diathesis
Relative: Anti-platelet agents Reversed anti-coagulated Valvular or CHD Hereditary telangiectasia |
|
|
AFOI Innervation |
CNV: V2 (Greater & lesser palantine) - nasal turbinate & septum V1 (Ethmoid) - Rest of nasal passage Although there is variability CNIX: Posterior 2/3 tongue; pharyngeal epiglottis; soft palate; oropharynx SUPERIOR LARYNGEAL (CNX) Base of tongue; Posterior surface of epiglottis; arytenoids & aryepiglottic fold RLN (CNX) VC & trachea |
|
|
Anticonvulsant Meds Implications |
Enzyme induction: * Phenytoin* Carbemazepine * Barb * Will increase metabolim of vec & roc - so use cis or atracurium * Ketamine * Enflurane - abnormal EEG - esp w hyperventilation |
|
|
Epilepsy suitability for day surgery |
Well controlled i.e.: Seizure free >1 yr Nocturnal seizures only |
|
|
Anaphylactic vs Anaphylactoid |
End point for both - mast cell degranulation Anaphylactic - Type 1 IgE mediated Anaphylactoid - Dose related
|
|
|
Anaphylactic Testing |
TRYPTASE: - In vivo half life 3hrs (histamine 3min); Peak 1hr - 3 samples - 1hr; 4hrs & > 24hrs REFER for TESTING: - Skin testing - IgE - RAST (radio-allergosorbent test) - measuring specific IgE - CAP - fluoro-immunoassay - alternative to RAST - more sensitive than RAST |
|
|
Causes of Life-Threatening Anaphylactic Reactions |
NMBDs (70%) Latex (12%) Colloids (5%) Induction agents (4%) Antibiotics (3%) BDZ (2%) Opioids (2%) Other (2.5%) e.g. Radiocontrast media |
|
|
Allodynia |
Painful response to a normally innocuous stimuli |
|
|
Hyperalgesia |
Increased response to painful stimulus |
|
|
Dysasthesias |
Abnormal sensation |
|
|
Warming Modalities |
Forced air warming Insulating layer Warming OR Circulating water mattress IV fluid warming Humidification of gases Preop warming Radiant heaters |
|
|
Hazards of Prone Position |
AIRWAY CVS - increased afterload; decreased preload; compression of neck veins ETT tie; increased myocardial demand (afterload) NEUROLOGICAL - C spine; Spinal cord (vertebrobasilar); Neuropathies (BP; Peroneal; Ulnar; Sciatic stretch; Fem compression); CVA risk OCULAR - Corneal abrasian; Orbital compression; Venous drainage RESP - Decreased FRC; Abdo compression; Atelectasis M-SK - C spine; Pressure ulcers; Gonads/breast; Face; Lines/monitoring THROMBOEMB MANUAL HANDLING LINES
|
|
|
CI to Beach Chair |
1. Risk of cerebral hypoperfusion: * Severe carotid disease/Increased ICP/ Chronic HTN* Hypovolemia * Autonomic dysfunction 2. Spinal injury 3. Morbidly obese (relative/precaution) |
|
|
Hypothermia - Def & Effects |
Temp < 35 deg
EFFECTs: Shivering - Increased pain; Dystonias; Dicomfort; Inc pain Inc Infections - Resp/surgical wound healing Drugs - Impaired metab & elimin (anaesthetic agents; analgesia; NMBDs) Increased hosp stay & cost CVS - Arrythmias/ Inc HR; Inc SCR/BP; Peripheral perf; IV access; ECG artefact; SpO2 CNS - Delayed wake; Opioid sens; Inc ICP Resp - Central resp depression; L shift ODC (dec unloading) GIT - ischaemia; Imp gut motility Renal - cold diuresis HAem - Imp Plt/clotting factor; Thromboemb risk/stasis (NB Coag tested at 37 deg therefore normal) Endocrine - Stress response - catechol/ Na & H2O retention; Inc BGL |
|
|
Monitoring ANZCA Guidelines |
Clinical - Circulation/Ventilation/Oxygenation
Equipment - Must be in use: * O2 Analyser* Breathing system disconnection or vent failure alarm * Pulse oximeter - tone & alarm * CO2 monitor * VA analysis * ECG - 5 lead option * BP - NIBP (must be) & invasive (should be) available * Temp * NMS * BIS/Entropy * Other indicated monitors e.g. TOE; CO; CVP; EEG
|
|
|
MACE Events? Risk of MACE in Stents for non-cardiac surgery |
MACE = Death; MI; Thrombosis or rpt revascularisation
BMS <30 days - 11% DES < 90 days 6.4%; < 365 days 5.9% |
|
|
RFs for Thrombosis of Stents |
CLINICAL: * Previous stent thrombosis* Age >80 * Prior brachytherapy * Low EF * ACS indication for stent * Renal failure * DM * Left main * Long stents (>18mm) * Small vessels (<3mm) * Suboptimal angio results * Multiple stents/overlapping * Ostial or bifurcation lesions |
|
|
Bridging for Non-cardiac Surgery (stents) |
Consider if high risk for thrombosis: BMS - < 6/52 or > 6/52 w addit RFs DES - <1 yr or >1yr w addit RFs
High risk surgery for bleeding - Intracranial/Spinal/Extraocular/TURP
Option for high risk thrombosis & surgery: * Cont aspirin if possible* Cease clopidogrel 5 days before * Tirofiban & UFH 3 days pre-op - cease 8hrs * D1 post-op - give 300mg clopidogrel * Other - short acting ADP-RA e.g. Ticagrelor - in future
NB Should be done in centre w CCU & PCI capability
|
|
|
Awareness Causes & Risk |
Human factors - miscalculation; omission; programming; inattention Patient factors - Inability to tolerate adequate anaesthesia; Altered PD or PK (obesity; hypermetabolic; other drugs); DI Equipment factors - delivery or monitoring - calibration; malfunction; disconnection
Risk 0.1-0.2% Implicit (unconscious awareness) & Explicit |
|
|
Pre-requisites for coming off CPB |
TRAVEL-CC
Temp - Normothermia (36-37deg) Rate/Rhythm - High-normal (80-90) & SR Acid/Base - Normal pH/pCO2/ HCO3 Ventilation - 100% O2 & expand lung bases Electrolytes - K (4.5-5); Mg; Ca Level table CO - Establish native cardiac output Coag - have protamine ready & do TEG
Main concerns - Inotropy; Coag; Temp |
|
|
Causes AS & natural Hx |
Calcific AS - age 70-90; progresses slowly Calcific Biscuspid (1-2% population); M>F; 40-60yrs RHD & congenital - rare
Pathophys - Sclerosis initally - ~16% progress to AS w/i 7yrs - Eventually LVH leading to diastolic dysfunction w onset of congestive symptoms OR angina (demand > supply) |
|
|
ECHO Aortic Stenosis Features |
Qualitative: - Valve leaflets - AR - Post-stenotic root dilation - RWMA - TR/RV function
Quantitative: - EF - AVA (<1; 1.5; >1.5) - Pressures - gradients; RVSP - Velocity (<3; 3-4: >4) - Diastolic dysfunction |
|
|
Mortality AS |
Asymptomatic <1% / yr 50% mortality if symptomatic, or median survival: Angina 5 yrs Syncope 3 yrs Exertional Dyspnoea 2 yrs
Not linear, therefore exercise used to reveal occult symptoms in younger pts at low surgical risk |
|
|
Aortic Stenosis Anaesthetic considerations |
Maintain SR Avoid brady or tachycardia Maintain SVR/avoid hypotension Optimise IV fluid volume to maintain VR & LV filling |
|
|
Day Surgery Criteria for DC |
Stable vital signs >1hr Correct orientation as appropriate for pt No resp distress/stridor - 4hrs post extubation Pain controlled - with suitable analgesia for DC Minimal N&V, dizziness Adequate hydration & oral intake Minimal bleeding or wound drainage Responsible adult to take home Lines of contact established |
|
|
Day Surgery Suitability |
PROCEDURE SUITABILITY - Airway; Length; Inexperience; Post-op surgical or anaes complications (airway or bleeding); NOT cranial/Tx/Abdo; Pain; Return to diet
PT SUITABILITY - PGA >46weeks; Ability to follow instructions; Place of residence w/i 1hr; ASA 1/2 or medically stable 3/4
SOCIAL REQUIREMENT - Responsible adult to take home; Within 1hr of appropriate medical help; Access to telephone
|
|
|
WHO SS Checklist Objective |
Improved communication & culture of safety
- Correct site surgery - Provision of safe anaesthesia - Management of airway problems - Management of haemorrhage - Avoiding known allergies - Minimising risk of surgical site infection - Preventing retention of swabs - Accurate ID of specimens - Effective COMMUNICATION w/i surgical team - Routine surveillance of surgical outcomes |
|
|
WHO SS checklist Evidence |
Reduced overall mortality 1.5% to 0.8% Complication rate 11 to 7%
|
|
|
WHO Components |
SIGN IN (B4 induction) Pt; Site; Surgery; Consent; Marked; Anaes machine & meds; Allergy; Anaphy; SpO2
TIME OUT (B4 skin incision) Team intro; Pt; Site; Surgery; Incision; Abs; Anticipated critical events; Imaging
SIGN OUT (B4 pt leaves OT) Counts; Specimens; Equipment probs; Name of procedure |
|
|
Consent Steps |
ELEMENTS 1. Must be voluntary 2. Must be competent 3. Provision of information - info sheets not enough alone 4. Documentation 5. Qualified personell & interpreter if needed
WHY NECESSARY - Ethicial (Autonomy) & Medicolegal
|
|
|
Serotonin Syndrome Causative Drugs |
Anti-depressants - SSRIs; SNRIs; TCAs; *MAOIs Opioid & related - Tramadol; Peth; Fent Mood stabilisers - Lithium; Na Valproate Recreational - Amphet; Ecstasy Herbal - St Johns Wort; Ginseng Anti-emetics - Ondansetron; Metoclopr ABs - Linezolid
|
|
|
Serotonin Syndrome - Clinical Signs |
CAN: CNS - Confusion/Agitation; Seizures - Coma ANS - Labile BP & HR; Hyperthermia; Dysrhythmias; Mydriasis; Flushing Neuromuscular (NM) - Rigidity; Hyper-reflexia; Clonus
DIAGNOSIS - of exclusion; Need NM signs & exposure to drug w/i 5 wks Extensive DDx - Drugs; Encephalopathies; Psych; MH; TFT |
|
|
NMS vs Serotonin Syndrome |
NMS - Idiosyncratic reaction after prolonged exposure OR abrupt cessation NMS - Develops over days or wks NMS - Severe muscle rigidity & rhabdo (SS - mydriasis, diarrhoea, hyper-refl, myoclonus) NMS - Freq assoc w MOF |
|
|
Contraindications Sitting Position (Neuro) |
ABSOLUTE: - Patent AV shunt - PFO - RAP > LAP - Cerebral ischaemia when upright & awake RELATIVE: - Extremes of age - Uncontrolled HTN - COPD |
|
|
SITTING POSITION COMPLICATIONS |
VAE Pneumocephalus Macroglossia Quadriplegia PNS - particularly common peroneal; RLN (inc risk w TOE) Spinal injury/SC |
|
|
Block of Fibres with RA - Order |
1. Sympathetic 2. C - Cold (slow pain, T, touch) 3. A delta - Pinprick (fast pain & T) 4. A beta - Touch; Pressure 5. Motor
Usually highest to lowest: Cold - Pinprick - Touch |
|
|
LSCS Blockade - Required levels & organs |
Incision - T12/L1 Peritoneum - T4 Uterus T10 |
|
|
Laryngeal Trauma Signs |
(HaNDSSS) MAJOR: Stridor Inability to lie Supine Subcut emphysema MINOR: Hoarseness Haemoptysis Dysphagia Neck tenderness/swelling
|
|
|
Sizes ETT to fit BB & FOB |
ETT >4.5; EBB 5; FOB <2.8 ETT >6.5; EBB 7; FOB <3.5 |
|
|
Sizes EBB |
French 5 7 9
|
|
|
DLT Sizes |
French (1 Fr = 1/3mm; 3 Fr = 1mm) 28/32/35/37/39/41 Calculating: - Diameter of trachea at clavicles - Ht of pt - Distance at lips NB Size 35F & below - need ped bronch <2.8mm >35F - fits 4.2mm FOB? |
|
|
Cerebral Monitoring |
Intraventricular Drain/Catheter Intraparenchyal Subdural pressure transducers Jugular bulb oximetry - shows effects of interventional therapy; Invasive; global O2 utilisation only Transcranial doppler - differentiate bn vasospasm & hyperaemia Near Infrared Cerebral Spectroscopy
NB ICP Monitoring - only evidence in TBI
|
|
|
DDx Stridor |
FB Infectious: - Epiglottitis - Croup (most common acute) - Bacterial tracheitis - Retropharyngeal or tonsillar abscess Laryngomalacia (most common chronic) Severe bronchospasm VC dysfunction Burns External compression |
|
|
ARDs Def & Diagnostic Criteria |
Def = Syndrome of inc pulm cap permeability & inflammation
Diag Criteria: PaO2 / FiO2 < 200 Bilat infiltrates on CXR PCWP < 18mmHg or no evidence of inc LAP |
|
|
ARDs Management |
1. Adequate Oxygenation (paO2 ~60) 2. Minimise Ventilator Trauma: - Volutrauma - Barotrauma - Biotrauma (infl) - Atelectotrauma PROTECTIVE LUNG STRATEGIES - TV 4-8ml/kg; Plateau P <30; High PEEP (5-24) 3. Prone - severe ARDS NNT = 11 4. Permissive Hypercarbia (deep sedation) 5. NO/PGI2 (no survival benefit); ECMO |
|
|
Contents Epidural Space |
Dural sac Fat Spinal nerves Connective tissue Blood vessels |
|
|
Tx vs Lx Epidural |
Tx VS Lx Distance from posterior epidural border to dural sac: Tx 1.5-3mm Lx ~6mm Ligament flav - thinner & softer Cardioaccel fibres T4 Spinous processes Tx more acute angle |
|
|
Decontamination |
Removal of micro-organisms from contaminated materials or living tissue |
|
|
Disinfection |
Inactivation of non-sporing organisms by thermal or chemical means Requires previous thorough decontamination eg 100deg water for 10min 70% EtOH 10min Doesn't kill a few bacterial spores |
|
|
Sterilisation |
Removes or destroys all forms of microbial life Must be decontaminated first Steam under pressure (autoclave) - most reliable |
|
|
Contraindications to Exercise Stress Test |
ABSOLUTE (pretty much acute cardiac conditions) * Acute MI* Unstable angina * Uncontrolled arrhythmia * Severe AS * Uncontrolled HTN * Severe pulm HTN * Aortic dissection * Acutely unwell * Heart failure |
|
|
Types of Stents DES |
Paclitaxel - anti-proliferative Sirolimus - anti-metabolite |
|
|
PDPH Incidence & untreated % |
Touhy needle puncture - 70% PDPH Untreated - 72% resolve within 7 days - 85% within 6 wks
|
|
|
PDPH Clinical Features |
Typically within 24-48hrs (up to 7days) Bifronto-occipital Neck stiffness Worse on standing Assoc - Diplopia (14%); Tinnitus (10%)
|
|
|
PDPH Treatment |
Intrathecal Catheter: - PDPH 6% (Late removal) (Resite - 90%; 50% late removal) Simple analgesia & rest - may help PHARM: - Steroids - dec intensity - Caffeine - poor evidence - Sumatriptan - nil evidence - Epidural saline - typically transient Blood patch (separate slide) |
|
|
Blood patch - Evidence; Efficacy; Technique & CIs |
EVIDENCE: - Symptomatic HA not relieved >24hrs post puncture (71% failure vs 4% if done >24hr) EFFICACY: - 75% pts - complete relief; 18% incomplete; 7% none TECHNIQUE - 15-25ml; Stop when pn; Lie still 2hrs post; no lifting 1/52 CI: - Normal epid CIs; ?Oncology COMPLICATIONS - Transient back pn (35%); Radicular pn; CN palsy; Meningitis; Seizure
|
|
|
PDPH DDx |
PIH/PET Meningitis Cerebral SOL Cerebral vein thrombosis - usually unilateral motor & sensory loss LLs Migraine ICH/SDH/SAH Muscle tension Caffeine withdrawal |
|
|
Causes of Visual Loss |
Rare - all surgery 0.0008%
CORNEAL ABRASIAN VASCULAR COMPROMISE/INAD O2 - Ischaemic optic neuropathy (most common) - Central Retinal Artery Occlusion (mostly embolic; Ext pressure) or BRAO - Central Retinal Vein Occ (External pressure) - Cortical Blindness (MCA/PCA occip/ICA chiasm)
