![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
1.what level of thoracic spine has the smallest spine canal diameter 2.which vertebrae as the narrowest of all pedicle diameter in the body? 3.which vertebral body as the shortest pedicle?
|
1.T4 2.T4 3. T4
|
|
|
#1 which erector spinae muscle is most medial and which is most lateral? |
#1 spinalis muscle & iliocostalis muscle |
|
|
In the adult spine, which of the following pedicles have the smallest average transverse diameter. 1. T1 2. T6 3. T12 4. L3 5. L5 |
Of the levels listed, T6 has the smallest pedicle diameter. Ans2 |
|
|
what genetic factors related 2 collagen production play a roll and anterior cruciate ligament injuries? |
COL5a1 gene |
|
|
what is the primary role of the anterior cruciate ligament |
to prevent anterior translation of the tibia relative to the femur |
|
|
what is the insertion of the anterior cruciate ligament |
in the RIGHT knee the anterior cruciate ligament originates from the lateral femoral condyle inserts just anterior to the intercondylar eminence of the tibia |
|
|
|
|
|
the predominant collagen type in anterior cruciate ligament is? |
type I collagen |
|
|
patient presents with he felt a pop and had immediate swelling physical exam effusion and quadriceps avoidance gait
It was diagnosis? #2 pathognomonic finding for anterior cruciate ligament on x-ray |
#1 anterior cruciate ligament tear |
|
|
if the femoral tunnel is to anterior what is leading to inside the knee? |
tight in flexion and loose in extension |
|
|
if the tibial tunnel placement is to anterior was the effect of the knee |
tight in flexion with impingement in extension |
|
|
what are the 2 most common complication with bone patellar bone autograft What is the maximum load to failure of a quadricep hamstring autograft? |
#1 patella fracture and #2 patellar tendon rupture |
|
|
reported to most common complications with quadricep hamstring autograft? |
windshield wiper effect and residual hamstring weakness |
|
|
what are the most common complications with allograft anterior cruciate ligament reconstruction? |
risk of disease transmission such as HIV and hepatitis, increased risk of rerupture and athletes, and if the graft was radiated decrease structural and mechanical properties of the graft |
|
|
what is the best determinant and skeletal maturity and female |
onset of menarche |
|
|
what are the most common complications with pediatric anterior cruciate ligament reconstruction |
increase 5 so injury due to increased tunnel diameter greater than 8 mm, high-speed reaming, interference screw fixation, oblique tunnel positioning |
|
|
contraindication with revision anterior cruciate ligament reconstruction? |
review harvesting bone patella bone |
|
|
during rehabilitation after an anterior cruciate ligament reconstruction what are the immediate treatments that are most beneficial? |
aggressive cryotherapy ice, immediate weightbearing, early full passive extension |
|
|
what exercises during postop anterior cruciate ligament reconstruction should be avoided? |
isokinetic quadricep strengthening and open train quadricep strengthening |
|
|
most effective oriented female athlete to prevent anterior cruciate ligament injury |
?neuromuscular training M PAULY metric jump training with the goal of increasing hamstring strength to decreased quadriceps dominance ratio |
|
|
most common reason for anterior cruciate ligament failure? |
surgical technique after most commonly improper tunnel placement with most commonly vertical femoral tunnel leading to rotational instability and positive pivot shift |
|
|
most common organism and anterior cruciate ligament reconstruction infection |
?staph aureus perform immediate joint aspiration with Gram stain and cultures and then do immediate arthroscopic I and D and may retain graft if multiple I and D's and antibiotics for 6 weeks |
|
|
most common nerve irritation after anterior cruciate ligament reconstruction? |
saphenous nerve |
|
|
most common complication the results and reoperation of an anterior cruciate ligament reconstruction? #2 most common complicationat 8-12 weeks postop after an anterior cruciate ligament reconstruction? |
improper tunnel placement |
|
|
A patient develops infrapatellar contracture syndrome after undergoing ACL surgery. All of the following findings are consistent with this diagnosis EXCEPT? 1. Patella infera 2. Decreased patellar mobility 3. Loss of active but not passive flexion 4. Loss of full extension 5. Loss of passive flexion |
Answer #3 which is incorrect because the resulting stiffness affects both active and passive motion. |
