![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
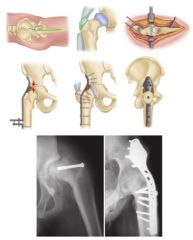
1-mc & C indication for 1^ hip arthrodesis? C |

1-MC salvage for failed THAc-young active laborers with painful unilateral, ankylosis after infection or trauma, neuropathic arthropathy, tumor resection2-MC severely debilitating back pain, severe ipsilateral knee pain with instability, severe contralateral hip pain3-assess the status of the gluteus medius, constrained acetabular component is required if the abductor complex is nonfunctional4-flex-25 (20-35), adduc-5, ER=5-10; avoid abd bc/ creates pelvic obliquity & inc back pain5-later app w/ trochanteric osteotomy, anterior; cobra plating 6-function of abd muscles7-ipislater kneepain/DJD; contralateral hip pain/DJD low back pain/DJDcontraindications-severe limb-length discrepancy greater than 2.0 cm, bilateral hip arthritis, severe osteoporosis, adjacent joint degenerative changes lumbar spine, contralateral hip, ipsilateral knee;contralateral THA
|
|

You are caring for an 18-year-old boy with severe hip arthritis and pain from a missed slipped capital femoral epiphysis. You decide that a hip arthrodesis is the best treatment option. What is the optimum position for a hip arthrodesis to maximize function and prevent complications? |
Hip arthrodesis is a salvage procedure for patients with hip arthritis without ipsilateral knee, contralateral hip, or lumbar spine pathology. The optimal position for hip arthrodesis is 0-5 degrees of adduction, 0-5 degrees of external rotation, and 20-35 degrees of hip flexion. Ans2 |
|
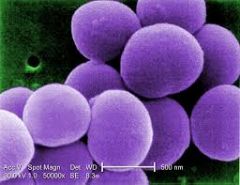
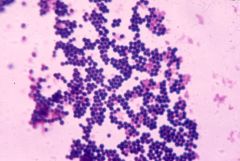
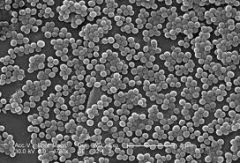
1-risk factors for neonatal septic arthritis? MC approach2-4 joints with intra-articular metaphyses include?3-mechanism of destruction septic arthritis?4-MC organism: adolescents, Tx? following varicella infection? does not require surgical debridement? neonates w/ community-acquired infection, Tx ? child > 2 yrs? HACEK organ- aka nosocomial infections of neonates grow after a week of blood cx med?5-poor prognostic indicators w/ septic hip 4? septic joint aspirate will show?6-on PE hip, MI view7-90% chance of septic arthritis if 3 out of 4 of the following are present mn, therefore ML not___?-best predictor of septic arthritis, #2?
|

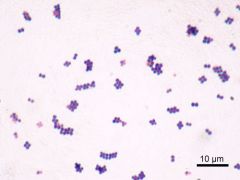
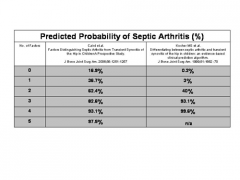
1-prematurity, c section; A=med 2-shoulder, hip, elbow, ankle,3-release of proteolytic enzymes (matrix metalloproteinases, MMPs)-> inflam & synovial cells, cartilage, bacteria damage w/in 8 hrs & inc jnt press may cause fem head osteonecrosis if not relieved promptly4-adol=neisseria G->oxacillin/cephalosporin; varcella=Group A beta-hemo strep->1st gen cephalosporin; no surg=neisseria G; commun-Acq-neonate<12 mth=Grp B strep->1st gen cephalosporin; >2=Staph A->2nd / 3rd gen cephalosporin; HACEK, Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, and Kingella, gram-negative bacilli: enhanced capacity to produce endocardial infections5-age < 6 mths, hip > knee, present > 4 days ago, assoc osteom hip; -aspir=high WBC count (> 50,000/mm3 with >75% PMNs)gluc 50 mg/dl < serum levelshigh lactic acid level w/ infections due to g(+)cocci/ g(-) rods6-hip=flex, abd, ER; MIV-frog lat7-mn 2,4,12, 101.4 2>crp, 40>ESR, 12K>wbc, 101.4/38.6best=fever, CRP >2
|
|