OTHERS - Acute glaucoma |
|
|
Ischaemic Optic Neuropathy - Types, & prognosis |
Most common cause visual loss peri-op Causes not clearly determined ANTERIOR - to sclera foramen - Non-arteritic & arteritic; Vasculitis POSTERIOR - more often embolic than occlusion AION & POIN - different blood supplies & diff RFs Complete or partial loss Poor prognosis - 50% no improvement
|
|
|
Risks of Intra-op Visual Loss |
PATIENT: - Elderly - Vasc disease - Cardiac RFs SURGERY/ANAES: - Spinal/prone/cardiac - Prolonged - Large blood loss - Fluid administration
|
|
|
Reducing risk of Visual Loss |
PRE-OP - Identifying those at risk INTRA-OP - Maintain IOPerfusion/O2 - Avoid hypotension - Dec transfusion threshold - Minimise IOP - Max venous outflow - Avoid direct pressure - DVT prophy - TEDs; SCDs POST-OP - Screen - As above + clexane |
|
|
Risk Resp Events Paed |
PT - Hx Airway reactivity; Recent URTI (4-6/52); Symptoms (cough/fever/recurrent); Age<1; Premature; Parental smoking; Un-fasted; GORD SURG - ENT; Pneumoperiton; Emerg ANAES - ETT (x10); LMA (x5); Light anaes |
|
|
Buprenorphine Patch PD & PK |
Mixed ag (mu) /antag (kappa) Ceiling effect for resp dep; not analgesia T max 60hrs High PPB High lipid solubility T1/2 5 days Metab - liver to bile (norbupren low activity) |
|
|
Regional General Answer |
CIMPLE-TED CONSENT - Include CIs & risks IV ACCESS MONITORING - O2/NIPB/ECG POSITION LA - dose & type EQUIPMENT - Needle (usually short bevel stimuplex); PNS; USS (linear probe 10-15MHz for most) TECHNIQUE - includes landmarks; anatomy; end point EVALUATION - time DOCUMENTATION |
|
|
Blocks to use Curved USS Probe |
Sciatic sub-gluteal block (3-7MHz) - probe in line with greater trochanter & ischial tuberosity Lumbar plexus block |
|
|
VTE RFs |
SLOMMM-COM-Throm SLOMM (major - RR 5-20): S - Surgery/trauma L - LL probs O - Obstetrics M - Malignancy; Mobility; Misc (previous)
COM (minor - RR 2-4) C - CVS (CHF/CHF) O - OCP/HRT M - Misc - travel/COPD/Neuro disab
Thrombophilias
|
|
|
VTE Prophylaxis (* = quality of evidence) |
GENERAL: **Mobilise; Hydration; High quality surgery MECHANICAL: (not demonstrated to dec death or PE) *TEDs (best w heparin); *SCUDs (method of choice - only if BMI <28) Need to be well sized/fitted; Can be worn intra-op NEURAXIAL - low quality data PHARM: **UFH - Inc risk minor bleeding & HITTS cf LMWH **LMWH - Better than UFH for high risk NEWER - Fondaparinux (synthetic) - same as LMWH - Rivaroxaban (Direct Thr I) - Possibly better but inc bleeding risk |
|
|
PONV Risk Score |
RFs - Female; Non-smoker; Previous PONV; Opioids in PACU Risk: 0 RF - 10% 1 RF - 20% 2 RF - 40% 3 RF - 60% 4 RF - 80% |
|
|
Disproven PONV risks |
BMI Anxiety Migraine NG tube Peri-op fasting
UNCERTAIN: - Neostigmine - ASA - Menstrual cycle |
|
|
Strategies reduce PONV w Evidence |
Level A: - RA - TIVA - induction & main - Avoidance N2O - Avoid post-op opioids (multimodal) - Hydration |
|
|
PONV treatment NNT |
5HT3 = 5 Drop = 5 (prevention) Dex = 4 (prevention & nausea); 7 (vomit) Anti-chol = 6 Propofol = 5 (temp) Midaz - 2mg 30 b4 end better than premed (as effective as ondans)
|
|
|
PONV Risk Children |
RFs: Surgery > 30min Age > 3yrs Strabismus Hx PONV or PONV in relatives
Risk: 1 RF = 10% 2 = 30% 3 = 50% 4 = 70%
|
|
|
Obstetric Palsies |
~1% Incidence SPINAL - Rare; Traumatic; Chemical; Ischaemic; Infective LUMBOSACRAL TRUNK - w/i pelvis by foetal head - Foot drop (unilat 75%); 76% recover completely PERIPHERAL: LFCN - most common; Self-limiting; RFs - DM; Hip F/Abd/ER; Obesity FN - Compression ing lig; RFs - Hip F/ER/Abd ON - 25% B/L; Usually w FN; Compress fetal head - pelvis or forceps CP - Disting from LS injury w nerve conduction; Knee hyperflex |
|
|
Differentiation Obstetric Palsy vs Central Lesion |
CENTRAL - Commonly assoc w back or leg PAIN - Bilateral (unusual for periph but possible) - Deteriorating S&S or onset after symptom-free interval - Fever & WCC suggests infection
|
|
|
Red Flags Post Neuraxial |
Acute onset back pain Radicular leg pain Urinary & anal dysfunction LL numbness & weakness
Permanent injury b/n 6-12hrs post symptom onset |
|
|
VAE Detection Sn |
Most to least Sn: TOE Praecordial Doppler PAP - start to get minor clinical signs (HR; BP) EtCO2 Echo - Signif clinical signs (CVS collapse) Oesophageal stethoscope ("Millwheel")
|
|
|
Prevention VAE in Sitting |
1. Positive Venous Pressure - Positioning - Normovolemia - Venodilation - PEEP (controversial) - Jug vein compression (times of high risk) 2. SURGICAL TECHNIQUE - Bone wax; Saline gauzes - Communication high risk periods - Fastidious haemostasis - Dec time 3. EARLY RECOGNITION - Bubbling at site - EtCO2 |
|
|
Signs VAE |
CLINICAL: - Desat - Sudden drop EtCO2 - HR - inc or arrhythmia - Inc ETN2 - Inc CVP/neck vein distension Remember can also be from IV lines |
|
|
Anatomy Larynx (C spine levels) |
Hyoid C3 Superior horn of thryoid cartilage C4 Cricoid C6 |
|
|
C450 Inducers & Inhibitors |
INHIBITORS SSRIs/St Johns Wort* Buprenorphine* Cimetidine/Ranitidine* Metoclopramide*
INDUCERS Dexamethasone * Rifampicin* Anticonvulsants
* = 2D6 |
|
|
Autonomic Neuropathy Incidence, CVS S&S |
Incidence 1 in 10 DM (all types) (40% DM1)
- Resting tachy (90-130) - Exercise intolerance - Loss of HR variability (normal >15 w deep breathing - AN likely when <10; Abn Valsalva) - Orthostatic hypotension (SBP >30; DBP >10) - Silent MI - QT abnormalities 2 Abnormal tests for Dx (most Sn - HR response to standing/valsalva/deep breathing) - Assoc w greater haem changes intra-op
|
|
|
Autonomic Neuropathy S&S GIT & Other |
- Gastroparesis (GORD; Early satiety; Nausea) - Constipation, alternating w diarrhoea (often nocturnal)
OTHER - Absence of sweating/perfuse gustatory sweating; Dec recognition of hypo; Urinary retention; Poor temp regulation; Impotence |
|
|
Effects of Hypothermia |
CVS - Vasoconstrict/SNS; <28 arrhythmias; AMI RESP - L shift ODC CNS - Confusion <34; LOC <32; Slow wake; Dec O2 5%/degree NM - Shivering - O2 demand & monitoring artefact; Dec metab NMBDs IMMUN - Impaired wound healing; Neutr HAEM - Plt & factor dysfunction BEHAVIOURAL
|
|
|
SC Blood Supply |
ASA - Anterior 2/3 of cord - Arises foramen M junction of vert @ 2 x PSA - From PICA Anastamoses b/n ASA & PSA.
Reinforced by radicular @, branches from: * ascending cervical artery* deep cervical artery * intercostal arteries * lumbar arteries * sacral arteries * |
|
|
SC RFs ischaemia & Prevention |
SCPP = MAP - CSFP Autoreg 45-180 Time >30-45min RFs - Distal aortic hypoperfusion - Peri-op hypotension - Hypoxemia PREVENTION 1. MAP/O2/Time 2. CSF drain - best w option 3 (set overflow 10 & cont post-op) 3. Distal aortic perfusion - only works if @ Adam below clamp 4. Surgical implantation critical intercostal @ 5. Hypothermia - local (epidural) or systemic |
|
|
Reasons not to do AFOI/Possible Probs/CIs |
* Patient refusal
* Bleeding in airway * Distressed patient/impending obstruction * Friable tumour * Stridulous - may completely obstruct with Bronch * Lack of airway skills * Allergy to LA * Severe coagulopathy * Fractured BOS (CI to nasal route)
|
|
|
Paediatric Dehydration Estimation (RCH) |
MODERATE DEHYDRATION (4-6%) - Delayed Central CRT (>2sec) - Inc RR - Mild Dec turgor SEVERE (>7%) - CRT >3sec; Mottled skin - Other signs of shock - Inc HR; irritable or Dec LOC - Deep, acidotic breathing - Dec turgor
UO (Mild/mod/sev) <2/<1/<0.5 |
|
|
Indications OLV |
ABSOLUTE: 2. Control of ventilation - BP fistula - Giant cyst or bullae - Major bronchial disruption or trauma - Unilat Tx 3. Surgical Access - VAT
RELATIVE: - Surgical access - Lobectomy/pneum - Other thoracic surgery - Oesoph; Vertebral |
|
|
Relative CIs OLV |
Paediatric - won't tolerate Tumour in lower trachea Critically O2 dependent |
|
|
Differential Blood flow - normal lung & OLV |
NORMAL: (R) 55% (L) 45%
OLV: Non-dependent 77.5% Dependent 22.5% |
|
|
Hypoxia on OLV Steps |
1. Check oximetry/trace/scan monitors 2. Increase FiO2 3. Check circuit/ventilator 4. Auscultate 5. Suction dependent lung & tube patency 6. Check tube position 7. Apply CPAP or entrain O2 to NVL 8. Perform recruitment man. or PEEP 9. Revert 2 lung 10. Clamp PA to NVL
(OO Circuit Listen Scan Suction Tube CPAP PEEP 2lung Clamp) |
|
|
General Approach to Any Complication |
ABC - Immediate medical care RV notes/event Sorry - open communication Debrief Consults Documentation Medical indemnity & hospital medico-legal authority Audit M&M
|
|
|
P COPE PRIME TIME RAW |
P - Pt; Procedure; PMHx C - Consults (inc Hx/Ex/Ix) O - Optimisation P - Premed E - Explain & consent P - Position; Prep; Plan; Pt safety R - Resusc I - IV access & fluids M - Monitoring E - Equipment T - TF (MADE) I - Induction - plan, drugs, airway M - Maintenance E - Emergence
PACU R - Recovery handover A - Analgesia W - Ward
|
|
|
CEA: 1. Indications? 2. Peri-op Mortality & Stroke risk? |
INDICATIONS: - Symptomatic pts with moderate to severe stenosis - Definite benefit in high grade (70-99% st) - NNT = 6 - Less marked benefit in sten 50-69% - Recommendation - with 2/52 of symptoms; <48hr is best (NICE guidelines)
PERI-OP MORT & STROKE RISK 2-5% Peri-op MI 2% (IHD common) |
|
|
Perceived Advantages of LA for CEA |
- Gold standard cerebral Fx - Lower shunt insertion - Improved haemodynamic stability - Earlier detection & Rx of complications - Intact cerebral autoregulation - Lower re-exploration rate - Less post-op anxiety for surgeon & anaes - Less post-op pain - Useful for pts whom GA is undesirable (a/w CABG) - Shorter stay
DISAD: - Conversion rate 1-3% - Airway & ventilation control - VA - cerebral protection - Claustrophobia - Phrenic nerve |
|
|
GALA Trial |
GA vs LA for CEA: - No difference (non-significant trend towards fewer operative deaths) - LA assoc with less shunts |
|
|
Monitoring Cerebral Function during CEA |
ICA stump pressure (want mean >50-60) EEG - cortical only not deep SSEP - Can detect subcortical ischaemia Transcranial Doppler - MCA flow - can detect emboli Jugular VO2 Near infrared spectroscopy |
|
|
Tourniquet Complications |
LOCAL EFFECTS: MUSCLE - Inflation - anaerobic metab (necrosis >2hr) - Deflation - 'Post-tourn syndrome' - swollen, pale, stiff limb - 1-6/52 NERVE 1. Physiological block - ischaemia 2. Direct compression - large nerves more susceptible - up to 6/12 CVS - Plaque rupture w exanguination - Inc CVP & SVR (CCF) - 400ml/leg - Deflation - hypotension TOURNIQUET PN - Unmyelinated slow C fibres |
|
|
Tourniquet Times, Size & Pressure |
PRESSURE (mmHg): - Fixed - 250 for UL & 300 LL - OR SBP + 100 (UL) & 150 (LL) SIZE: - >40% diameter of thigh TIMES: 1.5-2hr (muscle ATP depleted) Temp deflation - at least 10 min (ATP restored) |
|
|
CI Tourniquet |
DVT Severe crush injury Severe OP Sickle cell disease PVD Coagulopathy Cellulitis |
|
|
Obesity Systems Effects |
RESP - Dec FRC - Possible DI (correlates with OSA & neck circ) - Pulm HTN - Obesity hypoventilation syndrome CVS - HTN - systemic & pulm - Inc risk arrhythmias due to hypertrophy; hypoxemia; inc catechol & fatty conductive - DVT risk ASSOC DISEASES: - GORD - DM OTHER - PK; IV access & monitoring |
|
|
What is Obesity Hypoventilation syndrome? |
Diurnal variation in ventilation & inc PaCO2 CO2 sens & resp drive - partly under control of leptin (satiety hormone) Relative leptin insens in obesity - Dec vent response to inc PaCO2 THEREFORE - Avoid premeds w resp depressants; Opioid sparing techniques |
|
|
What is Metabolic Syndrome |
Cluster of RFs comprising: - Excess abdominal weight - Lipid abnormalities - HTN - Elevated glucose levels |
|
|
Anaemia Effects |
CVS: - Dec viscosity -> dec resistance -> Inc preload & dec -> Inc CO - Inc HR & /or contractility - minor role - Inc O2 ER - Redistribution of blood flow to areas of high demand (myocardium & brain) - Inc 2,3-DPG -> (R) shift ODC (chronic) RESP - Tachypnoea to Inc O2 - Dyspnoea ENDO - Inc EPO IMMUN - Impaired wound healing
|
|
|
Anaemia Classification |
NORMOCYTIC (MCV 80-100) - Anaemia of chronic disease (absent reticulocytes; low transferrin, iron & %sat) - Haemolysis (reticulocytes; high LDH; mildly inc bilirubin)
MICROCYTIC (MCV <80) - Iron def (hypochromic; high transferrin) - Chronic disease - Thalassemia
MACROCYTIC (MCV >100) - Acute blood loss - Haemolysis - Megaloblastic - Drugs (alcohol; MTXl Azathioprine; phenytoin)
|
|
|
SAH - WFNS Grades
|
GCS & Motor Deficit (+/-) Grades I - V I - 15 (-) II - 13-14 (-) III - 13-14 (+) IV - 7-12 (+/-) V - 3-6 (+/-) So basically only care about motor deficit to differentiate b/n grades II & III |
|
|
SAH - HUNT & HESS Grades |
Based on clinical presentation - more detail than WFNS (i.e asymptomatic; HA; nuchal rigidity; CN palsy; Drowsy; Hemiparesis; rigidity & coma)
Gives mortality: Ranges from 0-2%; 5-10% (Grades II & III) to 50% (V) |
|
|
Complications SAH |
1. RE-BLEED: - Untreated - 15% 1st 24/24; 30% 1/12; ~3%/yr 2. DCI (VASOSPASM) - Major cause delayed M&M - Peaks 4-14 days 3. HYDROCEPHALUS (15-20%) 4. CARDIAC DYSFUNCTION (b/c catechol release) 5. Dec Na & Mg 6. Epilepsy/Seizures 7. Neurogenic Pulm Oedema |
|
|
Remote Anaesthesia |
- Remote location - Risks of unfamiliarity w location - drugs / equipment; Unstocked - Unfamiliar staff - Access to DI trolley - Other colleagues further away if emergency - Poor lighting - Difficult access to pt |
|
|
Factors affecting IOP |
- Tone extraocular muscles (sux ?signif) - Venous drainage - head position; neck ties - MAP & CVP - pressor response; induction - LA volumes in orbit (transient) - External compression - Drugs - Mannitol (vitreous fluid); Azetazolamide (dec ciliary body aqueous production) - Hypocapnia - vasoconstriction choroidal vessels (26-30) |
|
|
Pre-op Ophthalmic Surgery |