|
|
A 25-year-old male is one year status post anterior cruciate ligament (ACL) reconstruction using patellar bone-tendon-bone (BTB) autograft. He complains of persistent instability with certain activities. His operative dictation notes excellent stability intra-operatively with femoral fixation at the 12 o'clock position. Based on his femoral tunnel position, his history and examination are most likely to reveal which of the following? 1. Positive pivot shift test and instability with cutting activities due to failure to reconstruct the posterolateral bundle of the ACL 2. Positive Lachman's test and instability with forward running activites due to failure to reconstruct the anteromedial bundle of the ACL 3. Positive pivot shift test and instability with cutting activities due to failure to reconstruct the anterolateral bundle of the ACL 4. Positive Lachman's test and instability with forward activites due to failure to reconstruct the posteromedial bundle of the ACL 5. Positive pivot shift test and instability with forward running activities due to failure to reconstruct the posterolateral bundle of the ACL |
ACL reconstruction with 12 o'clock femoral fixation would lead to a vertically placed graft and result in continued instability with cutting activities, and a positive pivot shift exam due to failure to reconstruct the posterolateral bundle of the ACL. Current standards for anatomic ACL reconstruction stress the importance of more horizontal graft placement (10:30 in a right knee vs 1:30 in the left knee), to try and reconstruct both the anteromedial bundle which provides anterior-posterior stability, and the posterolateral bundle which provides the rotational stability. Improper femoral graft placement is one of the most common reasons for ACL revision surgery.ans1 |
|
|
At what range of motion do seated leg extension exercises place the greatest amount of stress on the anterior cruciate ligament? 1. 0 to 30 degrees 2. 30 to 60 degrees 3. 60 to 90 degrees 4. 90 to 120 degrees 5. flexion greater than 120 degrees
|
Open chain leg extension exercises cause the most anterior shear stress that would affect the ACL. The Wilk article summarizes that isotonic closed kinetic chain exercises produced significantly greater compressive forces compared to the open kinetic chain knee extension. In addition, during closed kinetic chain exercises, a posterior shear force (PCL stress) was generated throughout the entire range with maximal shear occurring from 85° to 105° of flexion. During knee extension, there is an anterior shear force (ACL stress) from 38° to 0° and a posterior shear force from 40° to 101°. According to Beynnon, a closed chain program results in anteroposterior knee laxity values that are closer to normal, and earlier return to normal daily activities, compared with rehabilitation with an open chain program. |
|
|
During anterior cruciate ligament reconstruction, a graft that is tight in flexion but lax in extension may be due to which technical error? 1. Femoral tunnel is too posterior 2. Femoral tunnel is too anterior 3. Femoral tunnel placed at 12:00 position 4. Tibial tunnel is too anterior 5. Tibial tunnel is too medial
|
The majority of early ACL reconstruction failures are felt to be due to errors in surgical technique. The most common error in ACL reconstruction is aberrant tunnel placement. The femoral tunnel can be placed too anteriorly, thereby causing increased strain on the graft in flexion because of the cam effect of the femoral condyle which can result in graft stretching, laxity in extension, and subsequent failure. Chhabra et al. performed a cadaveric study to demonstrate the anatomic footprints of the anteromedial and posterolateral bundles of the ACL. Markhof et al. performed a cadaveric study analyzing the effects of aberrant placement of the femoral tunnel. Illustration A is a table demonstrating the effects of tunnel malposition. Illustrations B and C are gross anatomy illustrations of normal ACL anatomy. Ans2 |
|
|
An 18-year-old athlete is now 3 months out from anterior cruciate ligament reconstruction. He has been unable to obtain full extension of the knee. His range of motion is from 12° to 125° compared to 0° to 140° on the contralateral knee. He has no effusion, no pain at rest, and a stable Lachman’s test. He is having difficulty ambulating without crutches. What is the most common technical error which can account for these findings? 1. Femoral tunnel drilled too anteriorly 2. Failure to cycle the knee prior to final tibial fixation 3. Femoral tunnel drilled too vertically 4. Tibial tunnel drilled too vertically 5. Tibial tunnel drilled too anteriorly