A 7-year-old boy developed a limp with right leg pain five days ago, and today has trouble bearing weight. On exam, he is lethargic and has chills. His temperature is 38.4 degrees centigrade. He points to his right inguinal region as the source of the discomfort. He winces with compression of his pelvis. Lab studies reveal a white blood cell count of 11,400/ul, CRP of 9 mg/dL (normal < 1.0 mg/dL), and erythrocyte sedimentation rate of 55 mm/h. A pelvis radiograph is shown in Figure A. Ultrasound guided aspiration of the right hip joint yields 9,000 leukocytes per mL. What is the most appropriate next step in management? 1. Further imaging of the pelvis2. Open drainage and irrigation of the right hip joint3. Repeat aspiration of the hip joint4. Percutaneous screw fixation of the proximal femoral physis5. Nonsteroidal antiinflamatory medications and observation
|
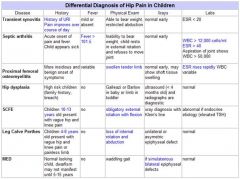
This patient has clinical signs of infection with symptoms localized to the pelvis. The differential diagnosis includes transient synovitis, pelvic osteomyelitis, and rheumatologic disorders. Further imaging,US, is required to confirm the diagnosis. The radiographs are not consistent with a slipped capital femoral epiphysis. The Kocher criteria for septic arthritis include fever>38.5 degrees centigrade, inability to bear weight, ESR>40 mm/h, and WBC count>12,000/ul. In this case, 2/4 of the criteria are positive (inability to bear weight & ESR>40mm/h), which indicates approximately a 40% likelihood of septic arthritis. Synovial fluid analysis is used to either confirm or reject the hypothesis of suspected septic arthritis; an aspiration of < 50,000 leukocytes per mL virtually rules out sepsis of the joint. Ans1
|
|
Which of the following is true regarding matrix metaloproteinases (MMPs)? 1. They are activated by chelating agents2. They mediate the destruction of cartilage in septic arthritis3. Toll-like receptors inhibit the formation of MMPs4. They have a anabolic effect on cartilage5. Stromelysin is an indirect antagonist of many MMPs
|
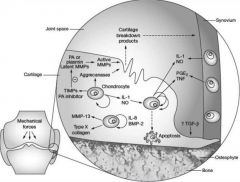
Matrix metalloproteinases have been associated with the destruction of cartilage in septic arthritis. Matrix metalloproteinases and their inhibitors, tissue inhibitors of metalloproteinases (TIMPs), are crucial to extracellular matrix remodeling in normal tissue development and maintenance. Additionally, their over-expression has been associated with cartilage degradation in diseases such as rheumatoid arthritis, osteoarthritis, and septic arthritis. In septic arthritis, toll-like receptors activate the NF-kB pathway which leads to the production of MMPs and resulting cartilage destruction.Incorrect Answers:Answer 1: Chelating agents bind to metals that serve to activate MMPs, thus inactivating them.Answer 3: Toll-like receptors have been linked to the NK-kB pathway, which activates the formation of MMPs.Answer 4: MMPs have a catabolic effect on cartilage.Answer 5: Stromelysins are a subgroup of matrix metalloproteinases.Ans2
|
|
|
3 yo child with fever, toxic appearance,children refuse to walk or move their hip, PE-localized swelling, effusion, tenderness, and warmth. severe pain with passive motion, unwillingness to move joint (pseudoparalysis).1-KIF(key image finding) -->Dx 1.1 other KIF1.2 DDX, what 4 factor assoc / septic arthritis 1.3 sx-4 ->dx1.4 pe->x1.5 other images->dx1.6 other labs->dx2-Tx 3-Complication 7 & salvage x2
|