Most day cases; LA; on elderly pts with > 1 serious systemic disease - Axial length (<25mm) - INR/APTT - BGL if DM - Ability to lie flat 1hr (cough; OSA; arthritis; CCF) - Hearing/comprehension |
|
|
Innervation Eye |
Muscles - All CN3 EXCEPT SO (IV) & LR (VI
Sensation (inc ciliary gang) - CNV (V1 & V2)
CILIARY GANGLION: PNS - CN III SNS - Carotid plexus
|
|
|
Peribulbar block complications |
- Globe perf (0.01%) - Inc IOP (Use Honan balloon) - Retrobulbar injection (upper eyelid should not fall) - Muscular injection - Retrobulbar haemorrhage (0.07%) - Systemic - oculocardiac R; neurogenic syncope (monitoring essential) - Infection - Dural injection (use short needle 25mm) |
|
|
Subtenon's Space - anaesthesia, akinesia & visual blockade mechanism |
OR Episcleral space = Potential space ANAES - from blockade of short ciliary nerves (V1) as they traverse the space VISUAL BLOCKADE - direct flow of LA into dura invaginating CNII posteriorly AKINESIA - Direct flow of LA into muscle sheaths |
|
|
PROS & CONS Subtenon Block |
- Greater akinesia than topical or subconj LA - Rapid onset - Good & reliable akinesia (?5-15min) - Less pn (cf retro & peribulbar) - No sharp needle (globe perf; SA injection; Intraneural) - Don't need to cease anticoag (bleeding pts can be cauterised directly) - Can use in myopic pts (>26mm) - Can perform block in any of 4 quadrants
CONS - Special equipment; Skill; More invasive than topical; Chemosis; Subconjunctival harm (30%) - Relatively CI inferonasal pterygium -> red eye & poor cosmetic result - CI Scleral disease & previous vitrectomy (spread) |
|
|
WHY INFERONASAL QUADRANT FOR SUBTENONS? |
- Lack of insertion of extra ocular muscles - Surgeons tend not to use this approach (can't get into coronial plane b/c of nose) |
|
|
Equipment Classification for Cleaning |
CRITICAL - will penetrate skin or MM - require sterilisation SEMI-CRITICAL - will be in contact with intact MM or may become contaminated with readily transmissible organisms - high level disinfection or sterilisation NON-CRITICAL - Contacts intact skin or doesn't contact pt directly - low level disinfection or cleaning
NB Everything should be decontaminated 1st |
|
|
Levels of Checks |
LEVEL I - after servicing or new machine LEVEL II - Before list - High pressure (pipeline) & low pressure (flow & anti-hypoxia) - Breathing systems (leaks/valves) - Automatic Ventilator - VA (level/scavenging/leak/back bar) - Other (suction/Emergency/O2 cylinder/Laryng blades) - IV & LA delivery systems END - Documentation LEVEL III - If circuit change - leak test - Suction/Intub/Humid/Filters/Gas analysis/ Monitors |
|
|
MH DDx & Supporting factors |
- Awareness - Rebreathing - Sepsis - NMS - Ecstasy - Thyroid storm
Supporting MH - Sustained jaw rigidity; Generalised rigidity; Core T Inc of 2 deg/hr |
|
|
Dantrolene Dose |
2.5mg/kg Boluses Q10-15 min Up to 10mg/kg or more
NB Each vial is 20mg |
|
|
Axillary block - Subcutaneous Nerves |
Medial Brachial Cutaneous Medial Antebrachial Cutaneous Intercostobrachial |
|
|
Effects Pneumoperitoneum 1. IAP 2. CO2 |
CVS - 10-20 - initally auto transfusion of splanchnic circa -> Inc VR & CO - Then -> Dec VR & CO; Inc SVR; HR Inc or same (SNS - CO2 & Pain) - Inc myocardial work, may ......-> Ischaemia - IAP >20 -> Dec VR & CO +++ (If Vagal w rapid insuffl -> brady) RESP - Dec lung volumes & compliance - Inc V/Q mismatch - Inc risk barotrauma RENAL >15 -> Oliguria >20 -> Anuria
2. CO2 Load (Resp/CVS/CNS/ODC) |
|
|
Trauma Induced Coagulopathy Definition & Characteristics |
Def - Imbalance of the dynamic equilibrium b/n procoagulant factors, anticoag factors, plts, endothelium & fibrinolysus CHARACTERISTICS: - Factor V Inhibition - Systemic Anticoagulation (APC -> breaks down Va & Viiia; Antirepression of fibrinolysis) - Hyperfibrinolysis (Rx TXA) - Plt dysfunction
|
|
|
Trauma Coag Abnormalities Lab Results |
- Anaemia - Thrombocytopenia (Plt dysfunction difficult to test) - Inc aPTT & PT ( APC breaks down fa & 8a - essential cofactors in both pathways) - Low fibrinogen (aPC -> dec plasminogen activator inhibitor -> Inc plasmin -> fibrinolysis) - Inc D-dimers - TEG & ROTEM changes - may take 30-60min |
|
|
Mx Trauma Coagulopathy |
PRE-HOSP: - TXA (<3hrs) - Crystalloids <3L - Prepare products (ring ahead) HOSPITAL: - Early activation MTP 1:1:1 - Prevent & treat hypothermia & pH (33 & 7.2) - TEG to guide - Level 3 evidence - Optimal CO - Ca2+ if hypocalcemic - Factor VII - non-surgical bleeding & all correctables corrected
|
|
|
TEG result & Products |
Inc R time -> FFP (>10) Dec alpha angle -> cryo (<53 - rate of clot formation) Dec MA -> Plts (consider ddAVP) (<50) Inc LY30 = fibrinolysis -> TXA (%Dec in amplitude after 30 min)
|
|
|
AFE Risk Factors |
- Inc maternal age (>25) - Multiparity - IUFD - Maternal Hx of atopy/allergy - Chorio - Polyhydramnios - Microsomia - Strong or tetanic uterine contractions - Placenta accreta - Augmented labour |
|
|
AFE Clinical Features |
1. MATERNAL COLLAPSE (Consider other DDx) 2. RESP - APO (>90%); Dyspnoea; Cough; Bspasm 3. CVS - Arrest (>90%); HypoBP; Arrhythmia; RV ->LV failure; Cyanosis; CP 4. NEURO - HA; Seizures 5. OTHER - Foetal distress (100%); DIC; Uterine atonyA |
|
|
Anatomy Bronch - Levels of cricoid & carina (i.e. length of trachea) - Length & angles of main bronchi - Directions of lobar bronchi |
Tracheal Length (10-15cm): Cricoid C6 Carina T5 RMB - 25 deg; 2.5cm to RUL bronchus LMB - 45 deg; 5cm to LUL bronchus RIGHT ULB - 0300 MLB - 1200 LLB - 0600 LEFT ULB - 0900 LLB - 0600
|
|
|
Lung Segments (Bronchopulmonary) |
Right lung = 10 Left lung = 8 |
|
|
Obstruction post thyroidectomy - DDx |
SURGICAL: - Haematoma - RLNP - Tracheomalacia - Hypocalcemia (unlikely early) - PTX - Oedema ANAES: - Residual NMBD - Drug error - Over-sedation/opioids PT: - Anaphylaxis - Pre-existing CVS or resp disease - Developing resp disease (atelectasis; aspiration) - MI - Anxiety |
|
|
Opioid Oral Morphine Equivalents (OME) |
IV morphine 1mg = 3mg OME Fentanyl (transdermal or IV) 12mcg = 30mg Tramadol 5mg = 1mg OME Oxycodone 1mg = 1.5mg OME Codeine 10mg = 1mg OME |
|
|
Variable Bypass Vaporiser Safety |
1. AGENT SPECIFIC (Colour; Key indexed fill) 2. Interlock device 3. Pressure resistance/anti-pumping 4. Locking spindle (& o-rings to prevent gas leakage from back bar) 5. Anti-tilt measures, visible agent level 6. Automatically compensate for changes in ambientpressure 7. One-way check valve b/n vaporiser & O2 flush valve |
|
|
TAP Spinal nerve Levels |
T6-L1 |
|
|
Pre-Eclampsia - Definition & Criteria |
= HTN occurring after 20/40 & resolving within 3/12 of delivery w:
SBP >140 or DBP >90 PLUS at least 1 of: - Proteinuria (0.3g/day) - Renal impairment (inc pr & cr) - Liver disease - pn; inc transam - Neuro probs - seizures; visual disturbance; papilloedema - Haem disturbance - Plt; Haemolysis; DIC - Foetal growth restriction |
|
|
PET Risk Factors |
- PET Hx - Inc maternal age - Multiple pregnancy - High BMI - CT disorders - Protein C & S Deficiencies - Factor V Leiden - Hyperhomocysteine
|
|
|
Peribulbar Insertion Point |
Inferior orbital rim - junction of zygoma & maxilla - Insertion point is 1mm above rim & just lateral to this |
|
|
Peribulbar Block Complications |
- Globe perforation (<0.01%) - Inc IOP (Honan balloon) - Retrobulbar injection (stop if upper eyelid falls) - Muscular injection - Retrobulbar haem (0.07%) - Systemic complications (OG reflex; Syncope) - Endophthalmitis - Dural injection (use short needle) Don't insert >15mm |
|
|
Vasospasm Mx |
- GENERAL MEASURES (airway; T; O2; CO2) - SURGICAL - Optimise CPP - Triple H - no evidence; ?HTN alone - Nimodipine - Level 1 evidence 60mg Q4H - No evidence - Mg; Statins - Clazosentan - small RCT (endothelia antag) - RADIOLOGICAL (angioplasty; papaverine - refractory; |
|
|
Metabolic Syndrome Diagnostic Criteria |
Elevated waist circumference (population specific) Elevated triglyceride levels Reduced HDL-C Elevated BP (>130/85) - Elevated fasting glucose (>5.5) |
|
|
Dabigatran & Rivaroxaban MOA & Indications |
Dabigatran = Oral direct thrombin inhibitor (Pradaxa)
TGA Approved Indications: - Prevention of VTE post major ortho surgery LL (PBS) - Non-valvular AF & at least one additional RF for CVA (Non-PBS)
Rivaroxaban = oral factor Xa inhibitor Indications - as above + treatment & prevention of recurrent VTE
|
|
|
Dabigatran Guidelines if bleeding |
- Optimise renal function - Check for drug interactions - Check FBC, U&E, Ca, APTT, TT & fibrinogen MOD BLEEDING: - Fluids to maintain UO - If Plt <80 or on anti-plt - consider Plts - Charcoal if <2hrs SEVERE BLEEDING: - As above PLUS - consider TXA - If critical - consider Recombinant FVIIa (50mcg/kg) - note short T1/2 - Dialysis - may remove 60% |
|
|
Dabigatran pre-op cessation & RA |
High bleeding risk (cardiac; spinal; neuro; abdo) - stop for 5 days
Low bleeding risk - eGFR > 50 - 2 days - eGFR > 30 - at least 3 days - <30 - 5 days & don't restart
Neauraxial - CI unless normal TT; & 24hrs post removal of catheter |
|
|
Fat Embolism Clinical Features |
Either fulminant or gradual Typically - 1F2-36hr post injury RESP - Inc PA pressures - Hypoxia.... Resp failure CUTANEOUS - Petechial rash (50-60%) - Upper half body/MMs/conjunct NEURO - Drowsiness/Coma/Seizures - Global dysfunction
MINOR SIGNS - HTN; Fever; Tachy; Oliguria; Jaundice; Retinal petechiae |
|
|
Fat Embolism Prognosis & RFs |
10-44% require ventilation Pulm - resolves 3-7 days Mortality 1-20% RFs: - Delayed ORIF (LLs > ULs) - Intramedullary fixation - Bone marrow necrosis; Sickle cell crisis; Acute pancreatitis
|
|
|
Hyponatraemia Causes |
HYPOVOLEMIC: - Renal H2O loss - CSW; Salt-losing nephro; Addisons - 3rd space - pancreatitis; burns; cirrhosis - Sweating/D&V - normal H2O intake EUVOLEMIC: - SIADH (drugs; malignancy; CNS) - Polydipsia; Amphet HYPERVOLEMIA: - Cirrhosis; CCF - Hypothyroidism - Renal failureH - Nephrotic syndrome PSEUDO: - When there is an osmolar gap (BGL; Glycine; proteins; lipids) |
|
|
Hyponatraemia Ix |
For hypo or hypervolemia: - Urinary Na to differentiate causes For Euvolemia: - Urine vs serum osm (SIADH Urine>Serum; all other causes opposite) |
|
|
Placenta Praevia: - Chance of Accreta - Risk of caesar-hysterectomy if accreta/percreta |
PP w: 1 previous LSCS - 30% 2 previous LSCS - 50% Risk hysterectomy: Accreta - 66% Percreta - 95% |
|
|
APGAR |
Out of 10 (0/1/2) APPEARANCE - Blue / Blue extremities / Pink PULSE - None / <100 / >100 GRIMACE - None / Feeble / Cry, pulls away ACTIVITY - Floppy / Some flexion / Flex & ext RESP - Apnoiec / Weak, irreg / Strong cry
Normal >7 Fairly low 4-6 Critical <4 |
|
|
NEONATAL RESUSC |
1. Ax - APGAR; Estimate gestation & ?meconium
2. If HR <100 / not breathing or crying -> ventilate (5 inflation breaths; then RR 40-60; 30cmH2O)
3. If HR < 60 OR not improving after ventilating for 30 seconds -> start CPR 3:1 every 2 sec & consider intubation
4. VENOUS ACCESS - adrenaline & fluid bolus 5. CHECK BGL 6. VT/VF - 4J/kg shock/2 min - Consider amiodarone; Atropine
Possible causes - PTX; Congenital heart or lung prob; APH |
|
|
Hazards of Laser |
1. Airway fire (Ignition) 2. Hypoxia (inadequate ventilation or distal debris/smoke/secretions) 3. Laser plume (PVR/ciliary/aerosolisation) 4. Soft tissue burns - pt or staff - cutaneous or adjacent to surgery 5. Eye damage (retina) - patient & staff 6. Gas embolism (gas coolant in Nd:YAG)
|
|
|
Laser - Minimising Hazards |
PATIENT: - Eye protection - Protect surrounding tissue - Laser compatible airway (tube or tubeless) - Minimise combustible gas (FiO2<0.4; N2O) - Flame resistant surgical drapes - Matte surgical instruments - Scavenge plume - Avoid plastic tape (combustible) STAFF: - Education/accreditation - Laser officer/protocol/signs & light on OT door - PPE - goggle/masks - Availability of non-water extinguisher |
|
|
Problems with Laser Tubes |
- Narrow ID as have thick outer walls -> difficult SV & higher airway pressures |
|
|
Airway Fire |
1. Disconnect O2 source Switch off LASER & flood site with saline If feasible remove tube Ventilate with air (BMV) w filter (smoke) Ensure keep anaesthetic going (TIVA) - if using VA CO2 extinguisher After fire extinguished - look with rigid bronch Arrange HDU/ICU If fire continues- follow local hospital protocol |
|
|
What does LASER stand for? |
Light Amplified Stimulated Emission of REadiation |
|
|
Effect of Magnet on PMs & AICDs |
PMs - Asynchronous (fixed rate) AICD - Disables anti-tachycardia function ICD+PM - Only disables AICD |
|
|
Peri-op plan PMs/AICDs & EMI |
EMI likely? - Switch of anti-tachycardia fx - Use bipolar - If mono polar - short bursts or low energy - Plate placed so current not within 15cm of heart - Does PM need programming to asynchronous mode (PM dependent & EMI close to PM) or disabling of special algorithms? - Disable AICD fx |
|
|
SAH Grading |
* WFNS - GCS & Motor (vasospasm)
* Fisher - CT - prognostic for vasospasm * Hunt & Hess - Clinical; Ranges from asymptomatic - mild-mod HA - Deep coma & decerebrate - Mortality prognosis (Grade 0 = 1-2%; Grade 3 - 5-10%; Grade 5 - 50%) |
|
|
Rate of re-bleed SAH (untreated) |
24/24 15% 1 month 30% 3%/yr thereafterS |
|
|
SAH Complications |
* Rebleed
* DCI/vasospasm * Hydrocephalus/ICP (15-20%) * Catecholamin - ECG STE & Echo.....->failure * Hyponatraemia (CSW/SIADH) * Hypomagnesemia * Seizures |
|
|
ECG changes SAH |
ST changes Inc QT TWI U waves |
|
|
Nimodipine dose, duration, SEs & mortality benefit |
* Oral 60mg Q4H
* IV Infusion 0.5mg/kg/min * Start as soon as Dx, for 21 days * Overal mortality RRR 40% * SEs - Hypotension; Nausea; HA |
|
|
Vasospasm & DCI Definition, RFs & incidence |
Incidence 60% SAH (leading cause of M&M) DCI = Neuro deterioration related to ischaemia. Lasts >1hr & has no other cause Vasospasm = Arterial narrowing demonstrated angiographically on doppler US, w corresponding S&S RFs: * Poor grade SAH* IVH * Fisher grade (high SA blood load) * Smokers |