|
A tibial tunnel drilled too anteriorly will limit full extension and causes tightness in flexion. incorrect Answers: 1. Femoral tunnel drilled too anterior will lead to tightness in flexion and laxity in extension. ans5 |
|
|
The saphenous nerve is most likely to be injured with which of the following steps during an anterior cruciate ligament (ACL) reconstruction with hamstring autograft? 1. Incision for an anteromedial portal with the knee flexed 2. Incision for an anteromedial portal with the knee extended 3. Incision for an accessory medial portal the with knee flexed 4. Hamstring harvest with the knee extended 5. Tibial tunnel aperture fixation with the knee at 30 degrees of flexion |
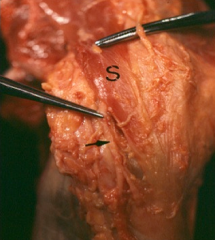
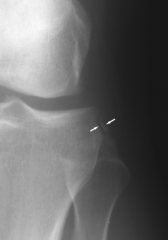
The saphenous nerve is most at risk during the hamstring harvest of an ACL reconstruction. At the joint line, the saphenous nerve is deep to the broad sartorious fascia, and superficial to the gracilis. Bertram et al describe a case report of a patient who sustained saphenous neuralgia following an ACL reconstruction utilizing a hamstring harvest. Symptoms can include paresthesias in the anteromedial region of the lower leg and tenderness at the medial side of the knee. They note that hip external rotation and knee flexion while harvesting the hamstring tendons allows the tendinous structures and saphenous nerve to relax, thus decreasing the chance of injury. Solman et al also stress the understanding of such anatomical relationships of the medial side of knee's anatomy to avoid pitfalls such as saphenous nerve injury during a hamstring harvest. Illustration A provides a depiction of the saphenous nerve with relation to the medial knee. Illustration B is an example of a cadaveric dissection showing the anatomic relationship of the saphenous nerve (black arrow) as it courses superficially along the sartorial fascia (labelled with S).Ans4 |
|
|
1.0 xray =15 genu varum in children 3 years of age, bilateral obesity 1.1 tx 1.2x-ray with 16° genu varum in a 3-year-old with the diagnosis and treatment 1.3 x-ray with 16° genu varum in a 13-year-old was the diagnosis and treatment?
|
1.1 treatment for mild cases observation in infantile BLOUNTS disease 1.2BLOUNTS disease lateral tibia and fibular epiphysiodesis 25 percent require formal osteotomy 1.3 proximal tibia fibula osteotomy |
|
|
A 15-year-old male presents with pain and progressive deformity about his left knee. A standing AP radiograph is seen in figure A, with the tibial growth plate nearly closed. Physical examination reveals significant varus and a leg-length discrepancy of 2.5cm right greater than left. Which of the following is the most appropriate method of management at this time? 1. Orthotics 2. Hemiepiphysiodesis of the left proximal tibia, medial side only 3. Hemiepiphysiodesis of the left proximal tibia, medial and lateral sides 4. Left proximal tibia osteotomy with placement of lengthening external fixator 5. Left proximal tibia osteotomy with plate fixation |
Incorrect Answers: |
|
|
most common cause of acquired spastic equinovarus deformity of the foot? what is the underlying etiology of this deformity? was the treatment of this condition? |
CVA and tBI overactivity of the gastrocnemius soleus complex and the and varus deformity occurs because of the overactivity of the tibialis anterior? the treatment is SPLATT Achilles tendon lengthening with split anterior tibialis tendon transfer
|
|
|
A 65-year-old female developed a right foot deformity 3 years ago following a cerebrovascular accident. She initially underwent early intervention with physical therapy and splinting. However, passively correctable contractures persist and the braces are causing skin problems on the leg. What is the most likely foot and ankle deformity in this patient and the most appropriate surgical treatment to be combined with a planned tendoachilles lengthening (TAL)? 1. Spastic equinovarus and split anterior tibialis tendon transfer (SPLATT) 2. Flaccid equinovarus and medializing calcaneal ostetomy and flexor hallucis longus transfer 3. Spastic calcaneovalgus and split anterior tibialis tendon transfer (SPLATT) 4. Flaccid equinovalgus and split anterior tibialis tendon transfer (SPLATT) 5. Spastic equinovalgus and medializing calcaneal ostetomy and flexor hallucis longus transfer
|
The most common physical finding in patients who have had a cerebrovascular accident is spastic equinovarus deformity of the foot and ankle (Illustration A) from an upper motor neuron injury. Ans1 |
|
|