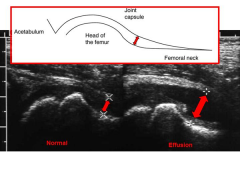
1-AP/frog-leg lat pelvic x-rays=may be nl, especially in early stages of dz, often see widening of the joint space, subluxation, or dislocation,-in infants, prior to ossification ->fem head, widening of joint space -> lateral displacement of prox fem Dx =Hip Septic Arthritis 1.1US-ID effusion1.2- transient synovitis, 90% septic arthritis if 3-4 of follwg (+)1.3 presents more acutely >osteo; (2)fever & other systemic symptoms = toxic appearance (3)children refuse to walk or move their hip (4) NOT hx of rash & swollen lymph nodes1.4 localized swellg effusion, tenderness warmthhip rests -> flex, abd, ER; severe pain w/ passive ROM, unwillingness move joint (pseudoparalysis)examine adjacent jnts1.5 US NOT MRI1.6 WBC, ESR, CRP, Asp jnt2-tx=Emergent I & D, IV-Abx based on age x 4 wks3-Fem head destruc-salvage operations ->varus/valgs prox fem osteotomies Deformity-late angular deformity & LLD Jnt contracture, Hip dislctn, Growth disturbanceGait abns, ON/AVN
|
|
|
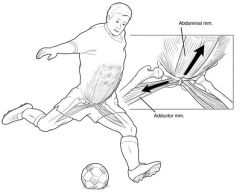
1-repetitive microtrauma to the pubic symphysis aka2-what MC sports assoc w/ dx of osteitis pubis, why?3-muscles in region w/attachments? (6)
|
1-Inflammation of the pubic symphysis caused by repetitive trauma2-soccer, hockey, football and running; repetitive microtrauma to the pubic symphysis bysports involving repetitive kicking & repetitive add/abd3-adductor magnus adductor brevis adductor longus gracilis rectus abdominispectineus
|
|
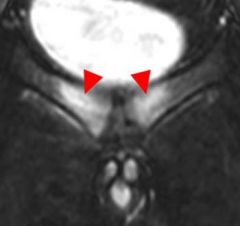
A 26-year-old rugby player has been having progressive anterior pelvic pain for the last 3 months. He is diagnosed with osteitis pubis, and a non-operative treatment regimen is initiated. What is the KIF of this patients diagnosis? ___?
|
classic findings of osteitis pubis including bony erosion and irregularity with early widening of the pubic symphysis.
|
|
adult soccer player, c/o vague, ill-defined pain is anterior pelvic region. PE=localized tenderness directly over the pubic symphysis.1-KIF(key image finding) -->Dx 1.1 sx->dx1.2pe->x1.3 ddx(5)1.4 other images->dx2-(indications) T2.1 treatment for vast majority of cases
|