|
|
Classification TBI |
Mild / Mod / Severe (GCS) 13-15 / 9-13 / <9 |
|
|
Normal ICP? |
5-15mmHg |
|
|
Hyperosmolar therapy for ICP? Limits |
Mannitol 0.25-1g/kg (5ml/kg of 20%) (Osm < ?320) - renal damage
3% saline 5ml/kg (Na <155)
OR 20ml of 20% |
|
|
DI Diagnosis |
UO >50ml/kg/day OR >3L/day
High serum osm (>305) & Na (>145)
With abnormally low urine ism (paired)
ADH level
Desmopressin test - will work for neurogenic (= >50% increase in urine osm) MRI - for cause |
|
|
Risks of SC damage intra-op & Risk minimisation |
* Length & type of surgical procedure
* Spinal cord perfusion pressure (= MAP-CSFP) * Underlying spinal pathology * Pressure on neural tissue during surgery * Careful positioning * Aortic surgery - distal perfusion or implantation * CSF drain * Maintain MAP * Methylpred w/i 8hrs post insult * NMDA antagonists? * Prevention of haematoma (haemostasis; drugs)M
|
|
|
Monitoring SC function |
'Wake-up' test SEPs * Record cortical (SCEP) or spinal (SSEP)* Resulting trace analysed for wave amplitude & latency w respect to a reference 'time zero' * Affected by anaes agents; opioids & LA BUT decrease in 35-50% thought to be significant * Recorded from electrodes in epi space * Affected less by VA than MEP * Sensitive to T & LAs * Stimulate motor cortex & elicit response in - distal SC; muscle or nerve * More difficult to achieve & sensitive to VA
|
|
|
VAE Monitor Order of Sensitivity |
1. TOE 2. Praecordial doppler 3. PAP/Minor HR & BP 4. ETCO2 5. ETN2 6. RAP - Significant haemodynamic 7. Echo - CVS collapse |
|
|
Cushings Anaesthetic Implications |
CVS - HTN ......-> LVH ; ECG (TWI; high voltage) - reverts once corrected RESP - OSA/obesity; Myopathies (weaning) AIRWAY - OSA; GORD METABOLIC - Electrolytes & DM OTHER - Often obese w difficult access
|
|
|
Types of Adrenal Insufficiency |
PRIMARY (Addisons) -> Dec glucocorticoids; mineral; androgen Causes - Auto-immune; Infection; AIDS; Mets SECONDARY - Failure of CRH (hypoth) or ACTH (pit) or suppression ->glucocorticoid deficiency only Causes - Iatrogenic (pit surgery; glucocorticoids) S&S - Cut & mucosal pigmentation - primary only - Weakness/fatigue/anorexia/N&V/abdo pn - Myalgia/jt pn - Hypovolemia - Dec Na & BGL; Inc K
|
|
|
What is synacten |
Synthetic ACTH Tests whole HPA axis |
|
|
Treatment Addisons |
Hydrocort 20mg mane, 10mg nocte Fludrocortisone 0.1mg (replace aldosterone) |
|
|
Addison's Crisis |
Causes - Stress in chronic insufficiency w/o replacement S&S - Hypovolemia; Dec Na & BGL; Inc K & Ca Mx - 100% O2 - IV fluids - colloids; NS & glucose - Hydrocort 200mg stat; 100mg tds - Inotropes & vasopressors |
|
|
Steroid Replacement |
All meds up to morning of surgery Hydrocortisone 25mg IV at induction, then: - Minor surgery - nothing required (e.g. hernia) - Intermediate - 25mg Q6H IV for 24/24 - Major - 25mg Q6H for 48-72/24
|
|
|
Brain Death Definition & 3 essential findings |
Def = Irreversible loss of all function of brain 3 essential findings: 1. Coma (unresponsiveness)2. Absence of brainstem reflexes 3. Apnoea |
|
|
Brain death Preconditions |
1. Cause for coma consistent with brain death
2. At least 4/24 of observation during which preconditions must be met (GCS 3 / PUORL/ apnoea/no cough) 3. Neuroimaging consistent w acute brain pathology 4. Normothermia (>35) 5. Normotension (MAP >60) 6. No sedation or analgesia 7. Absence of severe electrolyte, metabolic or endocrine disturbances 8. No paralysis 9. Ability to Ax brainstem reflexes (at least 1 eye & 1 ear) 10. Ability to perform apnoea test |
|
|
Brain death Testing |
Independent examination by 2 suitable trained & experienced doctors (can't be transplant team)
Test (CN) 1. TOF nerve stimulation2. GCS 3 3. Pupils F&D (2&3) 4. No corneal reflex (5&7) 5. No oculo-vestibular reflexes (3,4,6&8) 6. No gag (9&10) 7. No cough on suction (10) 8. Positive apnoea test - after pre-O2 (paCO2>60)
|
|
|
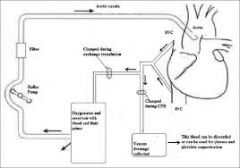
Bypass Circuit |
|
|
|
ICP trace |
|
|
|
Hypothermia effect on metabolic rate |
Decrease 7% for every degree drop |
|
|
ASA & mortality |
Originally used to Ax pre-op status of pts Studies have shown a correlation between ASA & post-op adverse outcomes
Mortality Data 1 - 0.05% 2 - 0.4% 3. 4.5% 4. 25% 5. 50% |
|
|
What affects thermodilution accuracy from PAC? |
* Cardiac shunt
* TR & MR * Variation in T from other sources * IPPV |
|
|
PAC waveform |
|
|
|
Cardiac Index Formula & Normal Values |
= SV x HR / BSA
Normal range 2.5-4.2L/min/m2 |
|
|
CEA Indications & Timing |
>70% stenosis (NNT = 6) Maybe - >50% w low surgical risk (M&M <3%)
TIMING NICE guidelines - Within 2 weeks of TIA/CVA, & <48hrs if possible
|
|
|
Rheumatoid Arthritis - Who to Xray C spine |
Flexion/extension views in: - Pts with UL neurological symptoms or signs - Those with persistent neck pain - particularly radiating to occiput - role of X-ray is controversial & interpretation is difficult (should be senior radiologist) MRI/CT to assess cord compression
Unless certain that C-spine is stable - treat all RA pts as if they might have an unstable spine |
|
|
Atlanto-axial subluxation - Types & incidence |
Order from most common to least: Anterior - 80% (significant if gap >3mm b/n odontoid & atlas) - neck F worsens i.e. "sniffing" position for intubation Vertical - odontoid moves up foramen magnum Lateral - uncommon (>2mm significant) - spinal n & vert @ compression Posterior - rare - neck E worsens
Subaxial (below C2 >2mm significant (suspect if fusion at higher level) |
|
|
CEA LA vs GA & points for LA |
GALA trial LA vs GA: - No signif difference for CVA & mortality rates - Possibly long term benefit for LA - lower cognitive impairment
LA * Empty bladder* Deep Cx plexus ->phrenic nerve * 50% require surgical LA supplementation * 3% conversion GA * Monitor - dysphagia; LOC; confusion
|
|
|
Hyperperfusion Syndrome post CEA RFs |
* Stenosis >90% pre-op
* Pre-op HTN * Dec cerebrovascular reserve * Previous CVA (ischaemic) * Intra-op ischamia or emboli * Post-op HTN Rx - Aggressive Rx of HTN |
|
|
Renal Protection Strategies AAA |
PRE-OP * ID those at risk* D/W surgeon - clamp position & plan ?shunt * Baseline BP * Fasting - monitor U&E; volume & BGL * No drug proven useful * Avoid nephrotoxins & hyperthermia * IAL/CVL/IDC * Perfusion pressure - critical periods * U&E; BGL; Hb & O2 * As above - in HDU/ICU |
|
|
Non-Surgical Mx AAA |
Aspirin (level 1) Stop smoking (slows growth) Statins Consider B-B & ACE-i in high risk |
|
|
Define Anaesthesia Dolorosa |
Pain in an area of numbness |
|
|
Neuropathic Pain Def (More up to date version) |
Pain caused by a lesion or disease of the somatosensory nervous system
|
|
|
Consent - BRAN |
Benefits Risks Alternatives Nothing |
|
|
Cardiac Ablation Complications |
ABLATION Cx: * Vascular damage* Related to Trans-septal puncture ->atrial perf; Ao perf; Pericardial effusion; Tamponade * Related to LA ablation -> MV damage; Coronary obstruction * Arrythmias & Blocks * Oesophageal damage due to thermal injury (often have a T probe in) * Tx nerve injury - CNX & (L) RLNP * Embolic Cx * Atrial stunning ->PO * IE; Skin burns from electrodes
ANAESTHESIA Cx: Hypotension Suppression of arrhythmia (partic VA) Airway complications; Positioning
Overall Mortality 1:1000 Age > 75 & CCF - assoc w complications
NB Rate of long term arrhythmia control or cure ~70% |
|
|
CM5 ECG configuration - where are electrodes placed? |
C = Clavicle - neutral lead (left leg) - can be placed anywhere, but usually placed over clavicle M = Manubrium - RA lead 5 = LA on V5 Select lead one - gives vector pretty much straight down direction of conduction |
|
|
CS5 Configuration |
Central Subclavicular Lead RA on (R) clavicle (C) LL - ground (anywhere) LA on V5 Lead I - anterior ischaemia Lead II - inferiorSen
Best & easiest alternative to a true V5 lead for monitoring ischaemia |
|
|
Sensitivity of ECG leads |
5 lead: II, V4 & V5 - 96% (however can't select 2 chest leads with our monitors) II & V5 - 80%
When only one praecordial lead can be chosen - Choose most isoelectric |
|
|
MPS - Info provided - PPV & NPV |
INFO: 1. Perfusion 2. Structure - wall thickness 3. Function - EF NPV 99% PPV 10-20% |
|
|
MPS - Not indicated |
* Emergency Surgery
* Coronary revasc in last 5 yrs w no symptoms * Recent coronary evaluation w favourable result - no symptoms |
|
|
MPS Indications |
* Unable to interpret ECG (PPM, BBB)
* Unable to exercise >85% of max HR * Exercise stress test gives equivocal results * Elective non-cardiac surgery - with active cardiac condition * 3 or more clinical RFs, <4 METs - vascular surgery; & consider for intermediate Sx (?change Mx) * 1-2 clinical RFs, <4 METs - vasc or intermed Sx (consider if will change Mx) |
|
|
Benefits MPS |
* Defer surgery for PCI or CABG
* Reversible - predicts per-op cardiac events * High NPV of predicting peri-op cardiac event * Obese - echo may be poor qualityM |
|
|
MP Score Sn & Sp |
~60% alone |
|
|
Ax RLN nerve Post-operatively |
1. R/V NOTES - intubation difficulty; VC pre-intubation 2. VOICE CHANGES (Sn 33%; Sp 75%) 3. LARYNGOSCOPY - direct & indirect (nasendoscopy/video) 4. USS - Established validity 5. LARYNGEAL EMG - prognosis & distinguish paralysis vs cricoarytenoid jt damage (ETT)
NB Innervates all muscles of larynx except cricothyroid (superior laryng) B/L incomplete more dangerous than complete |
|
|
Atlanto-axial Instability Conditions |
RA Downs AS Trauma Osteogenesis imperfecta |
|
|
Cocaine Toxicity |
MOA - SNDRI Biphasic response - low concentration -> brady; high ->HTN; tachy; coronary spasm Cx & Mx: * VT - HCO3- & defib |
|
|
OSA Associated Conditions (that cause) |
* Excessive alcohol
* DM/metabolic syndrome * Smoking * Low physical activity * Unemployment * Tonsillar & adenoid hypertrophy * NM disease |
|
|
Conditions Assoc with Difficult Intubation |
* Syndromes - Downs; P-R; T-C
* OSA * Pregnancy (late) * Neck pathology - RA/AS; Trauma; Post radiation; Post burns |
|
|
Difficult Intubation Definition |
ASA (1993) Proper insertion of ETT with conventional laryngoscopy that requires more than 3 attempts &/or >10 minutes Incidence - 1-2% (Failed 0.3%)
Difficult Laryngoscopy = C&L Grade 3-4 view |
|
|
Examination Findings to Predict Difficult Intubation |
1. MP Score - Visibility of soft palate & uvula * 1/2 - small FN* 3/4 - high FP * Sn 45%; Sp 90% 2. Mouth opening - <2.5cm = difficulty 3. Mandibular mvt - trismus; Protrusion A/B/C (B = Teeth edge to edge) 4. Incisors & oral cavity - high arched palate; oral tumours 5. Neck & TMD - <6cm - v. difficult (PPV 75%) 6. Body Habitus - OSA; Neck circ >40cm; Large breasts; ability to BURP; Pregnancy |
|
|
Failed Intubation - CICO |
1. Call for help Consider: * Returning to spontaneous vent (?sugamma)* Waking patient up * 2 hands; jaw thrust * Guedels; NP 4. Insert SGA - LMA 5. Emergency Airway Access - perc or surgical trache.
NB if Successful ventilation/O2 steps 3-4 - move to non-emergency pathway |
|
|
Failed Intubation - Can Ventilate/Oxygenate |
Non-Emergency Pathway:
Alternative approaches to intubation * Video laryngoscopy* Intubating LMA * FOI
If failure - wake pt or proceed to emergency airway if can't wake (i.e. emergency surgery) |
|
|
Emergency Case - CICO |
Same as elective pathway except:
Aspiration risk - Cricoid pressure maintained t/out unless think that releasing will improve view - Possible use of sux (i.e. rapid wake up with sugammadex not an option)
Basically same except risk of aspiration & ability to wake up not as clear an optioni |
|
|
iLMA Sizes of ETT to fit |
LMA 3/4 - ETT 6.0 LMA 5 - ETT 7.0 |
|
|
Smoke Inhalation - Ax of Damage |
Upper Airway Thermal * Stridor/Voice change* Swollen uvula/Singed nasal hairs * Dyspnoea * Cough/Wheeze * Carbonaceous secretions * CO - unconscious (NB COHb doesn't correlate w severity) * Cyanide - Lactic acidosis
NB 100% O2 - reduces T1/2 CO 4 hrs -> 45min |
|
|
Smoke Inhalation - Intubation |
* Hypoxia/Hypercarbia/Resp distress
* GCS <8 * Stridor * Deep facial burns * Full thickness neck burns |
|
|
CI to Cricoid |
* Suspected laryngotracheal injury
* Active vomiting * Inadequate view on laryngoscopy * Unstable C-spine * Need for BMV i.e. rescue ventilation in failed airway |
|
|
Obesity Classes |
From BMI: Pre-Obese 25-30 (overweight) Class I - 30-35 Class II - 36-40 Class III - 41-49 (extreme obesity) Super morbidly obese >45P
|
|
|
Predictors of DI in Obese |
* OSA
* MP 3-4 * Neck circumference (>40cm = 5%; >60cm = 35%) * Pretracheal tissue (USS) * Other factors - * Three studies 2002-2003 (50-200 pts)A |
|
|
RFs for Aspiration |
Greatest risk - Emergency surgery; Light Anaesthesia; Abdominal pathology; Obesity
OTHER PATIENT - Increased gastric content (fasting; opioids; obstruction); LOS (pregnancy; GORD); Laryngeal reflexes (TBI; bulbar); Female; Elderly SURGICAL - Pneumperitoneum; Lithotomy ANAES - Difficult airway; BMV ->gastric; LightA |
|
|
Aspiration Mx |
1. Minimise further aspiration (suction; position; cricoid) 2. Secure airway 3. Suction - Trachea; Bronch 4. CXR (25% NAD initially)/HDU/ICU (if SpO2 <10% of pre-op; tachycard or tachyp; CXR changes) 5. ABs only if develop pneumonia (targeted)
No steroids |
|
|
Eye Muscle Cone - Contents |
* Sensory nerves
* Optic nerve (CN II) * Ciliary ganglion * CN VI * Retinal artery & vein
NB Formed by all muscles except inferior oblique NOT IN CONE - CNIV; Other V1 branches/V2 (frontal & lacrimal sensation to peripheral conjunctiva/lower lid) Apex of cone = annulus of Zinn |
|
|
Gabapentin - MOA & PK/PD |
MOA - Not completely understood - Effect on VG-Ca channels - Postulated - enhanced inhibitory input of GABA-mediated pathway; NMDA antagonism Oral prep only!