|
|

|

|
|
|

|
|
|
what is the most common complication with surgical treatment of anterolateral bowing of the tibia? |
recurrent fracture |
|
|
of bowing of the tibia
|

|
|
|
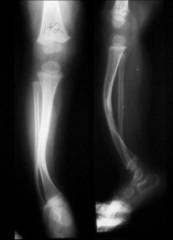
Anterolateral tibial bowing is associated with which of the following lower extremity conditions in children? 1. Calcaneovalgus foot deformity 2. Congenital pseudoarthrosis of the tibia 3. Fibular hemimelia 4. Congenital talipes equinovarus 5. Congenital vertical talus |
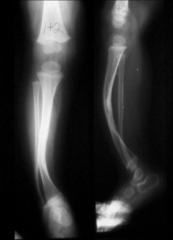
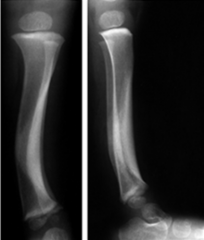
anteroLateral tibial bowing and congenital pSeudoarthroSiS of the tibia are related conditions and represent a continuum of the same disease process. It is most commonly seen in children with neurofibromatoSiS. The radiograph in Illustration A is an example of anterolateral tibial bowing. The radiograph in in Illustration B is an example of congenital pseudoarthrosis of the tibia. ans2 |
|
|
when greater than 50% of the Achilles tendon insertion must be removed for debridement what is the treatment? |
tendon augmentationwith FDL, FDP H or PB |
|
|
what is the treatment forAchilles tendinitis and less than 50% of the tendon has to be removed? |
the treatment is retrocalcaneal bursa excision, calcaneal bony prominence resection |
|
|
what is the key treatment for Achilles tendinitis to be done doing physical therapy? |
eccentric training |
|

A 48-year-old male complains of 5 years of heel pain while running. Initially the pain was relieved with Achilles tendon stretching, orthotics, and open-backed shoe wear. Over the past year these modalities are no longer helpful and he is beginning to have pain with walking. Clinical photograph and radiograph are provided in figures A and B. Which of the following treatment options is the best choice to relieve pain and improve function? 1. Arizona gauntlet brace 2. Steroid injection 3. Achilles tendon debridement 4. Achilles tendon debridement, calcaneal exostectomy, and FHL transfer 5. Ankle arthrodesis |
Clinical photograph and radiograph demonstrate Haglund's deformity and calcifications consistent with insertional Achilles tendonopathy. Failure of conservative management and loss of function are indications for surgical management. Given the large Haglund's deformity on radiograph, calcaneal exostectomy is preferable to tendon debridement alone. ans4 |
|
|
Which of the following exercises is important to incorporate into an Achilles tendinopathy rehabilitation protocol following a period of diminished intensity of activities? 1. Plyometric 2. Isokinetic 3. Concentric 4. Eccentric 5. Isometric |
Eccentric exercises are important to implement into a functional rehabilitation program for Achilles tendinopathy. Eccentric exercises most efficiently strengthen skeletal muscle. Eccentric exercise is a type of isotonic exercise that includes constant muscle tension while the muscle is lengthening.Ans4 |
|
|
what on the 4 effect of NSAIDs in the body? |
|
|
|
what other contraindications to NSAIDs? (2) |
|
|
|
were the side effects of COX 2 specific inhibitors |
?cardiac toxicity |
|
|
side effects of NSAIDs? |
|
|
|
COX to admission has been shown to decrease what an abnormal fracture and models? |
decrease in endochondral ossification |
|
|
All the following medications binds reversibly to the enzyme COX-1 EXCEPT 1. Meloxicam 2. Diclofenac 3. Indomethacin 4. Naproxen sodium 5. Aspirin |
Aspirin binds irreversibly to the cyclooxygenase enzyme. Aspirin acetylates platelet cyclooxygenase and permanently inhibits thromboxane (TX) A2 production leading to its antiplatelet effects. The other NSAID's listed above bind reversibly with COX-1. ans5 |
|
|
Arachidonic acid is directly metabolized by which of the following substances? 1. Carbonic anhydrase 2. HMG-CoA reductase 3. 1-lipoxygenase 4. Cyclooxygenase 5. Thromboxane synthetase |

