![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
Gram + Staphylococci produce ________
what are the three major medically important staphylococci? |
catalase
S. aureus, S. epidermidids, S. saprophyticus |
|
|
where is S. aureus carried in 30% of the population? |
anterior nares
(also common on body skin & perineum) |
|
|
If someone contracts S. aureus in the hospital, what is the most likely source? |
medical personnel
(resistant to drying, reinfection common) |
|
|
which staphylococcus is sensitive to novobiocin? which is resistant? |
sensitive: epidermidis
|
|
|
which member of the staph family is more likely to cause prosthetic infections? UTI's in young sexually active females? Osteomyelitis & septic arthritis? |
prosthetic: epidermidis |
|
|
what two pathogens create biofilms?
what can they cause due to their ability to create biofilms? |
strep viridans and staph epidermidis.
Both can cause subacute bacterial endocarditis. |
|
what is antigenic and relatively specific for S. aureus (contained in the cell wall of S. aureus)? |
ribitol-Teichoic acid |
|
|
what is S. aureus's virulence factor that binds to the Fc portion of IgG molecules? |
Protein A |
|
|
what is the function of Protein A? |
blocks Fc binding to Fc receptor on phagocytes, preventing phagocytosis |
|
|
what is the pathogenesis of osteomyelitis via staph aureus? |
1) colonization: via adhesins (bind to laminin, fibrinonectin, etc) |
|
|
What toxins does S. aureus release? |
alpha-toxin exfoliatin PTSAgs (Pyrogenic Toxin superantigens) Staphylococcal enterotoxins (GI disturbance) TSST-1 (toxic shock syndrome toxin) |
|
|
Which toxin in only produced by S. aureus (coag pos staph)? What does it do? |
alpha-toxin
creates transmembrane pores (allows other molecules to be released into cell) |
|
|
what is the function of exfoliatin?
|
works between stratum spinosum and stratum granulosum causing intracellular splitting of the epidermis (detaching) causing global denutation. |
|
|
why are (PTSAgs & TSST-1) superantigens called superantigens? |
bc the superantigen binds outside the MHC molecule & outside of the V-beta region of the T cell. Therefore the specificity is loss they can bind to anything. This will cause a mass proliferation of inflammatory cells- IL-1, TNF-alpha. = induce toxic shock syndrome |
|
|
what is the difference between the triggering points of gram negative shock and toxic shock syndrome? |
gram negative shock is triggered by LPS (ie all the inflammatory cytokines are induced by the LPS).
|
|
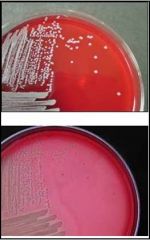
What organisms show beta-hemolysis on sheep blood agar? |
Staphylococcus sp. Streptococcus sp. (groups A & B) |
|
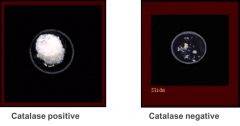
The catalase test can be used to differentiate btwn staph & strep, which will be +? |
Catalase enzyme is produces by staphyloccus sp ONLY |
|
|
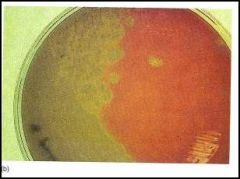
ONLY staph aureus ferments on what medium? what color does this medium turn? |

mannitol salt agar. Turns from red to yellow. |
|

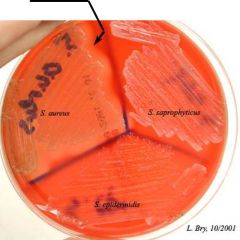
what are the coagulase negative staphylococci? |
s. epidermidis and s. saprophyticus
(only S. aureus will be coag positive) |
|
|
How does coagulase work?
|
it breaks down fibrinogen to fibrin making a mechanical barrier around it which allows it to evade phagocytosis. |
|
|
How can you differentiate btwn the two coagulase negative staphs (s. epidermidis & s. saprophyticus)? |
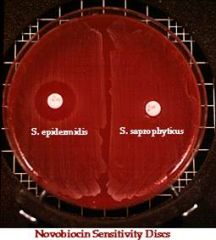
Novobiocin discs
zone of inhibition= sensitivity= S. epidermidis
no zone= resistance= S. saprophyticus |
|
|
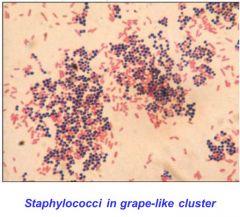
S. Aureus diagnosis: |
*Microscope: Gram + cluster of grapes (purple) *Blood agar: overnight growth *Catalase Test: Positive Coagulase: Positive Mannitol=salt agar: red--> yellow, mannitol fermenting
(* these are same for all staph) |
|
|
S. aureus was initially treated w/ penicillin, but developed resistance via _______________ |
penicillinase or beta-lactamase
^ breaks down penicillin by opening the beta-lactam ring & preventing drug action |
|
|
what is the mechanism of penicillin resistance?