1-AP pelvis->osteolytic pubis w/ bony erosions & often times diastasis of the symphysis1.1sx=vague, ill-defined pain is anterior pelvic region, worse with activities involving hip add/abd @ ant pelvis, may have spasms with hip add1.2PE=localized tenderness directly over the pubic symphysis1.3-Athletic publagia, Stress fx of the pubic ramiStress fx of the fem neck, Inguinal herniaOncologic disease (rare)1.4 MRI-bone marrow edema found early BS-increased activity in area of pubic symphysis2.1 NSAIDS, rest, activity modification, self-limiting process which usually resolves with non-operative treatment, may take several months to resolve
|
|
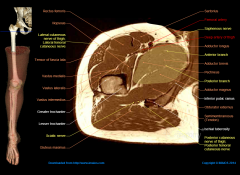
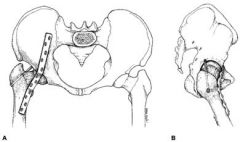
1-(5)Indications medical approach to hip, aka?1.2-internervous plane of med approach to hip? what nerve innervates ____which muscle__ ? 2-description of skin incision from A-B & length/orientation?3-superficial dissection to hip?4-deep dissection to hip?5-(4)structures at risk,6-cross sectional anatomy
|
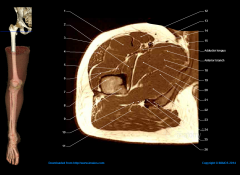
1-(1)open reduction of cong hip dislocation; (2) psoas release (3)biopsy(4) txt of tumors of the inf portion of feml neck & medial aspect of prox fem shaft (5)obturator neurectomy1.2-no superficial internervous plane-bt/ add brevis & add magnus, ant division of the obturator N2-A=begin incision 3 cm below the pubic tubercleB=length of incision is determined by the amount of femur that needs to be exposed-Incision longitudinal incision over the adductor longus 3-Sup diss=develop plane between gracilis and adductor longus muscles4-develop plane b/t add brevis & add mag until you feel lesser trochanter on the floor of the wound5 MFC A & Deep ext. pudendal A, Ant & Post Div of & of obturator N,
|
|
Tenotomy of which muscle performed during an anteromedial approach for surgical reduction of a congenitally dislocated hip places the medial femoral circumflex artery at risk? 1. semimembranosus2. biceps femoris3. iliopsoas4. rectus femoris5. sartorius
|
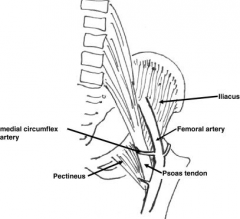
Weinstein and Ponseti suggested that the anteromedial approach provides "a safe, effective way to reduce a dislocated hip in infancy". The superficial plane is between gracilis and adductor longus. The deep plane is between adductor brevis and adductor magnus. During this approach, the iliopsoas tendon can be released, but should be fully exposed above and below the lesser trochanter so as not to injure the medial femoral circumflex artery. Ans3
|
|
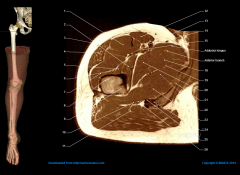
Following an uneventful medial approach to the hip, the iliopsoas tendon is released. Which of the following neurovascular structures is most at risk during release of the tendon? 1. obturator nerve2. obturator artery3. femoral artery4. medial femoral circumflex artery5. sciatic nerve
|
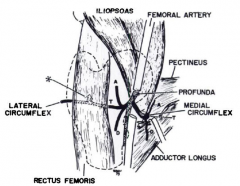
The medial approach to the hip involves utilizing the interval between adductor longus and gracilis, then adductor brevis and magnus in order to arrive at the lesser trochanter, psoas tendon, and hip capsule. As seen in the illustrations below, the medial femoral circumflex artery is in close proximity to the psoas tendon as it wraps medial and posterior to the distal portion of the tendon to travel to the posterior proximal femur.Ans4
|
|

1-define simple vs complex hip dislocation? what is approch for Open redctn2-MC type of hip dislocation? aka? MoI?***3-associated inj patterns w/ post dislctd hip? (5)3-associated inj patterns w/ ant dislctd hip? MoI? 2 types of ant discln, descr? mn4-presentation of post hip dislctn vs ant hip dislctn5- what test required after all traumatic hip disclns, why? 36-emergent CR w/in ___hrs? contraindications7-lesser trochanter shadow reveals___? make sure of what on hip xray?
|