PK: BAV high but varies w dose; TDS dosing; Nil metabolised (renal excreted)
PD: Sedation (20%); Dizziness (18%); Ataxia; Fatigue; Convulsions (1%)
|
|
|
Gabapentin in Acute Pain - the evidence |
Level 1 evidence - single pre-op dose: * Opioid sparing (& subsequent decreased vomiting, pruritis & urinary retention)* Increased sedation * Similar efficacy to NSAIDS * Good for mvt-evoked pain * Anti-allodynia & hyperalgesia * Used in gps w RFs for CP - but no proof |
|
|
Gabapentin in Chronic Pain - evidence |
Level 1 evidence: * Neuropathic pain (NNT = 4)* Esp DM; post SC injury & phantom * Equal to TCA efficacy, but better SE profile * Sedation may be beneficial (sleep) Limited evidence for other chronic post-surgical pn states |
|
|
Pain History |
Nature Location Intensity Duration Onset/Offset Associated Symptoms Aggravating/Relieving Radiation Functional Impairment
|
|
|
Mx & Prevention of Phantom limb pn - evidence |
PREVENTION - Epidural reduces incidence; Ketamine reduces severity (cont for 3/7)
Rx - MDT & Multimodal: * PHARM - TCA best; tramadol good; Gaba effective; Opioids effective; calcitonin for acute only; nerve blocks (all used with some success)* NON-PHARM - very little evidence, but all low risk options & valuable adjuncts (e.g. TENS; acup; PT; USS; Hypnosis) * SURGICAL - Unfavourable - stump RV only if local pathology * PSYCH/OT - Sensory discrimination (level II); Mental imagery (IV); Formal psych (CBT) * SOCIAL - Coping mechanisms; Rx depression
|
|
|
Analgesia & Antiemetics Classification Pregnancy |
A - Paracetamol/Bupivacaine/Lignocaine/Codeine /Metoclopramide B1 - Ropivacaine/Gabapentin/Granisetron B2 - Domperidone/Hyoscine B3 - Clonidine/Ketamine C - Other Opioids/Aspirin/Promethazine D - Anticonvulsants/Paroxetine
NB Opioids - Short term treatment appears safe - at a minimal dose (concern - neonatal abstinence syndrome) |
|
|
Pregnancy Drug Classification |
A - Safe in large number of pregnant women B - Appears safe in humans - variable safety in animals: B1 - Safe in animals B2 - May be unsafe in animals B3 - Appears unsafe in animals C - Have caused, or suspected of causing harmful effects in foetus without causing malformation D - Have caused, or suspected of causing foetal malformations or irreversible damage X - Such high risk of foetal malformation that shouldn't be used if any chance of pregnancy |
|
|
Classes of drugs in persistent pain? |
Simple analgesics Anticonvulsants (Old - carbamazepine; valproate - level I; New agents - gaba; lamotrigina - Level III-IV) Antidepressants (TCAs - level I) Membrane stabilisers e.g. some anticonvulsants; lignocaine (level II) Opioids |
|
|
Assessing pain in dementia pt - methods |
Both understanding of scores & ability to communicate impaired * Many tools e.g. Checklist of non-verbal Pain Indicators (CNPI) - validated* Examples - Grimacing; Bracing; Rubbing; Restlessness * Can use observations by caregivers - usual pain behaviour & change in behaviour NB Vital signs are not accurate reflection |
|
|
Problems with naltrexone |
Naltrexone = opioid antagonist Long DOA (T 1/2 14hrs) May have up regulation of opioid Rs Opioid beneficial - Co-induction; Sole anaes agent ('CVS stable'); Balanced GA
Cease 24-48hrs if possible If not able to cease: Intra-op - consider lignocaine or esmolol; Increase induction agent dose; alternative analgesia; BIS; Remi Post-op - Regional; Multimodal; Adjuncts |
|
|
Mortality for lobectomy vs pneumonectomy ppo FEV1% for above + wedge resection |
Pneumonectomy 6-8% Lobectomy 2-4%
ppo FEV1%: Pneum 55% Lobectomy 40% Wedge resection 35% |
|
|
Checking DLT |
R vs L 1. CLINICAL * Intubate Trachea - tip anterior & rotate 90 deg* Inflate Tracheal lumen - check vent * Clamp Tracheal limb & open tracheal sealing cap - inflate bronchial cuff slowly until no leak & OLV (unclamp & reseal) * Clamp bronchial lumen - check other OLV * 25-80% still malpositioned! * Gold standard - repeatable; minimally invasive * Blue cuff not herniated; Carina; UL not obstructed (esp RUL) * Left side bronchi - secondary carina * Right side bronchi - trifurcation * Radiation/Time * Difficult to define carina & position relative to ULs 4. CAPNOGRAPHY/SPIROMETRY |
|
|
RFs RDS Thoracic Surgery |
* (R) side pneumonectomy
* Increased IV fluids peri-op (>3L/24h) * Inc UO post-op * Increased TV 8ml/kg |
|
|
Blood Loss Trauma Causes |
SCALPeR
S = Scalp (esp children) C = Chest A = Abdomen L = Long bones, esp femur P = Pelvis R = Retroperitoneal |
|
|
Pulse palpation & approximate BP |
Only carotid - SBP 60-70 Only carotid & femoral - 70-80 Carotid, radial & femoral - 80-90
Always disappear in that order - but values vary individually
|
|
|
Haemorrhage Adults - Estimating amt |
Grades I - IV based on % blood volumes: 15 - 30 - 40 - >40 (game over) * GII - HR >100 & dec pulse pressure * GIII - BP decreases * RR - GII (>20); GIII (>30)
Don't really bear out in reality - age/comorbidities /Meds (e.g. BB) |
|
|
Final common pathway coagulation |
Prothrombin (2) -> Thrombin (2a) -> Fibrinogen -> Fibrin Fibrin + platelets = platelet-fibrin matrix = Haemostasis Extrinsic (7a) - converts 10 ->10a |
|
|
Recombinant Factor VIIa Pros & Cons |
PROS: * Licenced bleeding haemophilia A&B* Theory * RCTs - Decreased RBCs & ARDS (blunt trauma, not penetrating); ICH (w/i 1hr) - Decreased haematoma & mortality * Cons of blood products & MTx * Quick & easy to use * No storage probs * Apart from ICH - no evidence of dec M&M * Possibly publication bias * Off licence for trauma * Expensive (1 vial/1.2mg = $1200) * SEs - Significant increase in arterial TE events (likely coronary) * No real agreed protocol * Needs platelets, fibrinogen & Ca to be effective |
|
|
Approach to using rFVIIa |
Use in life-threatening bleeding & MTx. Consider use in ICH Consider when pt has had: * 10 RBC; 8 FFP; 2 Plt; 2 Cryo* TXA considered * Plt >100 * Fibrinogen >1 * T >35 & pH >7.2 * Warfarin/heparin reversed
Dose - 100mcg/kg - round up to nearest 1.2mg vial. Wait 20min - repeat |
|
|
TRAUMA - ATLS Approach |
Primary Survey - ABCDE + avoid secondary insult AMPLE / MIST A - Airway maintenance & C-spine B - Exposure & inspection - Chest surgical emphysema/Tension (may only become apparent after PPV) C - Permissive low BP (poor evidence) - but SBP <90 -> mortality increases x2; Find the bleeding & stop it (remove all bandages); IV & Ix D - GCS; AVPU - Severity of TBI; Is suspect spinal -> priaprism & anal sphincter tone; BGL E - T/Expose/log roll Adjuncts - FAST; XR; OGT; IDCT Secondary Survey - Top to Toe O/E |
|
|
Trauma - Deadly Dozen |
Lethal Six 1. Airway obstruction2. Tension 3. Tamponade 4. Open PTX 5. Massive HTX 6. Flail chest 7. Thoracic Ao disruption 8. Tracheobronchial disruption 9. Myocardial contusion 10. Traumatic diaphragm tear 11. Oesophageal Disruption 12. Pulmonary contusion |
|
|
Laryngeal Cartilages |
3 Unpaired: * Thyroid (C4-5) - BURP* Cricoid (C6) * Epiglottis (C3-4) * Arytenoid - move VC * Cuneiform * Corniculate * Thyrohyoid * Cricothyroid * Cricotracheal * Isthmus overlies tracheal rings 2-4 |
|
|
TPN Complications |
Related to CVL: * Infection* Occlusion (usually 1st rib & clavicle) * Fibrin sleeve * Thrombus * Erosion - SVC/RA * Hyperglycemia * Hypercholest * Refeeding * Abnormal LFTs * Acidaemia * Volume * Trace element deficiences (thiamine; Vit K; Copper; Iodine; Selenium)C |
|
|
Classification of Shock |
* Cardiogenic
* Hypovolemic * Distributive * Neurogenic (SNS) * Obstructive * Endocrine/Metabolic (Addisons) |
|
|
ScvO2 Pros & Cons |
Normal O2 extraction 25-30% - corresponds to SvO2 >65% Intermittent or continuous Pros: * Continuous reading - earlier than MAP/HR - guide & response to Rx* Only requires CVL - no added risk * EGDT - >70% part of strategy that reduced mortality in sepsis (16%) * Global change only * Surrogate for SvO2 * Doesn't reflect myocardial perfusion * Lactate clearance - non-inferior * ScvO2 < SvO2 normally (CNS extraction ratio) - reversed w Dec CMRO2 * Falsely elevated in cyanide * Interpretation errors - intracardiac shunts, TR & CVL malposition
|
|
|
Timing of Smoking Cessation & Changes |
One day -> Decreased COHb & nicotine (expect increased tissue O2 delivery) 3/52 -> Wound healing 6/52 -> Sputum volume & pulmonary function 6/12 -> Immune function
Ask Advise Refer
Following abdo surgery - 6x increase in resp complications |
|
|
Pneumothorax Causes |
1. Spontaneous - Primary - healthy, no lung disease; often tall smokers - Secondary - Underlying lung disease 2. Traumatic - High inflation pressures - Complication of surgery/Iatrogenic
Risk of recurrence of spontaneous PTX is 54% at 4 yrs |
|
|
Common Peri-op nerve injuries of UL |
* Ulnar nerve (30%)
* Brachial plexus (20%) - stretch; compression (sternal retraction) * Radial nerve - compression by humerus * Median -cubital fossa * MC - BP cuff
Aetiology - Stretch; Compression; Ischaemia; Metabolic derangement; direct trauma (needle, diathermy); LA injection |
|
|
RFs for Peripheral Nerve Injury |
PATIENT * Pre-existing neuropathy / DM / Smokers* Pre-existing ulnar nerve palsy * Congenital abnorm (e.g. extra rib) * Arthritis * Thin; Female; Elderly * Hypovolemia/dehydration * Intra-op hypotension * Hypothermia * Poor positioning * Electrolyte abnormalities * Arterial tourniquet * Sternotomy |
|
|
Failure to Emerge from GA - Causes |
4 S's
Sedatives/Drugs * Residual anaesthesia/NMBD (liver/renal failure/age extremes)* Other - opioid; ketamine; central anti-cholinergic syndrome * In posterior circulation involving thalamus * Dissection of Ao -> vert origin * Acute hydrocephalus * Paradoxical embolism * LA * Non-convulsive or seizures w NMBD * Hyponatraemia * Hypoglycemia * Thyroid * Uraemia * Hypothermia * Hypercarbia |
|
|
Anti-emetic Rx for PONV |
If prophylactic drug failed - use anti-emetic from a different class Re-administer if >6hrs in PACU Don't re-administer droperidol? |
|
|
Impaired Colleague |
DEF - Inability to safely & competently practice anaesthesia at a standard appropriate for a given environment * Primary obligation to patients* Secondary obligation to colleague * Gather evidence * Pre-plan confrontation - formal meeting * Plan post-confrontation * Other obligations - dept; medical board; college |
|
|
Decreasing risk of awareness |
1. BDZ pre-med 2. Dont titrate anaesthetic agents to CVS or resp depression 3. EtVA >0.8MAC 4. Only use when required NMBD 5. BIS/entropy - in high risk patients (B-aware trial) - LSCS; Emergency; Hx previous awareness OR clinical signs of awareness may be masked |
|
|
OHGs |
1. Biguanides e.g. metformin - promote utilisation glucose & decrease production
2. Glitazones - peripheral 3. Sulphonureas - increase insulin secretion & peripheral (hypo) 4. Acarbose - glucosidase inhibition |
|
|
Peri-op Probs DM |
* Stress response -> hyperglycaemia
* Interruption of food/meds * Altered consciousness - mask hypo * Circulatory disturbance - may impair sub cut absorption * Post-op would healing |
|
|
Required to cough? |
VC should be twice TV |
|
|
Rheumatoid Arthritis - Anaesthetic Implications |
C-Spine * Subluxation - laryngoscopy & positioning (quadriplegia/death)* Refer for fusion; RA or MILS * TMJ, cricoarytenoid & Rh nodules * AFOI; C-Mac & airway obstruction extubation * Symptomatic relief - Steroids (cover); NSAIDS (renal; GIT; bleeding); Opioids (tolerance/RA) * Disease modifying - MTX (pulm; bone marrow; LFTs); Sulfasalazine (LFTs; photosens) * Anti-cytokine - Infliximab (monoclonal AB) * Pericardial effusion; Endocarditis; Raynaud's; Atherosclerosis & CAD; Diastolic * ECG & ex tolerance pre-op; 5-lead & IAL * Fibrosis; Nodules; Effusions * Anaemia common - multifactorial (ACD; Fe; drugs -> bone marrow) * CRF common (drugs) - 25%! * Hepatomegaly; Splenomegaly * CVL - Cx * Vasculitis/steroids/FFD wrist = difficult * Pros - C-spine; airway; LFT/CRF; Pain * Cons - Inc risk of high SA; Pn w prolonged immobility * PCA difficult * Positioning * Eye drops for kerato-conjunctivitis * Infection risk (drugs) * DVT (mobility) |
|
|
Bone cement implantation syndrome - Grades |
Methyl methacylate
Grade 1 - Mod hypoxia or hypotension Grade 2 - Severe ditto OR unexpected LOC Grade 3 - CVS collapse |
|
|
DIC |
Disseminated Intravascular Coagulopathy Widespread activation of coagulation -> consumptive coagulopathy LAB: * Increased PT/D-dimers/Fibrin degradation products* Decreased fibrinogen/plts * Treat underlying problem * Maintain circulating volume * Replace products
|
|
|
Pk of Dabigatran & Rivaroxaban |
Dabigatran: Prodrug - converted by plasma esterases T1/2 (hrs) - dependent on renal function & increases w chronic dosing - Normal = 14; Mild-Mod = 16-20; Severe = 30 Elim = 80% renal; 20% metab (active metab) Monitoring - aPTT or TCT Rivaroxaban: T1/2 (hrs) - 7.5 (with severe renal impairment = 9.5) Elim - 33% renal; 66% metab Monitoring - PT or anti-factor Xa assay |
|
|
Rivaroxaban vs Warfarin Effects |
R vs W:
CVA reduction w AF: 1.7 vs 2.1%/yr ICH bleeding - R < W GIT & bleeding requiring Tx - R > W
|
|
|
Dabigatran vs Warfarin Effects & SEs |
D vs W:
VTE/death post TKR - D = W CVA/emboli w AF: Lower dose - D = W effect; D < W bleeding Higher dose - D > W effect; D = W bleeding (although W - ICH more common & D - GIT more common)
NB DABIGATRAN - CI w prosthetic heart valves (trial terminated early as increased thromboembolic events - valve thrombosis, CVA, MI, & bleeding > W) |
|
|
Neuraxial Guidelines for Dabigatran & Rivaroxaban |
ASRA - Avoid European - 24hrs post dose for insertion & removal for R (D - CI); Dose after removal - 6hrs TGA - D - CI for insertion, but dose 2hrs post removal. R - 18hrs for insertion/removal post dose; and dose 6hrs post removal
|
|
|
Spinal USS - Steps |
1. Sitting flexed position
2. 2-5Hz Curved array probe; Depth to 9-12cm 3. Paramedian sagittal oblique view scan - 2-3cm lateral to midline at sacrum - point towards midline & identify sacrum, then move cephalad to reveal 'sawtooth' appearance of laminae. Mark L5-S1 interspace, then move up & mark the rest 4. Transverse inter laminar view - Rotate probe 90 degrees & slide cephalic or caudal to ID inter laminar spaces (bat appearance or mickey mouse!) 5. Measure needle insertion depth w US - from skin to posterior complex (ligamentum flavum/dura mater 6. Mark the midpoint on the probes long & short sides w inter lamina space on screen - intersection of these lines is the needle insertion point (for midline approach) |
|
|
Substance Abuse Management |
1. Prevention* Drug test screening
* Electronic signing out drugs/regulated dispensing * Discard unused drugs (witnessed) * Investigation * Intervention * Detoxification * Rehab * Monitoring & Surveillance * Only 20% make a long-term recovery w/i anaesthesia * 25% Death is initial relapse symptom & indication of propofol abuse (30%) |
|
|
Specialist Referral for Burns |
* >5% full or partial (paed)
* Chemical or electrical * Inhalational * Pre-existing medical conditions * Concomitant trauma * Burns to face, hands, perineum or feet |
|
|
Modified Parkland Formula |
%BSA x 4ml x weight = 24hr fluid
Give half in 1st 8hrs, half n next 16hrs
Burns oedema maximal in 1st 18-30hrs Re-assess fluid needs w CRT, mental state & UO
Don't forget to treat pain |
|
|
RSI Steps |
1. Equipment - machine, drugs, airway, suction, IV access 2. Assistance - cricoid + airway 3. Monitoring 4. Pre-oxygenate; Aspirate NG 5. Induction 6. Intubation |
|
|
Dose & drugs for caudal |
Bupivacaine 0.25% 1ml/kg - long DOA; Motor blockade short time may be helpful (levi & ropiv not licenced) Adrenaline 1: 200 000 - Slightly increases DOA; IV; decrease absorption (minor); Con - ?arachnoiditis Fentanyl - Aids quality; Cons - opioids SEs |
|
|
Apnoea RFs paediatrics |
* Premature (<36.40) - up to 60 weeks PCA
* Term - < 44 weeks PCA * Anaemia |
|
|
Physiological anaemia of pregnancy - nadir
|
Birth 16-18g/dL Nadir 3 months - 9-10g/dL By 8 months - 12
|
|
|
Maximal allowable blood loss calculation Paediatric blood volumes |
pre-op Hb - trigger Hb/pre-op Hb x EBV
Estimated blood volume (EBV): Preterm 90-100ml/kg Term 85-90 Infants 80 School age 70 Adult 70 |
|
|
Risks of Epidural with numbers |
1. Shivering & Itch up to 50%
2. Failure/unilateral - 1 in 20 3. Hypotension - Severe 1 in 50 4. IDC 5. PDPH 1 in 100 6. Mild bruising/back pain 7. IV 1 in 500 8. Subdural <1 in 1000 9. Total spinal 1:1000 10. Nerve injury - Reversible 1:500 Neuropraxia 1:1000 - 1:10000 Paralysis 1:200000 11. Abscess 1:25000 12. Haematoma 1:150000 |
|
|
Nimodipine Dose |
Oral - 60mg Q4H IV - 0.5mg/kg/min No difference between oral & IV (new evidence) Start as soon as diagnosis made (w/i 96hrs), & continued for 21 days Cerebral infarct RRR 35% Overal mortality RRR 40%
SEs: - Hypotension - Nausea - Headache
|
|
|
Definition of Sentinel Event |
= Relatively infrequent, clear-cut events that occur independently of a patient's condition, commonly reflect hospital (or agency) system & process deficiencies; and result in unnecessary outcomes for patients |
|
|
Reportable Sentinel Events (8) |
1. Procedures involving wrong patient or body part resulting in death or major permanent loss of function
2. Suicide in an inpatient unit 3. Retained instruments or other material during surgery, requiring re-operation or further surgical procedure 4. Intravascular gas embolism resulting in death or neurological damage 5. Haemolytic blood transfusion reaction from ABO incompatibility 6. Medication error leading to death of pt reasonably believed to be due to incorrect administration of drugs 7. Maternal death or serious morbidity assoc w labour or delivery 8. Infant discharged to wrong family or abduction |
|
|
Blood transfusion Paediatrics: Maximum allowable blood loss (MABL) Hb increase Blood volume |
MABL = Initial Hb - Final Hb x blood volume Initial Hb
4ml/kg of packed cells increases Hb by 1g/dL
Blood volume - Prem 90ml/kg; Infants 80ml/kg; Child 70ml/kg |
|
|
Quantities Calcium in Calcium Chloride & Gluconate & Dose in Hypocalcemia |
CaCl 10ml = 27.2mg CaGluconate 10ml = 9.3mg
Adult - 500-1000mg over 5-10min Paed - 10mg/kg over 5-10min (?from medscape - check) |
|
|
Definition of ARDS |
An acute, diffuse inflammatory lung injury, leading to increased pulmonary vasc permeability, increased lung weight & loss of aerated tissue, with hypoxemia & bilateral radiological opacities & decreased lung compliance.