|
chromosome (G) mediated- coating of beta lactamase enzymes |
|
|
how does penicillin inhibit cell wall synthesis? |
by binding to transpeptidases (penicillin binding protein,PBP) |
|
|
what is the function of transpeptidase?
|
catalyze the crosslinking of peptidoglycans |
|
|
T/F |
true |
|
|
A semi-synthetic penicillin, methicillin, was created to treat penicillin resistant s. aureus.
How did S. aureus then become methicillin resistant S. aureus or MRSA? |
S. aureus acquired a gene encoding for a different type of transpeptidase (PBP), with a reduced affinity for the beta-lactam antibiotics (penicllin & methicillin can no longer bind PBP), thus allowing cross-linking |
|
|
what is the mechanism of MRSA?
|
plasmid mediated transduction |
|
|
what is the DOC for tx of MRSA? what problem is arising? |
vancomycin; vancomycin resistant MRSA. |
|
|
what does vancomycin directly bind to? what does it inhibit? |
terminal AA side chain (NOT PBP) *it inhibits the crosslinking of peptidoglycans, PBP cannot bind to side chain |
|
|
what is vancomycin resistance?
|
when the terminal chain of the AA is changed and vancomycin can't bind. |
|
|
how is multidrug resistance acquired?
|
via plasmid mediated transposition which involves the transposon |
|
|
what do you give a patient who is methicillin sensitive? |
nafcillin or oxacillin |
|
|
what do you give a pt who is methicillin resistant? |
vancomycin |
|
|
What do you give pt who is methicillin AND oxacillin resistant? |
Linezolid or Levoflaxacin + rifampin |
|
|
what do you give a pt who is vancomycin resistant? |
streptogramin (dalfopristin and guinupristin in combo) or Daptomycin |
|
|
After Staph Aureus what is the 2nd MC cause of ALL osteomyelitis? |
strep. Pneumonia |
|
|
what pathogen causes osteomyelitis after trauma or surgery? |
Group strept A (s. pyrogenes) |
|
|
what causes osteomyelitis in neonates? |
S agalaciae (GBS) |
|
|
what causes osteomyelitis in older infants, children and adults? |
S. viridans |
|
|
what causes osteomyelitis in pts with hemolytic disorders? |
S. Viridans |
|
|
what are the three types of streptococci that are lancefield antigens?
ALL of these organisms are involved in _________ |
S. pyogens, S. agalactiae, S. pneumoniae
osteomyelitis |
|
Which sp. are beta-hemolytic streptococci? |
Group A strep: S. pyrogenes & Group B strep: S. agalactiae
(staph are also beta-hemolytic) |
|
|
Which streptococcus is bacitracin sensitive? |
Group A Streptococcus |
|
|
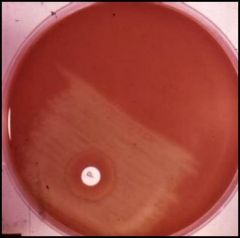
what is the confirmatory test for group B streptococcus? |
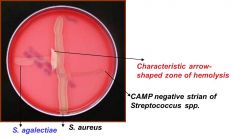
CAMP test
(*characteristic arrowhead = CAMP +) |
|
which sp. are alpha-hemolytic (partial hemolyisis) streptococci? |
S. pneumoniae & S. viridans |
|
|
how do you differentiate s. viridans from s. pneumonia? |
optochin disc. Pneumonia is sensitive to optochin.
*or bile test, pneumonia is autolytic & bile will become clear= + result* |
|
|
what is the only gram positive diplococci?
(ALL strep are gram positive) |
S. Pneumoniae
(s. agalactiae & S. pyrogenes are both arranged in chains) |
|
|
what virulence factors of streptococcus binds to surface molecules like fibronectin? |
Protein F, M protein and Lipoteichoic acid |
|
|
what is the essential virulent factor for streptococcus pyogenes? what does it do? |
M protein; it degrades C3b (an opsonin) and allows evasion of phagocytosis. |
|
|
what is serotype detection used for?
what protein is essential for this serotyping? |
difference between pyogenes and pneumoniae (streptococcal).
M protein |
|
|
what strain of M protein causes post streptococcal glomerulonephritis?
|
M12 |
|
|
Rheumatic fever is a complication of ___________.