1-simple=pure dislocation w/out assoc fx complex=dislocation assoc w/ fx of acetabulum or prox femPD=post (Kocher-Langenbeck) apprAD=ant (Smith-Petersen) appr 2-MC-pos dislctn, dashboard inj, axial load through flex knee & addON/AVN, post wall acetabular fx, fem head fx,sciatic N inj, ***ipsil knee inj (up to 25%)3-fem head impaction or chondral injury,MoI=hip ->abd & ERtype=inf & sup, hip ext -> superior (pubic) dislctn; flex -> inf (obturator) dislctn4-P Dislctn=flex, add IR PIN AXE (posterior - internal, anterior external). Anterior dislocations rotate externally. A dislctn=flex, abd, ER5-post redctn CT-r/o fem head fx, loose bodies acetabular fx 6-6 h, ipsilateral displaced or ND fem neck fx7-IR limb as compared to contralateral, scrutinize femoral neck to rule out fracture prior to attempting CR
|
|
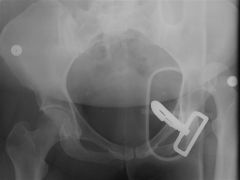
A 41-year-old female sustains the injury shown in Figure A as a result of a high-speed motor vehicle collision. After a successful attempt at closed reduction in the emergency room using conscious sedation, repeat radiographs show a reduced hip joint. What is the next most appropriate step in treatment? 1. Femoral skeletal traction2. CT scan of hip and pelvis3. Dynamic fluoroscopic examination under general anesthesia4. Hip spica dressing5. Touch down weight bearing mobilization
|
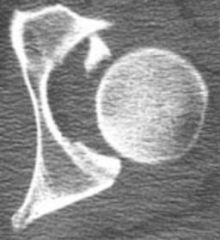
The radiograph shown in Figure A reveals a left hip dislocation, with some obscuring of detail secondary to the trauma backboard. CT scans should be obtained following a hip dislocation to evaluate for fractures or impacted areas of the femoral head or acetabulum, as well as noncongruent reductions and free intraarticular joint fragments. ANs2
|
|

A 30-year-old driver is involved in a motor vehicle collision and sustains the injury shown in Figure A. What is the most likely concomitant injury? 1. Right knee meniscus tear2. Left knee ACL tear3. Subdural hematoma4. Right ankle fracture-dislocation5. Lumbar burst fracture
|

Traumatic hip dislocation results from the dissipation of a large amount of energy about the hip joint. Clinically, these forces often are first transmitted through the knee en route to the hip. It is therefore logical to look for coexistent ipsilateral knee injury in patients with a traumatic hip dislocation. Ans 1
|
|
|
20 yo s/p high speed MVA, c/o acute pain, inability to bear weight, deformity, PE-vitals signs nl1-KIF(key image finding 4) -->Dx__1.1 sx->dx1.2pe->PEF of Ant disloctn vs PEF for post dislcnt mn1.3 other images->dx2-(Indications) Tx & Rehab/Time 2.1 acute anterior and posterior dislocation2.2 radiographic evidence of incarcerated fragment delayed presentation, non-concentric reduction2.3 acetabulum fx + hip dislocation2.4 post op?3-Complication 4
|

1KIF=AP pelvis r/o fem head smaller < contralateral side; Shenton's line broken; lesser troch shadow reveals IR limb compared to contralateral side, scrutinize fem neck to rule out fx prior to attempting CR. Dx-hip dislocn A or P1.1 sx=acute pain, inability to WB, defrmty1.2 PE=P Dislctn=flex, add IR, detailed neurovascular exam (10-20% sciatic N inj, exam knee -> assoc inj or instability PIN AXE (posterior - IR anterior external). AD= ER. A dislctn=flex, abd, ER1.3 other KIF-CT=must look->fem head fx, loose bodies, acetabular fxMRI-NOT routine r/o labrum, cartilage & fem head vascul2.1 emergent CR w/in 6 hrs2.2 Opn redctn & +/- removal of incarcerated frag2.3 ORIF2.4=pwb 4-6 wks3=post tram DJD, fem ON/avn, Sciatic N inj, reccurrent dislctns
|
|