(Berlin Definition - published Sep 2013) |
|
|
Paediatric weight calculation |
Infants = (age in months + 9) / 2
Age 1-10yo = (age + 4) x 2
> 10 = age x3 (large variation) |
|
|
Paediatric SBP |
> 1yr = 80 + (age x 2) |
|
|
Paediatric ETT size & length |
> 2yrs
Age / 4 + 4 = Uncuffed size
For cuffed -> minus 0.5
Length: Age / 2 + 12 Neonates = weight + 6 (preterm; term; post-term - 7,8,9) |
|
|
Children at risk of hypoglycaemia |
* < 3-6 months
* < 2-3 yrs who are malnourished, likely to have poor glucose reserves or have had a prolonged fast * Extensive regional blockade (prevents hyperglycaemic response during surgery) * Receiving TPN * Metabolic syndromeI |
|
|
Insulin infusion in DKA |
50 units in 49.5ml -> 1 unit/ml
0.1U/kg/kr BGL >15
0.05U/k/hr BGL < 15 |
|
|
Corrected Na in hyperglycaemia |
Corrected (i.e. actual) Na = measured Na + 0.3 (glucose - 5.5) mml/L
i.e. Na is actually higher than measured in lab (pseudohyponatraemia)PCA |
|
|
Paediatric PCA - morphine & fentanyl |
MORPHINE: 0.5mg/kg in 50 ml = 10mcg/kg/ml. Bolus 1-2 ml; Lockout 5 min (if >50kg - as for adults)
FENTANYL: 15mcg/kg in 50ml = 0.3mcg/kg/ml. Bolus 1ml; Lockout 5 min (>50kg - 750mcg/50ml = 15mcg/ml) |
|
|
Sedation Score |
University of Michigan Sedation Score:
0 = Awake & alert 1 = Minimally sedated; may appear tired/sleepy, responds to verbal conversation &/or sound 2 = Mod sedated: somnolent sleeping, easily roused w light tactile stimulation or simple verbal 3 = Deep sedation: deep sleep, rousable only w deep or significant physical stimulation 4 = Unrousable S = Sleeping |
|
|
Naloxone dose paediatrics |
Pruritis = 1mcg/kg Sedation = 2mcg/kg Resusc = 10mcg/kg |
|
|
Routine extubation criteria |
* Awake, alert, able to follow commands
* Vital signs stable * Protective reflexes (gag, swallow, cough) * NMBD reversal * Good gas exchange w FiO2 0.4 (O2>60) * Respiratory mechanics adequate (TV>5ml/kg; negative insp force >20cmH2O) |
|
|
Signs of hypocalcemia |
* Tingling fingertips & peri-oral
* Carpopedal spasm * Tetany - Chovsteks (CNVII) & Trousseau (BP cuff) * Prolonged QT * Laryngospasm * Seizures * Arrhythmias |
|
|
Topical lignocaine - max dose Co-phenylcaine spray - dose of lignocaine & phenylephrine |
9mg/kg = Max dose for topical lignocaine
Cophenyl spray - 5% lignocaine & 0.5% Phenylephrine Each spray = 0.1ml = 5mg lignocaine & 0.5mg phenylephrine
If nebulise LA ~25% is absorbed |
|
|
To achieve good handover need: |
* Shifts must cross-over
* Adequate dedicated time * Clear leadership * Adequate information technology support * Support of handover process from all members of team |
|
|
Temp to start active cooling in phaeo, thyroid storm, cocaine toxicity |
41 degrees |
|
|
Branches of cervical plexus - anterior rami |
Superficial (sensory - superior to inferior): * Greater auricular* Lesser occipital * Anterior cutaneous/transverse cervical * Supraclavicular * Phrenic nerve - diaphragm * Ansa cervicalis- hyoid musculature NM Greater occipital from dorsal rami of C2 |
|
|
Transport of Critically Ill (PS52) |
* No step down
* Communication; Responsibility; Documentation; Governance * Monitoring - * Assistance (Intra-hospital) - nurse, orderly & medical practitioner * Drugs - to keep asleep, manage hypotension/bradycardia & manage emergencies (Thomas pack) * Equipment - to manage complications of ABC (tubes; LMAs; blades) * Know your ROUTE * Before I depart - making sure pt is stable, all equipment is battery charged & excess O2 in cylinder for distance |
|
|
Definition of Handover |
The transfer of professional responsibility & accountability for some or all aspects of care for a pt, or group of pts, to another person or professional group on a temporary or permanent basis |
|
|
Smart Phrases |
My principle aims I am concerned about......., to prevent this I am going to aim for e.g. SR, maintain preload & after load ...... Underlying principles |
|
|
Pringles Maneouvre - What is it & physiological consequences Tumours near IVC - possible surgical action |
Clamp of portal vein & hepatic artery - results in temp occlusion of blood to liver. Consequences: * Decrease CO up to 10%* Increase LV afterload 20-30% * Above may cause CVS compromise * Hypoglycaemia (closely monitor) * May clamp supra- & infra-hepatic vena cava & hepatic pedicle - assoc w drop in CO up to 60% & severe hypotension
|
|
|
Handover - ISBAR |
Identification Situation (if urgent - say so) Background Assessment (ABCDE) Response |
|
|
Stages of Anesthesia |
1. "Induction" - between drugs & LOC
2. "Excitement" - follows LOC, marked by excited & delirious activity - irregular HR & RR; laryngospasm, bronchospasm; divergent eyes - longer w gas inductions 3. "Surgical anaesthesia" - (4 substages) - lack of lid & corneal reflexes; pupils midline; regular respiration 4. "Overdose" - respiratory arrest; if drugs continued possible cardiac arrest |
|
|
Complications after liver resection |
* Liver failure - usually present 72hrs post (increased risk pre-existing cirrhosis or biliary tract obstruction)
* Sepsis * Major bleeding * Renal failure * Respiratory failure
NB 50% pts will get significant self-limiting ascites in 1st 48h - can cause hypovolemia Low serum UREA on day 1 - early sign of liver dysfunction LOW RISK - <50% resection in non-cirrhotic
|
|
|
Liver resection important points |
* Suggested that pts w Child-Pugh score of B or C shouldn't receive liver resection
* Can do epidural for liver resection but keep a close eye on INR & if prolonged may need to cover catheter removal w FFP * Normothermia (coagulation); large IV access * Main source bleeding valveless hepatic veins therefore CVP <5 crucial - use dobutamine or phenylephrine for hypotension * High CVP - Rx w GTN or diuretics * Can restore blood volume after resection phase as risk of bleeding is reduced * Avoid PEEP during resection phase * After resection phase - can restore blood volume as risk of bleeding is much reduced * Intermittent clamping (10 min on , 5 min off) - effective in hepatic protection (ischaemia-reperfusion injury) * No paracetamol until Fx restored |
|
|
Causes of failed handover |
* Inadequate time
* Inadequate training * Fatigue/Stress * Distracted * Language * Lack of respect for handover process |
|
|
Purpose of GA |
Amnesia Analgesia Immobility (loss of motor reflexes) Unconsciousness Skeletal muscle relaxation |
|
|
Treatment hyperkalaemia |
* Treat >6.5mmol or ECG changes
* Treat the cause if possible * Insulin 10U in 50ml 50% - over 30-60min * Calcium gluconate 5-10ml (may need to repeat) * If acidotic - give bicarb * B2 agonist - neb salbutamol * Ion exchange resin (calcium resonium PO or PR) * If initial Mx fails - don't forget DIALYSIS |
|
|
Haemophilia - restoration of clotting factors pre-op & Mx |
X-linked <1% = Severe deficiency 1U factor concentrate/kg for 2% increase Want clotting factor activity 40% of normal FFP = 1U/ml & cryo = 20U/ml NO NSAIDS May be on immune modulators (e.g. rituximab) + steroids CVL w US; No IM injections; Care w intubation Consult - haematology & admit all pts (even for minor procedures) Haemophilia B (IX) - can give PTX Haem A (VIII) - not in PTX |
|
|
Von Willebrands Disorder |
CONGENITAL: Most common hereditary coag disease - autosomal Deficiency/abnormal VWF Type I - Quantitative; Response to ddAVP Type II - Qualitative; Many subtypes Type III - Most severe; no response to ddAVP
ACQUIRED: - Aortic stenosis - SLE - CHD - Wilms tumour - Hypothyroid
|
|
|
ddAVP (Desmopressin) |
Synthetic analogue of ADH Intranasal & IV (& SC) Peak response 45-90 min Repeat every 12-24hrs
|
|
|
Peripheral nerve injury nerve block Incidence |
Depends on location: - Interscalene 3% - FNB 0.3# - Supraclavicular 0.03% Majority are temporary & resolve over weeks to months In general - overall 1/100 Permanent 1/10000 Transient deficit up to 10% |
|
|
Risks Blood Product Transfusion |
* TACO 1/100
* Haemolytic reaction - delayed 1/5000; Acute 1/50000 * Anaphylaxis (IgA deficiency) - 1/50000 * Bacterial sepsis - plts 1/75000; RBCs 1/500000 * TRALI - 1/100000 (variable though) * Hep B - 1/700000 * HIV/Hep C/malaria - <1/millions * CJD - never in Australia |
|
|
Calman Chart of Risks |
> 1/1000 - Chicken pox transmission in household 1/1000 - 1/10000 - Death from road accident - 1/100 000 - Death from work accident - 1/1000 000 - Death from train accident - >1/1000 000 - Death from lightning strike |
|
|
Peripheral nerve anatomy |
Nerve fibres surrounded by endoneurium, enclosed in fascicles, surrounded by perineurium. Fascicles are embedded within stromal tissue & surrounded by epineurium. (Intrafascicular injection assoc w injury) |
|
|
Spinal cord meninges |
PAD: Pia Arachnoid Dura |
|
|
Dexmedetomidine Infusion |
Studies CEA - Sedation 0.2-0.4mch/kg/hr - comfortable & cooperative pt
Less agitation & respiratory depression than proposal infusion or boluses of fentanyl +/- midazolamW
|
|
|
What is damage control surgery?