Arachidonic acid is the common substrate that is directly metabolized by cyclooxygenase into the prostanoids including prostaglandins, prostacyclin and thromboxane. Cyclooxygenase 1 enzyme, or COX-1, results in prostaglandins responsible for maintenance and protection of the GI tract. Cyclooxygenase-II enzyme, or COX-2, results in prostaglandins responsible for inflammation and pain. Leukotrienes are synthesized from arachidonic acid by 5-Lipoxygenase, not 1-Lipoxygenase. Mevalonate is involved in the HMG-CoA reductase pathway – the metabolic pathway that produces cholesterol (site of action of the statins). A diagram of arachidonic acid metabolism is provided in Illustration A.ans4
|
|
|
A 45-year-old man is placed on indomethacin for heterotopic ossification prophylaxis following surgery for an acetabular fracture. What is the most likely side effect of this medication? 1. Renal failure 2. Hepatitis 3. Peripheral neuropathy 4. Deep vein thrombosis 5. Gastrointestinal ulceration |
Indomethacin, commonly used to prevent heterotopic ossification, is associated with a high rate of gastrointestinal toxicity. ans5 |
|
|
|
|
|
|
|
|
patient presents with weakness of ankle plantar flexion what caused this injury? |
S1 nerve root injury |
|
|
patient presents with weakness in hip flexor what caused this injury? |
L2/L3 nerve |
|
|
loss of patellar reflex what caused this injury? |
injury to the L4 nerve root |
|
|
bowel and bladder dysfunction with saddle anesthesia what caused this injury? |
cauda equinus syndrome |
|
|
patient presents with weakness great toe extension causes injury? |
L5 nerve root and weakness with ankle dorsiflexion |
|
|
what is treatment of an adult high-grade spondylolisthesis? |
decompression, L4-S1 posterior lumbar fusion and anterior column support |
|

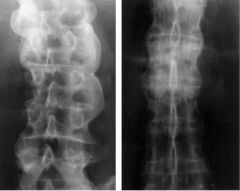
A 26-year-old male presents with chronic back and bilateral leg pain that has not improved with extensive nonoperative management including physical therapy, oral medications, and corticosteroid injections. Radiographs are shown in Figure A. What is the most appropriate next step in treatment? 1. Placement of epidural spinal stimulator 2. Lumbar decompression alone 3. Lumbar decompression with L5 to S1 posterior lumbar fusion 4. Lumbar decompression, L4 to S1 posterior lumbar fusion, and anterior column support 5. Minimally invasive direct lateral interbody fusion with percutaneous pedicle screw placement |
The clinical presentation and imaging studies are diagnostic of a high grade spondylolisthesis that has failed nonoperative management. Surgery is indicated, and the procedure of choice is a posterior lumbar decompression with an instrumented fusion from L4 to S1 with anterior column support.aaans4 |
|
|
the patient presents with bilateral sacroiliitis, uveitis and HLA-B27 what is the diagnosis? |
ankylosing spondylitis |
|

what is the diagnosis? What is the treatment? |
vertebral scalloping or bamboo spine ankylosing spondylitis marginal syndesmophytes |
|

