![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back
|
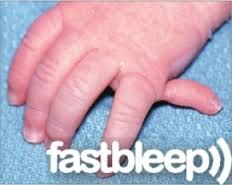
1-MCC of symbrachydactyly and shortening of middle fingers |
1&2-Poland Syndrome (3) 1-unilateral chest wall hypoplasia, due to absense of sternocostal head of pectoralis major 2-hypoplasia of the hand and forearm 3-symbrachydactyly and shortening of middle fingers
3-release produces skin deficiency that requires skin grafting 4-perform only one side of the digit at a time 5-web creep |
|

Which of following malformations is most commonly associated with Poland's syndrome?
1. complex syndactyly. 2. amniotic band syndrome. 3. radial club hand 4. symbrachydactyly 5. thumb polydactyly |

symbrachydactyly which is most commonly associated with Poland's syndrome.
Poland's syndrome is a rare birth defect characterized by underdevelopment or absence of the chest muscle in conjunction with ipsilateral symbrachydactyly. Poland syndrome most often affects the right side of the body, and occurs more often in males than in females.Ans4 |
|

Syndactyly is associated with all of the following conditions EXCEPT?
1. Apert syndrome 2. Poland's syndrome 3. Holt-Oram syndrome 4. Carpenter syndrome 5. Tay-Sach's Disease |

Syndactyly is one of the most common congenital hand deformities with an incidence of 1 in 2000 live births and is associated with Poland's syndrome (chest wall deformity with limb hypoplasia), Apert syndrome (autosomal dominant inheritance with mental retardation, craniosynostosis), Holt-Oram syndrome (also known as "heart-hand syndrome" with abnormalities of the heart and upper limbs), and Carpenter syndrome (acrocephaly, peculiar facies). There is no association of syndactyly with Tay-Sach's disease.Ans5
|
|
|
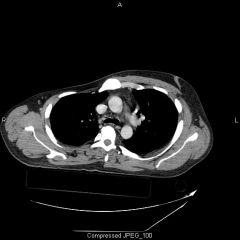
infant w/Sprengel’s deformity, scoliosis, dextrocardia
absence or underdevelopment of the breast PE=absence of extensors or flexor tendons carpal coalition or hypoplasia, hypoplasia or absence of metacarpals or phalanges. 1-KIF(key image finding) -->Dx 1.1 KPEF 1.2 ***OKIF 2- Tx*** 3-Complication (6) |

1KIV=AP hand& forearm=syndactyly, hypoplasia or absence of metacarpals or phalanges, carpal coalition or hypoplasia, radioulnar synostosis
Dx=Poland Syndrome= (3) 1-unilateral chest wall hypoplasia, due to absense of sternocostal head of pec mjr 2-hypoplasia of the hand and forearm 3-symbrachydactyly and shortening of middle fingers 1.1KPEF=extent of hand and chest involvement varies;chest deformities=hypoplasia or absence of the pec major, pectoralis minor, deltoid, serratus anterior, external oblique, and latissimus dorsi, Sprengel’s deformity, scoliosis dextrocardia, absence or underdevelopment of the breast, hand deformities, syndactyly, hypoplasia or absence of metacarpals or phalanges, absence of exten or flex tendons, carpal coalition or hypoplasia, radioulnar synostosis, nail agenesis 1.2 ***OKIF-CT chest-absent pectoralis major 2-***syndactyly release + skin grafting 3-Skin graft fail, Excessive tension, Improper flap planning Digital A inj, Web creep Nail defrmty |
|

1-#1 & #2 MCC of death in children; #1 & #2 MC presenting lesions in abused children
2-w/ child abuse what is most frequent cause of long term physical morbidity in the child? 3-MC age of child abuse? if suspect child abuse what is mandatory? 4-if child abuse goes unreported, ____chance of repeat abuse and ___ chance of death from abuse 5 DDx of child abuse (3); MC loc of fx in child abuse 6 social risk factors for child abuse (3) 7-(7)red flags for child abuse? MC presenting fx pattern seen in abused children |