|
Timely use of a staged approach in the treatment of the actively bleeding shocked patient. Emphasises control of bleeding & prevention of further contamination, to allow the correct of T, pH & coagulopathy before definitive surgery is undertaken |
|
|
What is permissive hypotension? |
SBP 80-100 tolerated while bleeding is controlled (particularly ruptured AAA) CI in TBI |
|
|
Mx laryngospasm in a child |
1. Jaw thrust & CPAP
2. Propofol 1-3mg/kg 3. Sux - IV 0.5-2mg/kg IM 4mg/kg into deltoid - takes 3-4 min for peak effect but will effect VC much earlier NB SpO2 reading is averaged from last 10-15sec therefore may stay low for a while. Watch for chest mvt After SpO2 improved & sux still working - suction pharynx to remove secretions NB A cough under GA w LMA or mask is warning sign of laryngospasm - worth giving bolus of proposal |
|
|
MTP Triggers |
Actual or anticipated 4 U PRBC < 4hrs + haemodynamically unstable +/- anticipated ongoing bleeding >150ml/min
Children - >40ml/kg in 4 hrs (half blood volume) |
|
|
MTP - Special Considerations |
Obstetric - look for DIC; consider cryo; want fibrinogen >2.5 Head injury - Plt >100; permissive hypotension contraindicated Warfarin - Vit K; PTX; FFP |
|
|
MTP Targets |
Calcium >1 pH >7.2 Temp >35 Lactate <4 BE > -6 Fibrinogen >1.5 INR <1.5 APTT <1.5x normal Hb >70 Plt >75 |
|
|
Doses of blood products in children |
RBCs 4ml/kg increased Hb by 1g/dL (mix w albumin if ongoing bleeding - facilitates rapid administration) FFP 10ml/kg Cryo 5ml/kg Platelets 5-10ml/kg |
|
|
SSEPs & MEPs Significant Changes |
SSEPs & MEPs: * >50% amplitude* >10% latency * Loss of MEP * Increase in stimulation threshold |
|
|
What affects accuracy of Evoked potentials? |
SSEPs: * NMBD increase accuracy* Sensitive to temp & LAs * More stable during surgery i.e. less affected by VA * NMBD decrease amplitude * VAs & propofol (?keep <0.5MAC)
Epidural recordings of both SSEPs & MEPs - more robust than cortical or muscle readings as less polysynaptic transmission |
|
|
EDH vs SDH |
EDH = biconvexity (think Egg shaped = E) SDH = crescent EDH: * Most temporoparietal region* Commonly middle meningeal ARTERY bleed (30% venous) * |
|
|
SSEPs utility |
* Stimulus to peripheral nerve (usually CP, PT or median)
* Decrease neuro injury in traumatic spinal instability 7% to 0.7% * Can detect subcortical ischaemia (unlike EEG) * UL - primarily dorsal columns * LL - includes components from spinocerebellar pathway (ASA) |
|
|
MEPs utility |
* Pure motor tract monitoring
* Motor cortex -> cortical spinal tracts ->anterior horn cell -> peripheral nerve -> muscle * Can detect at spinal cord or muscle |
|
|
Features of Aneurysm Suitable for Coiling |
* Narrow neck (although can treat wide neck w fenestrated stents)
* |
|
|
Don't forget..... |
Surgeon Consult with other specialities Haemorrhage - pressure bag & level 1 in OT |
|
|
If anticipating blood loss - preparation |
* Pre-op optimisation of pt's Hb if possible (iron, EPO)
* Correct coagulopathies * Experienced surgeon * Large IV access & IAL * Temp monitoring * Vasopressors * Blood - Xmatched or in OT * Level 1 in OT - primed * Warm OT if trauma * 2nd anaesthetist * Cell saver
|
|
|
CN III palsy |
* Susceptible to compression in cavernous sinus than other CNs (3, 4, V1 & V2 + 6 in the middle)
* Ipsilateral ptosis * Ipsilateral pupillary dilation * Diplopia * Cavernous sinus (CS): - Pituitary gland lies between 2 CS therefore adenomas will compress CS |
|
|
Risk Factors for Awareness |
DR AWARE: DR = DRUGS = EtOH; Chronic BDZ; Opioids; Current protease inhibitors A = Acute trauma w hypovolemia W = Women (LSCS) A = Awareness in past; Anticipated DI R = Rigid bronch; high Risk cardiac surgery (EF <30%; CI <2.1; Severe AS; Pulm HTN; off-pump CABG) E = End stage lung disease
BIS - NNT = 138 (cost $2200 to prevent one incidence of awareness) |
|
|
Protease inhibitors - drug interactions |
Many drugs & interactions!! Most drugs shouldn't be co-administered: * Anti-arrythmics (absolute)* Rivaroxiban (heparin is ok) * BDZ * Sevo may interact (iso is ok) * Propofol & roc may interact (Thio, vex & cis are ok) |
|
|
Tapentadol - MOA; Indications; Dose equivalents; Efficacy; SEs |
MOA - Mu receptor agonist & NARI Indications - moderate chronic pain unresponsive to non-narcotic analgesia; Studied in LBP & OA As good as oxycontin Morphine : Tapentadol 1 : 2.5 SEs - similar to other opioids, w less GIT adverse effects Interactions - MAOIs; mostly glucuronidation, small amount CP450
|
|
|
Budapest Criteria for CRPS diagnosis |
A - Patient has continuing pain which is disproportionate to inciting event B - Patient has at least 1 SIGN in 2 or more of the categories C - Patient has at least 1 SYMPTOM in 3 or more of the categories D - No other diagnosis can better explain the signs & symptoms CATEGORIES: Sensory - allodynia; hyperalgesia Sudomotor - Oedema; Sweating changes Vasomotor - T asymmetry (>1 degree); Skin colour changes/asymmetry Motor/trophic - Dec ROM; Motor dysfunction; Trophic changes
|
|
|
Non-obstetric surgery in pregnancy |
* If possible - delay until 6/52 postpartum
* Miscarriage risk 5%; 10% in 1st trimester (organogenesis weeks 3-8) * Antacid prophylaxis 14/40 * ACC 20/40 * DVT prophylaxis - always * CO2 - aim normal (high -> uterine VC; low -> ODC (L) shift * Airway - from 2nd trimester * RA > GA (but no evidence, & use less LA by 1/3) * Pre-O2 3 min * Maintain uteroplacental perfusion - avoid catecholamine release * Outcomes - likely to deliver early & have smaller baby, regardless of timing |
|
|
Anaesthetic Drugs in Pregnancy |
* 1st trimester - avoid N2O
* Single dose of BDZ - no link to teratogen (cleft palate w diazepam) * Ketamine & LA -> increase uterine tone * Avoid NSAIDs * NMBDs; Opioids; Induction agents all ok - as long as maternal physiology maintained
Miscarriage risk - probably uterine irritability (greatest risk w lower abdo/pelvic procedures) |
|
|
Caesarian Urgency Categories |
Cat 1 = Urgent threat to LIFE of mother or foetus Cat 2 = Maternal or foetal COMPROMISE, but not immediately life threatening Cat 3 = Needing earlier than planned delivery, but without currently evident maternal or foetal COMPROMISE Cat 4 = At a time acceptable to both woman & OT team "Based on objective evidence in relation to the newborn" DDI (Decision to Delivery Interval) - based on custom & practice. No DDI attached to categories by RANZCOG |
|
|
CTG Interpretation |
DR C BRAVADO DR - Determine risk (based on Hx & O/E - antenatal & intrapartum probs) C = Contractions, frequency (x: 10 min) BRA = Baseline rate - normal 110-160 V = Variability - normal 5-25 A = Accelerations - normal 15bpm for 15sec D = Decelerations: Early - head compression Variable - Cord compression +/- foetal hypoxia Late - foetal hypoxia Prolonged >2min - foetal hypoxia O = Overall impression
NB 1 square = 1min |
|
|
CTG - Features very likely assoc w foetal compromise |
* Prolonged bradycardia (<100 for 5min)
* Absent baseline variability * Sinusoidal pattern * Complicated variable decelerations w reduced baseline variability * Late decels w reduced variability |
|
|
CVS Changes in Pregnancy |
* Inc CO 30-50% (SV & HR)
* Dec BP (DBP > SBP) * Epidural venous congestion * Inc blood volume 25-40% -> dilutional anaemia * Inc fibrinogen * Inc coag factors -> hypercoag state * Dec oncotic pressure (blood volume > Inc total protein) |
|
|
Respiratory changes pregnancy |
* Capillary engorgement resp mucosa
* Inc minute vent 50% (TV > RR) * Dec FRC, RV & ERV after 20/40 * Inc O2 consumption 20% * Resp alkalosis + Dec HCO3- - minimal pH change * (R) shift ODC due to Inc 2,3-DPG |
|
|
GIT/Endocrine changes PRegnancy |
* Dec gastric emptying & motility
* Inc acid production * Dec barrier pressure * Placenta - pressure dependent flow, not autoregulated (~500-750ml/min at term) * Inc risk gallstones * Inc insulin & glucagon but impaired glucose tolerance |
|
|
Causes Maternal death - Australia |
DIRECT * AFE* HTN * VTE * Haemorrhage * Cardiac disease * Suicide * Infection |
|
|
Obstetric Arrest - Points of difference |
* Perimortem caesarian delivery
* Rapid airway management * Lateral displacement of the uterus * CPR & defib implications * Likelihood of non-cardiac causes |
|
|
Intra-uterine Foetal Resuscitation |
* Left lateral tilt
* O2 * Fluids (except severe pre-eclampsia) * Cease oxytoxics +/- give tocolytics (GTN/Mg/terbutaline) * Vasopressors GTN = 50mcg Terb = 250mcg SC Q20min Mg = 4g/20 min (same as PET) |
|
|
Cell salvage in obstetrics |
* Separate suction device from time of ROM to complete delivery of foetus & placenta
* Replacement of clotting factors as cell salvage -> dilution coagulopathy * Leukocyte depletion filters essential * Not for use in perineal or lower genital tract bleeding (infection risk) * Kleihauer testing essential (?only Rh-ve) |
|
|
Foetal monitoring GA for non-obstetric surgery |
Loss of variability normal |
|
|
Myotonic Dystrophy - Obstetrics |
* Temporary exec may occur 3rd TM, improve postpartum
* Inc risk of preterm labour * Care w nifedipine & MgSO4 * Resp & cardiac conduction defects * Airway issues, & inc aspiration risk * MYOTONIC CRISIS - warm room/pt; IV fluids; avoid six & shivering (not relieved by nerve blockade) * Generalised contracture -> dantrolene, phenytoin * Localised -> direct LA into muscle * Higher incidence of CS & PPH * Care w SA if resp compromise * GA - care w resp depressants; full reversal * Consider HDU post-op |
|
|
Multiple Sclerosis |
* Common onset child-bearing years
* Concern re: neurotox LAs - no evidence * Intra-op hypotension may be refractory to vasopressor therapy * Inc relapse rate post-partum regardless of anaes technique or mode of delivery |
|
|
Spina bifida occulta |
* Usually isolated bony defect - generally between L4-S2
* RA ok - perform block at site remote from region (as no posterior bone) * Inc accidental dural puncture risk * Inc failure/patchy block rise if epidural space is discontinuous * Those w cord anomalies often have cutaneous signs, & may be symptomatic * MRI - ?tethered cord |
|
|
Spina bifida cystica - Obstetrics |
* Either meningocele, or myelomeningocele (more common)
* RA may be technically difficult * Inc risk of dural puncture, incomplete block * SA - possible, low or tethered cord may inc risk of neural injury * NB Latex allergy
|
|
|
Obstetric Anaesthesia - approach to all neuro conditions |
Antenatal Ax Counselling Investigations - Imaging, RFTs etc Full baseline neuro Ax & documentation Post-partum follow-up |
|
|
Obesity & Pregnancy - Increased Risks |
Maternal: * Death or morbidity* CVS, resp disease, OSA * Recurrent miscarriage * PET * GDM; VTE * Inc LSCS; Prolonged surgical time; Post caesar wound infection * PPH * Stillbirth & neonatal death * Congenital abnormalities * Prematurity * RA - USS; needle choice; dural puncture * GA - Airway; Resp/OSA; pre-O2 & position; Aspiration; Multimodal analgesia; PNS |
|
|
Antacid Prophylaxis |
* Sodium Citrate - (0.3M) - effective w/i few minutes; DOA 1 hr
* Ranitidine - 50mg IV (onset 45min); 150mg po (1hr) - DOA 5 hrs * PPIs - no more effective, just expensive * Combo of ranitidine + Na citrate = best * Metoclopramide can inc gastric emptying * OBSTETRICS - use >14/40, & up to 18hrs post delivery (consider ranitidine in labour if high risk of requiring GA Q6H) |
|
|
PPH - Causes |
* Tone
* Tears * Tissue * Thrombin |
|
|
PPH - Mx |
* Consider MTP/Help
* Fluids/vasopressors * If GA -> TIVA * Massage fundus (except if retained POC) * Syntocinon bolus then infusion * Ergometrine 250mcg IV * Misoprostil 800-1000mcg PR * PGF2-alpha IM 500mcg * Surgical: - B-Lynch suture - Bakri balloon - Aortic compression - Internal iliac ligation (will cause ischaemia therefore -> hysterectomy) |
|
|
Neonatal resusc - Initial Ax |
* Estimation of gestation & APGAR
* Presence of meconium * Absent, difficult breathing * Absent muscle tone * Heart rate |
|
|
Neonatal resusc |
1. Warm, position, clear airway, dry & stimulate (unless meconium then suction trachea 1st)
2. If HR <100/inadequate breathing/not crying -> ventilate (5 breaths 30 2-3sec), then RR 40-60 (30cmH2O, preemie 25) - Use air & target SpO2 3. If HR <60, or not improving after 30sec -> CPR (3:1/2 sec) 4. If not improving: Venous access -> fluid (10ml/kg boluses); adrenaline Consider possible causes: * PTX* Congenital lung/heart problem * Sepsis * BGL * APH 5. If VT/VF -> 4J/kg every 2 min Amiodarone 5mg/kg Atropine 20mcg/kg for brady Adenosine if SVT 100mcg/kg |
|
|
Targeted SpO2 neonatal resusc |
1 min 60% 3 min 70% 5 min 80% 10 min 85% |
|
|
Suggested dose for caudal analgesia |
Bupivacaine 0.25% 1ml/kg Fentanyl 0.5mcg/kg |
|
|
Post neonatal resusc care |
* Arrange admission to NICU - keep intubated until in NICU & assessed
* Documentation of observations, interventions & times * Closely monitor fluid status & nutrition * Check BGL immediately following resusc & regularly * Consider ABs if sepsis possible Dx * Close monitoring of Temp * Communication w parents - early contact if possible * Debrief of staff * M&M |
|
|
Down Syndrome Associations |
* Atlanto-axial instability (20%)
* Airway - large tongue; OSA; subglottic stenosis (post-extubation stridor) - consider smaller ETT; awake extubation * CVS defects - ASD/VSD/TOF * GIT - TOF;GORD; Duodenal atresia * Vagal tone - prone to bradycardia (esp w high doses of sevo) therefore have atropine * Hypothyroidism (50%) * ALL * Difficult IV access * Behavioural * Epilepsy (10%) |
|
|
Polycythaemia consequences |
* Coagulopathy
* Intracranial abscess * Stroke * Hyperuricemia * Neurodevelopmental delay |
|
|
Canadian CT Head Rules |
CT for minor head injury patients (GCS 13-15) High Risk: 1. GCS < 15 at 2hrs post injury2. Suspected open or depressed skull fracture 3. Any sign of basal skull fracture 4. Vomiting >2 episodes 5. Age >65 6. Amnesia before impact >30min 7. Dangerous mechanism (pedestrian, ejection, fall from > 3 feet) |
|
|
Canadian CT head Rule - Exclusion Criteria |
* Non-trauma
* GCS < 13 * Age < 16 * Coumadin or bleeding disorder * Obvious open skull fracture |
|
|
Common Chemotherapeutic SEs: MTX (anti-metab) Vincristine (mitosis) Doxorubicin (antibiotic) Cyclophosphamide (alkylating) Bleomycin (antiobiotic) Fluorouracil/Mercaptopurine/Actinomycin Cisplatin (alkylating) Paclitaxel (anti-metabolite) Cyclosporin/Tacro (calcineurin inhibitors) Azathioprine (anti-metabolite) |
MTX - Pulm fibrosis; Myelosuppression; Stomatitis; Hepatoxicity Mycophenolate - Myelosuppression Vincristine - Neuropathies; SIADH; Myelosuppression Doxorubicin - Cardiomyopathy; Myelosuppression Cyclophosphamide - Prolonged NMB Bleomycin - Pulm toxicity Fluorouracil/Mercaptopurine/Actinomycin - Myelosuppresion Cisplatin - Peripheral neuropathy; Nephrotoxicity; GI upset; Myelosuppression Paclitaxel - Myelosuppression; Peripheral neuropathy; Arthralgia Cyclosporin/Tacrolimus - HTN; Renal tox Azathioprine - Liver; Pancytopenia |
|
|
Oxytoxics - SEs |
Syntocinon - Vasodilation & Hypotension; Tachycardia Ergometrine - Pulmonary vasoconstriction; HTN PGF2-alpha - Severe bronchospasm; HTN; Pulmonary oedema PGE2 - (Misoprostil) - vasodilation; nausea Carbeprostin - (100mcg) - Synthetic long acting oxytoxin
|
|
|
Indications Peri-operative TOE |
* Class I - Cardiac surgery - valve repair; CHD; aortic dissection/aneurysms; HOCM; Endocarditis
* Class IIa - emergency use in non-cardiac surgery w persistent haemodynamic instability ?cause * Class III (no benefit) - routine use to screen or monitor for ischaemia during non cardiac surgery w/o risk factors * Intra-op emboli monitoring |