patient with a known history of ankylosing spondylitis presents to the ER after trauma to his neck and initial x-rays are negative what is the next most appropriate step in the management of this patient? |
CT scan to rule out cervical fractures MRI scan to rule out epidural hemorrhage after cervical fracture in a young patient |
|
|
All of the following are characteristics of juvenile ankylosing spondylitis EXCEPT? 1. Spinal stiffness 2. Sacroiliitis 3. Urethritis 4. Enthesitis 5. Kyphosis
|
Juvenile Ankylosing spondylitis (AS) one of the spondyloarthropathies that is characterized by sacroiliitis, spondylitis, enthesitis, HLA B-27, kyphosis, asymmetric lower extremity inflammatory arthritis, decreased chest expansion, and uveitis, but NOT Urethritis (which is typical of the triad of Reiter syndrome). ans3 |
|
|
A patient with ankylosing spondylitis and a hip flexion contracture undergoes uneventful right total hip replacement using a Kocher (posterior) approach. This patient is at increased risk for which of the following complications post-operatively? 1. Posterior hip dislocation 2. Anterior hip dislocation 3. Deep infection 4. Osteolysis 5. Periprosthetic fracture
|
Degenerative joint disease due ankylosing spondylitis (AS) with a concomitant hip flexion contracture increases post-operative rates of anterior hip dislocations. Correction of hip flexion contracture with THA can restore sagittal balance. However, when positioning the acetabular component in a patient with AS, one must account for the relationship of the pelvis to the lumbar spine in the sagittal plane in order to avoid an excessively hyperextended hip once the patient resumes an upright position.ans2 |
|
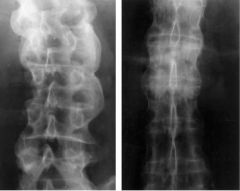
A 32-year-old man presents with low back and hip pain that has been gradually worsening over the past year. He reports the symptoms are worse in the morning. Radiographs are shown in Figure A. Laboratory studies show a positive HLA-B27. What additional finding will help confirm the diagnosis? 1. Erythema marginatum 2. Positive HLA-DR3 3. Uveitis 4. Positive Rheumatoid Factor 5. Elevated urine phosphoethanolamine
|
The radiograph in Figure A shows bilateral sacroiliitis. Bilateral sacroiliitis (with or without uveitis) and a postive HLA-B27 is diagnostic of ankylosing spondylitis. ans3 |
|
|
A 45-year-old man with ankylosing spondylitis presents with fixed sagittal imbalance and difficulty with horizontal gaze. His kyphotic deformity is localized to the thoracolumbar spine. Which of the following procedures allows the most correction in the sagittal plane at a single level without having to resect the intevertebral disc? 1. Smith-Petersen osteotomies 2. Pedicle subtraction osteotomy (PSO) 3. Vertebral column resection (VCR) 4. Single-level opening wedge osteotomy 5. Multi-level opening wedge osteotomies
|
Pedicle subtraction osteotomy (PSO) provides greater sagittal correction than single-level opening wedge osteotomy and Smith-Petersen osteotomies, with the advantage of working at a single level and not having to resect the intevertebral disc.ans2 |
|
|
|
|
|
what is the best predictor of curve progression? |
in Femaleit is just before menarche or RISSER 1 the best method is it tender method to determine skeletal maturity |
|
|
patient idiopathic scoliosis curve is seen how much curvature is allowed in order to treat in the following method
|
|
|
|
with the most common organism causing delayed infection after scoliosis surgery? |
Propionibacterium acnes |
|

A mother and her 16-year-old daughter present to your clinic because the daughter has noticed asymmetries in her back. She has no back pain and no neurologic symptoms. She is two years post-menarcheal. After a complete history and physical, you order PA thoracolumbar radiograph, which is seen in figure A. The cobb angle is 38 degrees. When discussing the natural history of the disease, you tell the family they should expect: 1. difficulty with vaginal child birth in the future. 2. decreased pulmonary function in the future 3. to undergo an MRI to rule out any underlying neurologic pathology, as this is an abnormal curve 4. an increased risk of chronic back pain over her lifetime 5. this curve magnitude has the highest curve progression rate without operative intervention |
Discussion: The patient is presenting with classic adolescent idiopathic scoliosis (AIS). She has an apex at T8, which makes this a main thoracic, Lenke type 1 curve. While AIS is commonly referred to as a painless condition, Weinstein et al. published the 50-year follow-up, of 117 untreated patients with AIS compared to 62 age- and sex-matched controls and found a statistically significant (p = 0.003) increase in chronic back pain over 50 years. Incorrect Answers: |
|
|
When compared to normal controls, adults with untreated idiopathic scoliosis and a Cobb angle of greater than 60 degree at the time of skeletal maturity have a higher rate of which of the following? 1. Acute and chronic back pain 2. Premature death 3. Disability 4. Clinical depression 5. Limitation in activities of daily living |
Patient with untreated adolescent idiopathic scoliosis with a curve of 60 degrees or greater at skeletal maturity have an increased rate of low back pain relative to normal controls.ans1 |
|
|
what is most common complication complication of an untreated scoliosis curve? |
acute and chronic back pain |