A 27-year-old man sustains a Gustilo and Anderson type II open tibia fracture during a motorcycle accident. He had his full 3 doses of tetanus vaccination as an infant. He also had a tetanus booster vaccination 18 months ago when he began a new job. In addition to intravenous antibiotics, what tetanus prophylaxis should be administered? 1. No prophylaxis required2. Tetanus vaccine3. Tetanus immune globulin4. Tetanus vaccine and tetanus immune globulin5. Tetanus vaccine and tetanus immune globulin with a booster vaccine required 6 months from now
|
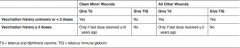
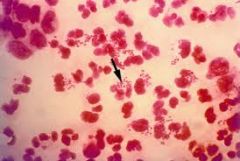
The tetanus vaccine, booster, and immune globulin are used to enhance the immune response to clostridium tetani, a gram positive bacillus found in soil. In this case, the patient's tetanus had been updated within the past 5 years so he does not need an update of the vaccination or immune globulin. Illustration A is a concise table that can be used as an algorithm to provide appropriate tetanus prophylaxis.Ans1
|
|

A 25-year-old male involved in a motorcyle accident sustains the injury seen in Figures A and B. After adequate debridement of nonviable tissue, which of the following irrigation methods and devices should be used? 1. Antibiotic solution applied by low pressure gravity flow device2. Antibiotic solution applied by high pressure pulsatile flow device3. Saline solution applied by low pressure gravity flow device4. Saline solution applied by high pressure pulsatile flow device5. Antibiotic solution applied by high pressure pulsatile flow device followed by low pressure gravity flow device
|

Figures A and B reveal a Type IIIB open tibia fracture with obvious gross contamination and devitalized tissue. Systemic antibiotics and tetanus prophylaxis should be administered immediately upon arrival, and the lower extremity should be splinted while the remaining trauma workup takes place. Once cleared, this injury should be adequately debrided of all devitalized tissue and subsequently irrigated with a saline solution to reduce the bacterial count. Some evidence suggests that high-pressure pulsatile lavage damages bone structure and disrupts soft tissue. In an animal model, Hassinger et al showed that high-pressure pulsatile lavage caused deeper penetration of bacteria and results in greater bacterial retention in soft tissue when compared with low-pressure lavage. Ans 3
|
|
|
what of the risk factors for septic hip neonate |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|
|
|
|
|
|
|
|

|

|
|
|
what R for poor prognostic indicators of the patient with septic arthritis as a child |
|
|

child presents to the clinic with toxic appearance, refuses to walk and on physical exam severe pain with range of motion
|

|
|

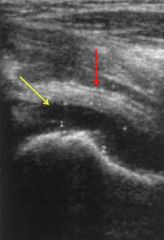
patient presents to the emergency room with hip the rest in flexion abduction and externally rotated, and ultrasound is done
|

|
|
|
in patient < 12 months of age – neonate
|
|
|
|
indications 6 months to 5 years
|
|
|
|
|
|
|
|
|
|
was most common organism to cause septic arthritis in the in the acquired pneumonia nosocomial septic arthritis |
staph aureus |
|

A 7-year-old boy developed a limp with right leg pain five days ago, and today has trouble bearing weight. On exam, he is lethargic and has chills. His temperature is 38.4 degrees centigrade. He points to his right inguinal region as the source of the discomfort. He winces with compression of his pelvis. Lab studies reveal a white blood cell count of 11,400/ul, CRP of 9 mg/dL (normal < 1.0 mg/dL), and erythrocyte sedimentation rate of 55 mm/h. A pelvis radiograph is shown in Figure A. Ultrasound guided aspiration of the right hip joint yields 9,000 leukocytes per mL. What is the most appropriate next step in management? 1. Further imaging of the pelvis 2. Open drainage and irrigation of the right hip joint 3. Repeat aspiration of the hip joint 4. Percutaneous screw fixation of the proximal femoral physis 5. Nonsteroidal antiinflamatory medications and observation |
clinical signs of infection with symptoms localized to the pelvis. The differential diagnosis includes transient synovitis, pelvic osteomyelitis, and rheumatologic disorders. Further imaging is required to confirm the diagnosis. The radiographs are not consistent with a slipped capital femoral epiphysis.ans1 |
|