|
|
Brice Questionairre |
1. What was the last thing you remembered happening before you went to sleep?
2. What was the first thing you remembered happened on waking? 3. Did you dream or have any other experiences whilst you were asleep? 4. What was the worst thing about your operation? 5. What was the next worse thing? |
|
|
Types of awareness |
EXPLICIT = Conscious recollection of events, either spontaneously or as a result of direct questioning IMPLICIT = memories exist without conscious recall but they can alter patients' behaviour after the event |
|
|
Sequelae of awareness |
* Anxiety
* Fear of surgery * Sleep disturbances * Nightmares * Flashbacks * PTSD * Depression |
|
|
Signs of awareness |
* HTN
* Tachycardia * Lacrimation * Pupillary dilatation * Diaphoresis Beware lots of drugs can alter above signs (BB; opioids; anti-cholinergics; CCB; ACE-I) |
|
|
Awareness RFs |
PATIENT: * Past history* Chronic opioid or BDZ/substance abuse * DI * Limited CVS reserve * Cardiac * Trauma * GA LSCS * Rigid bronch (TIVA & NMBD) * TIVA * NMBD |
|
|
Indications resynchronisation therapy |
(Class I) - With systolic HF and: * LVEF = 35%* LBBB * QRS >150ms * NYHA >II symptoms * Sinus rhythm |
|
|
Definition STEMI |
New ST elevation at the J point in at least 2 contiguous leads of ≥2 mm (0.2 mV) in men or ≥1.5 mm (0.15 mV) in women in leads V2–V3 and/or of ≥1 mm (0.1 mV) in other contiguous chest leads or the limb leads |
|
|
CHADS-VASC Score |
* CHF
* HTN * Age >75 (2 points) * DM * CVA/TIA/TE (2 points) * Vascular disease (prior MI, PVD or aortic plaque) * Age 65-74 * Sex - Female Max score = 9 Score = 0 -> no therapy = 1 -> anticoag or anti-plt >/= 2 -> oral anti-coagulation |
|
|
Indications MRI C-spine - Trauma |
*
Post traumatic cervical myelopathy/radiculopathy * Clinical symptoms unexplained by other radiologic studies * Assess ligamentous injury * Possible disc herniation |
|
|
HAS-BLED score |
* HTN (SBP >160)
* Abnormal renal (>200) or liver fx (1 point each) * Stroke * Bleeding tendency * Labile INRs (<60% time in therapeutic range) * Elderly (>65) * Alcohol or drugs (anti-plt; NSAIDS) |
|
|
How to test supraclavicular block |
PUSH-PULL-PINCH-PINCH
Push = elbow extension = Radial Pull = elbow flexion = MC Pinch = hypothenar eminence = Ulnar Pinch = Thenar eminence = Median |
|
|
DAS Extubation Guidelines |
1 - Plan extubation 2 - Prepare for extubation 3 - Perform extubation 4 - Post-extubation care: recovery & F/U |
|
|
At risk airway for extubation |
Airway RFs * Pre-existing airway difficulties - OSA; DA; aspiration risk* Peri-op airway deterioration - oedema; bleeding * Restricted airway access * CVS instability; impaired resp fx; neuro/NM impairment; T; electrolyte * Type of surgery - smooth emergence may be desirable |
|
|
Preparing for Extubation |
Optimise Pt suitability, Assess Risk & Stratify 1. Upper airway - is BMV achievable?2. Larynx - cuff-leak test 3. Lower airway - may require CXR 4. Other e.g. gastric distension 5. If rescue involves subglottic access - should have access to neck 6. NM block should be fully reversed (TOFR >0.9) 7. Ensure adequate analgesia 8. CVS stability 9. Optimise fluid status, T, pH, electrolyte & coag status |
|
|
Paediatric C-spine imaging criteria (APLS) |
* Unconscious w suspected spinal injury
* Posterior midline spinal tenderness * Focal neurological deficit or pain * Sedative drugs * Painful distracting injury * Reduced mental state |
|
|
Trigeminal neuralgia diagnostic criteria |
* Paroxysmal attacks of facial or frontal pain
* No neurological deficit is present * Pain has at least 4 of following characteristics: - Distribution along one or more divisions of CNV - Sudden, intense, sharp, superficial, stabbing or burning in quality - Severe pain intensity - Precipitation from trigger areas (e.g. brushing teeth) - No symptoms b/n paroxysms
Need to exclude tumours e.g. acoustic neuroma/Mets & MS Rx w best evidence = carbamazepine (SE - agranulocytosis; S-J syndrome) |
|
|
Hyperkalaemia in Paed |
* ?Arrhythmia -> Calcium 0.1mmol/kg IV
* Nebulised salbutamol * Repeat K - resonium if falling * If remains high -> Ax pH: - pH <7.35 -> NaHCO3 1mmol/kg - pH >7.35 -> glucose 10% 5ml/kg + insulin 0.05U/kg/hr |
|
|
Paed BLS & ALs |
Same except: * CPR 15:2* Shock 4J/kg * Adrenaline 10mcg/kg * Amiodarone 5mg/kg (if VT w no shock -> over 1-4hrs) * Adenosine 100/200/300mcg/kg * Sync shock 1J/kg/2J/kg |
|
|
Intra-arterial Injection Drugs |
* Presentation - Intense burning pain; blanching
* Immediate action - Stop injection but leave cannula in situ; 1% lignocaine 5ml; Papaverine 40mg; Flush w heparinised saline * F/U - Regional symp blockade; anti-coagulation; refer to vascular (we don't have admitting rights, |
|
|
Mediastinoscopy |
* Assessment - Obstruction; Position of comfort
* Ix - Imaging (degree & length of obstruction); How small is the trachea (inc complications * Prep - have rigid bronch available; Large bore IV/XM; Jet vent; 20 deg head up (venous); PNS (avoid NMBD in MG) * Plan A - Spont breathing; Spray cords; Direct laryngoscopy - ETT * Plan B - Smaller tube * Plan C - Rigid bronch * If surgeons ask for paralysis - have suggamadex available, test ventilate (as can still obstruct past the ETT) * Thyroid - often compliant can push tube past it * Other options - rigid bronch on standby |
|
|
Dose Neostigmine & atropine paed |
* 50mcg/kg neostigmine
* 20mcg/kg atropine * Put 2.5mg neostigmine |
|
|
Pyridostigmine to Neostigmine conversion |
30:1 Pyridostigmine - usually Q3H dose e.g. 120mg pyridostigmine - rarely exceeds this If a long case - need replacement. 4mg neostigmine over ?time of pyridostigmine |
|
|
Performing High risk Extubation |
Is it safe to extubate? No - Consider postponing; or Tracheostomy Yes - Options: Awake Advanced manoeuvres - Remi; LMA exchange; Airway exchange catheters
|
|
|
Aintree Catheter |
ID 4.7mm (so need 4.5mm bronch or smaller) ED 6.3mm |
|
|
Bronchoscopy Sizes |
General 6mm Diagnostic 4.2mm Paed 3.6mm |
|
|
LMA Sizes & ETT |
LMA 3/4/5 ETT 6.0/6.0/7.0 |
|
|
Limits Mannitol & Hypertonic Saline |
Osm < 330 Na < 155 |
|
|
AFOI Indications |
* Anticipated difficult airway without airway obstruction - as assessed pre-op
* Previous difficult airway or AFOI * Previous difficulty in mask ventilation * To avoid iatrogenic injury e.g. unstable C-spine |
|
|
Cerebral Perfusion Monitoring |
Awake patient Stump pressure (CEA) - ischaemia rarely occurs at > 60mmHg (High FP rate ->unnec shunts) NIRS - Change in oximetry is best measure (>20%); Normal value 60-80% (venous) - <40% significant hypoxia SjVO2 - Initiate Rx if <50% (global not focal ischaemia) EEG - changes at SjO2 <40% SSEP - global - cortical only? TCD - alone or w EEG - useful for detecting micro emboli |
|
|
Definition of Difficult Airway |
ASA (one or all): * Difficulty w mask ventilation* Difficulty in supraglottic device ventilation * Difficulty in tracheal intubation (grade 3 or 4) * >2 attempts at intubation w direct laryngoscopy * Or using adjuncts * Or using an alternative device or technique |
|
|
Contraindications AFOI |
* Lack of airway skills
* Difficult airway w impending airway obstruction * Allergy to LA * Infection/contamination of upper airway - blood/friable tumour, open abscess * Grossly distorted anatomy * Fractured BOS (nasal route) * Penetrating eye injuries * Pt refusal or uncooperative pt |
|
|
Paediatric Laryngoscopy blade sizes |
Neonate-6 months -> 0 (Miller straight or Macintosh) 6-9 months -> 1 1-4yrs -> Mac 2 >4 -> Mac 2 or 3 |
|
|
PTSD S&S |
* Intrusive thoughts (flashbacks, or reoccurring pain, or dreams)
* Avoidance (of any experience that reminds them of traumatic event) * Hyperarousal (panic attacks, anxiety) |
|
|
Coronary Anatomy |
Dominance - which vessel supplies PDA (supplies AV node) 80% RCA LMCA: * Bifurcates to LAD & LCx* LAD - Anterior-lateral wall of LV; Septum * LCx - (obtuse marginal) - several atrial branches, & SA (40%) * RVOT & SA (60%) * Branches to PDA |
|
|
CP Implications |
* CNS - IQ/anxiety/pain Ax/Epilepsy
* Resp - Aspiration/spinal deformity/Dec immunity -> chronic disease -> restrictive pattern & pulm HTN * GIT - Malnutrition/anaemia/dehydration * Airway - TMJ dislocation (spasticity) * Msk - FFD/osteopenic/Sux is ok/likely difficult IV access * Meds - anti-convulsants/anti-spasmodics (withdrawal) * CVS - adult IHD high * Pre-med - anxiety & anti-sial * Consider other meds * Good analgesia * Care with positioning * Actively warm & T monitor * Extubate left lateral * May need HDU resp * Reinstitute diet & meds |
|
|
Children - OSA higher risk after anaesthesia |
* Age < 2yo (esp <1)
* Airway surgery (esp T&A) * Facial abnormality w reduced oropharyngeal size * Severe OSA on polysomnography
If need a premed - reduce dose (e.g. midas 0.3mg/kg) |
|
|
Pre-med dose & peak effect Paed |
Midazolam - 0.3-0.5mg/kg orally; 0.2mg/kg intra-nasal; Peak 20-30min; bad taste (max 15mg) Clonidine - 4mcg/kg; Peak 60-90min Ketamine - 5mg/kg oral (may produce unconsciousness/airway obstruction); IM 1-2mg/kg (through clothing if need be!) |
|
|
EtSevo required for intubation (paed) |
4% N2O & fentanyl reduces this |
|
|
Post-extubation Stridor Rx |
* Give dex if concerned obstruction will worsen
* Neb adrenaline if significant obstruction |
|
|
Adrenaline Concentrations |
1:10000 = 0.1mg/ml (mini-jet) 1:1000 = 1mg/ml (in our trolley) |
|
|
Recovery Scores for Discharge |
Scoring systems e.g. modified Aldrete or Steward score - components: * A - Maintaining airway* B - Acceptable O2 saturation * D - Conscious; Good pain control & not agitated |
|
|
What is stridor? |
Results from turbulent flow in larynx or lower in bronchial tree - caused by narrowing of airway
|
|
|
Nasendoscopy - Anatomy |
Epiglottis VC Arytenoids - posterior to VC Ary-epiglottic fold - b/n epiglottic & arytenoids Pyriform fossa - posterior & lateral to A-E fold
Posterior cricoarytenoid muscles - abduct VC (RLN - CN X) |
|
|
Level II Check Components |
* Service label present
* O2: * Vapourisers - full; power on for Des; seated ok; leaks (occlude circuit & APL 30 - wait for 30sec & check pressure has increased to 30 or more) * Circuit - assembly; high pressure leak; low pressure; valves & APL; manual ventilation * Ventilator - alarms; bellows; self-inflating bag * Scavenging; Suction; Laryngoscopes; Monitoring * Other - drugs; IV; pumps; power |
|
|
Uraemia - Causes, S&S |
Causes: * Pre-renal - hypotension; shock; CCF; dehydration; Increased production in liver (high protein diet); Increased production - protein catabolism (stress; fever; steroids; GIT haemorrhage; Tumour lysis - LD)* Renal failure * Post-renal - calculi; bladder or prostate tumours * Confusion/Fatigue * Anorexia/N&V * Cramps * Anaemia * Platelet dysfx * Pericarditis/HTN * Itch |
|
|
Chronic Renal Failure - Calcium & Ph |
1. Dec GFR -> Inc Phosphorus -> * Direct stimulation PTH* Mild hypoCa due to precipitation (CaHPO4) * Stimulation FGF-23 -> inhibits Vit D 2. Dec GFR -> Dec calcitriol (dec renal conversion of 25-Hydroxyvitamin D3 -> 1,25-Hydroxy/Calcitriol) 1 and 2: -> Secondary hyperparathyroidism -> Bone disease PTH -> Ca & Ph release from bone
|
|
|
IVRA: Dose Prilocaine & Lignocaine Equipment Other points |
* Avoid risks of GA
* Need purpose designed double cuff - pressure displayed & will maintain inflation if no electricity * Width of cuff = 20% more than upper arm diameter * Pressure SBP + 50 * Prilocaine: * Release - warn patient, monitoring, fluid bolus, vasopressors available |
|
|
Dose intralipid LAST |
* 20% 1.5ml/kg bolus, then 15ml/kg/hr infusion
* Increase 30ml/kg/hr if CVS not restored * Max dose 12ml/kg * Conventional ALS protocol * Post care - blood for analysis; ICU; Lipase daily for 2 days (exclude pancreatitis) |
|
|
Epidural Space lumbar vs thoracic |
* Epidural space - potential space, roughly triangular
* Anterior dura - heavily innervated * Thoracic ~2mm (posterior epi. border to dural sac) * Lumbar ~5mm * LF thinner & softer * T1-4 - cardioaccelatory fibres |
|
|
Epidural Blood patch - advice post |
1. not to carry anything heavier than the baby for 2-3 weeks, |
|
|
Levels block needed for LSCS |
* Uterus T10
* Peritoneum T4 * Incision T12-L1 * Bladder ?T10 |
|
|
Innervation penis & Block (paed dose) |
* Root - Ilioinguinal L1
* Remaining - Pudendal S2-4 * Block dorsal nerve w paired injection above root of penis, deep to Buck's fascia * Touch pubic bone - redirect 5-10 deg caudally, & 10-20deg each side * Avoid injecting into Bucks (as vein & arteries are there) * KIDS dose - 0.5% bupivacaine - ml = age +1 (i.e. neonate 2ml) * Adult dose - 10ml * Aspirate & don't inject in midline (superficial dorsal vein & other vessels deeper) |
|
|
TAP Anatomy & Dose |
* T6-L1 anterior rami
* Run in plane b/n IO & TA * 2 branches: * L1 - Ilioinguinal & Iliohypogastric (part of lumbar plexus) * Dose - 20ml 0.375% each side
|
|
|
Lumbar plexus |
T12 - L4 - I twice Get Laid On Fridays Iliohypogastric - L1 Ilioinguinal - L1 Genitofemoral - L2-3 Lateral Fem cut - L2-3 Obturator - L2-4 Femoral - L2-4 |
|
|
Sacral Plexus |
L4-S4 SIPPS * Superior gluteal - 451* Inferior gluteal - 512 * Posterior cutaneous - 123 * Pudendal - 234 * Sciatic - L4-S3 - 10% separate earlier than popliteal fossa |
|
|
Block Saphenous |
* For supplementation sciatic
* ~10cm above knee medially - probe transverse plane * Vastus medialis (anterior) & sartorius * Deposit LA behind sartorius - field type block * 20ml 0.2% ropivacaine |
|
|
Most peripheral blocks - needle & dose |
10cm 22G stimuplex needle 15-20ml 0.2-0.375% ropivacaine |
|
|
Specifics of Primary Survey |
Airway & C-spine Breathing - RR/SpO2; Exposure; Asymmetry; Crepitus; Surg emphysema; Percuss/auscultate; Trachea (log roll to look at posterior chest if concerned); May need needle/finger thoracotomy or ICC Circulation - BP/HR; Cap refill; Bleeding sources - SCALP; 2x large bore IV; bloods inc XM; ABG/VBG; 1-2L crystalloid, then blood (paed - 20ml/kg) Disability - GCS; pupils; gross motor & sensory; Priapism; PR (if suspect spinal injury); GLUCOSE; Prevention of Secondary injury/ICP Mx Exposure/Environment - T; Expose; Log roll if not already done |
|
|
Damage control resusc |
MAP > 65 & good perfusion -> sit tight MAP >65 & poor perfusion -> give fentanyl 20-25mcg (take away fear & pain) & vasodilator - then give products/fluid to bring MAP to >65 MAP <65 -> give products |
|
|
Changes after cardiac death |
Cushings - HTN Catecholamine storm Hypotension/Myocardial dysfunction Pulmonary oedema Endocrine dysfunction - loss of HPA axis |
|
|
Brain Death Drugs |
Fluids/Norad T3; Methylpred; ddAVP
|