It occurs when pathogenic Ags cross-react w/ antigenic epitopes on cardiac & joint tissue.
how do you confirm the diagnosis of rheumatic fever? |
group A strep (pyrogenes) pharyngitis
if the pt has either 2 major criteria conditions or one major and 2 minor criteria. |
|
|
what is included under the major criteria for Rheumatic Fever? |
carditis (mitral & aortic valve damage) arthritis, chorea, subcutaneous nodules, erythema marginatum |
|
|
what is included under the minor criteria for Rheumatic Fever? |
fever, joint pain, electrical changes in the heart, presence of certain proteins in the blood. |
|
|
Rheumatic fever tx: |
Tx Strep: Penicillin-G + 5 yr maintanence dose + any symptoms; Pain & inflammation: Aspirin Carditis: steroids Chorea: Diazepam or haloperidol |
|
|
__________ also contains Lancefield antigen (D) & was previously referred to as Strep group D, gamma-hemolytic (no hemolysis)
|
enterococcus |
|
|
which pathogen is a normal intestinal/genitourinary flora that is able to withstand high bile and salt? |
enterococci
*thus infection occur after procedures involving these areas |
|
|
what are the 2 common enterococci species |
E. faecalis E. faecium |
|
|
what is the medium of choice for enterococcus growth? |
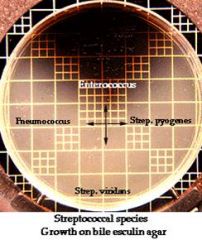
bile esculin agar
** no other bacteria can survive on this, turn agar BLACK! |
|
|
where do you usually encounter enterococcal infections? |
hospital settings
|
|
|
three pathogens can cause subacute endocarditis, what are they?
|
strept viridans, staph aureus, and enterococcus |
|
|
Enterococci are responsible for nosocomial-UTIs Intra-abdominal infections Blood stream infections & Osteomyelitis due to ______________ |
osteomyelitis due to contaminated open wound & prosthetic joints |
|
|
T/F |
TRUE |
|
|
what are the agents of choice for minor enterococcus infections? |
penicillin and ampicillin (PARADOXICAL)
(*major infections= penicillin + vancomyocin) |
|
|
An elderly man is suspected to have BPH. After undergoing an exploratory cystoscopy he comes down with bacteremia resulting osteomyelitis (or endocarditis). What is the likely pathogen responsible? |
Enteroccoci |
|
|
Osteomyelitis following clenched-fist bite wound of the proximal phalanx is indicated by...... |
-concurrent bone erosion & subperiosteal bone deposition (found on x-ray) & -discharging sinus on dorsum of proximal phalanx |
|
|
what pathogen can cause osteomyelitis following a dog or cat bite?
what about human bites? |
Pastruella multicolor;
kingella kingae & eikenella corrodens |
|
|
Both K. Kinage & E. corrodens are ________ positive |
oxidase |
|
|
how do you differentiate kingella kingae from einkella corrodens? |
einkella corrodens has lysine decarboxylase and ornithin decarboxylase.
Kingella kingae does not. |
|
|
when ornithine is present in the medium, what color does the solution change?
|
ornithine: purple = Einkella |
|
|
what type of selective media is helpful for recovering kingella kingae? |

a selective media containing clindamycin or vancomycin
*short gram - rods w/ square ends |
|
|
what makes Kingella kingae different from all the other kingella's? |
it's beta-hemolytic |
|
|
what does a mature colony of Eikenella corrodens grow on? what color will it be? |
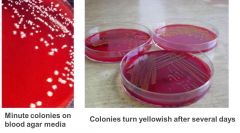
grows on blood & chocolate agar, requires hemin for growth
yellow in-grown colonies |
|
|
Why does Eikenella corrodens smell like bleach? |
produces hypochlorite
|
|
|
Eikenella produces gram - rods, that may twitch, on what type of selective medium? |
selective medium containing clindamycin |
|
|
both Einkella corrodens and Kingella Kingae are susceptible to what?
However, due to slow growth, bites are usually tx w/ what while waiting to identify the organisms? |
B-lactam antibiotics, tetracycline and quinolones
3rd-generation cephalosporin |
|
|
In addition to osteomyeltis, what else do Einkella infections cause? |
septic arthritis endocarditis |
|
|
Einkella corrodens & what kingella species are part of the HACEK group of atypical endocarditis orgnanisms? |
Kingella dinitrificans |
|
|
HACEK group (E. corrodens & K. dinitrificans) are the most common cause of gram - endocarditis in _______________ |
non IV drug users
(HACEK organisms are all in the oral cavity) |