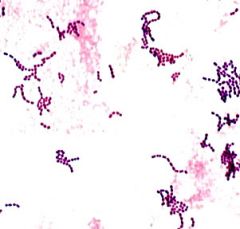
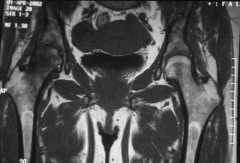
An 8-month old infant is brought by his parents to your office for fever and malaise. Your inspection of the patient is detailed in Image A. An oral temperature of greater than 38.5 has been found to be the best predictor of this child's condition. What is the second best predictor? 1. Elevated neutrophil count 2. Elevated ESR 3. Elevated rheumatoid factor 4. Elevated CRP 5. Presence of bacteria on CSF gram stain |
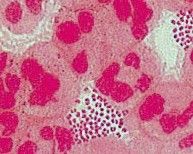
clinical image reveals a flexed, abducted, and externally rotated left hip. This hip position maximizes intracapsular volume and indicates a left hip effusion as described in the review by Sucato. |
|

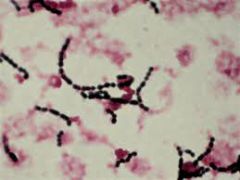
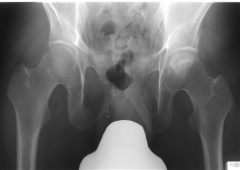
A 10-month-old infant is brought to the emergency department for fevers, irritability, and avoidance of motion in the right leg. On physical exam, passive motion of the right hip elicits crying. An AP pelvis and an ultrasound of the right hip are shown in Figures A and B respectively. A hip aspiration yields 82,000 WBC with >80% PMNs. Which of the following is the strongest predictor of a poor prognosis? 1. CRP > 5mg/L 2. Delay in treatment >4 days 3. Age > 6 months 4. Absence of associated osteomyelitis 5. ESR > 40mm/hr |

The clinical scenario is consistent with a pediatric septic hip. The AP pelvis in figure A shows soft-tissue swelling with mild subluxation of the right hip due to a septic effusion, and the ultrasound in figure B also shows a hip effusion. The hip aspiration is consistent with an infectious process. An aspirate with WBC >50,000 is highly suggestive of a septic hip. Jackson et al reviewed pediatric septic arthritis and describe four poor prognostic signs: age <6 months, joint effusion with underlying osteomyelitis, hip involvement, and delay in treatment >4 days. In a review of pediatric septic hips, Sucato et al state that hip aspiration is the most sensitive test and that I&D is required to prevent late sequlae. ans2 |
|

|
|
|

what the next best diagnostic studies to confirm the diagnosis of this condition |
|
|
|
|
|
|
A 45-year-old with a history of sickle cell anemia reports hip pain for the past 6 months. A radiograph of the affected hip is shown in Figure A. Which of the following interventions has been shown to have the best outcomes in this patient population? 1. Observation 2. Bisphosphonates 3. Hemi-arthroplasty 4. Uncemented metal on polyethylene total hip arthroplasty 5. Cemented metal on polyethylene total hip arthroplasty |
the best intervention is an uncemented metal on polyethylene total hip arthroplasty. |
|
|
what percent of sickle cell anemia disease patient with AVN of the femoral head going on to collapse |
> 75% likelihood for progression of pain and collapse |
|
|

|
|
|
|
|
|
patient had a femoral resurfacing procedure done returns to the 1st postop visit complaining groin pain with the diagnosis |
femoral neck fracture periprosthetic |
|
|
contraindications for a hip scope 5 |
|
|
|
when doing a hip arthroscope what is a landmark for the iliopsoas tendon |
zone orbicularis |
|
|
with the most common complication with hip arthroscopy 2 |
pudendal nerve neurapraxia peroneal nerve |
|
|
what is the most at risk structure with the anterolateral portal hip scope |
superior gluteal nerves |
|
|
External rotation of the hip |
|
|
wwhat structure at risk with anterior portal of the hip arthroscopy |
|