1-#1-accidents #2-child abuse;-
-#1 skin cuts or bruises & #2 fx 2- head injury 3-<3yo; report abuse to appropriate agency & admit infants with fractures to the hospital and consult child protective services 4-50% repeat, 10% death 5-true accidental injury, OI, metabolic bone Dz; diaphyseal 6-recent job loss, step children, child w/ special needs 7-(1)long bone fxs in infant NOT yet walking, (2)multiple fxs in various stages of healing, (3)corner fxs (4)posterior rib fx (5)bucket handle fx (6)transphyseal separation of the distal hum (7)multiple bruises MC-Single transverse long bone fx |
|
|
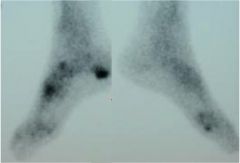
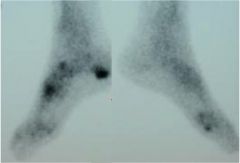
2 yo child w/ non ambulatory CP c/o pain PE=skin lesions
1-KIF(key image finding) -->Dx *** 1.1 initial evaluation includes? 2-Tx 3-Complication/Prognosis(2) 3.1/DDX |

1-xray &PE r/o 7 red flags of child abuse:1)long bone fxs in infant NOT yet walking, (2)multiple fxs in various stages of healing, (3)corner fxs (4)posterior rib fx (5)bucket handle fx (6)transphyseal separation of the distal hum (7)multiple bruises
1.1-skeletal survey if>5 yo Bone scan bc/ skeletal surveys not as reliable in older children 2-report abuse to appropriate agency, admit infants with fractures to the hospital and consult child protective services 3-50% repeat, 10% death 3.1-report abuse to appropriate agency, true accidental injury, OI, metabolic bone Dz; diaphyseal |
|

1-MC forms of polyethylene sterilization, why is only one method used?
2-what leads to early failure of PE? 3- what are the effects of oxidation on PE? 4-(5)mech properties of highly crosslinked PE?*** 5-(3)methods to obtain sterilization in oxygen depleted environment |

1-gamma radiation in an air environment ->PE becomes oxidized->leads to early failure
-gamma radiation in argon, nitrogen->PE becomes cross linked ->improved resistance to adhesive and abrasive wear decrease in mechanical properties 2-sterilization in oxygen rich environment, oxidized 3-leads to early failure due to: subsurface delamination, pitting, fatigue cracking ***4-improved resistance to adhesive wear -improved resistance to abrasive wear (decreased mechanical properties:) -decreased ductility -decreased fatigue resistance -greater risk of catastrophic failure under high loads 5-argon, nitrogen, vacuum environment |
|
|
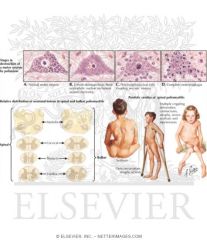
1-name 3 forms of Polydactyly of Hand
2-MC type of Preaxial Polydactyly (Thumb Duplication), define 3-which type of Preaxial Polydactyly (Thumb Duplication) is NOT associated w/a syndrome 4-describe Wassel Classification of Preaxial Polydactyly 5-(4)goals of treatment Preaxial Polydactyly (Thumb Duplication) 6- Bilhaut-Celoquet define, used to TX what 7-which polydactly is MC in blacks, Tx; Central Polydactyly tx high association w/? |
1-preaxial polydactlyly= thumb duplication
postaxial polydactlyly=small finger duplication centrall polydactlyly 2-type 2-Duplicated distal phalanx 3-7-Triphalangia 4-1=Bifid distal phalanx; 3=Bifid proximal phalanx; 5=Bifid metacarpal 2-Duplicated distal phalanx 4-Duplicated proximal phalanx 6-Duplicated meatcarpal 7-Tri-phalangia 5-construct a thumb that is 80% of the size of the contralateral thumb, resect smaller thumb (radial side) preserve / reconstruct medial collateral structures in order to preserve pinch function reconstruction of all components typically done in one procedure 6-involves removing central tissue and combining both digits into one, type 1,2,3 7-Postaxial Polydactyly (Small Finger Duplication), ti off in nursery: syndactyly , |
|
|
Which of the following congenital hand deformities is more prevalent in patients of African-American ancestry?
1. Constriction band syndrome or amniotic band syndrome 2. postaxial polydactyly, 3. Preaxial polydactyly 4. Syndactyly 5. Macrodactyly |

ostaxial polydactyly, which is more prevalent in patients of African-American ancestry.
The cohort study by Woolf found the incidence of postaxial polydactyly in African americans is 12.42 per 1,000 (1.2%) compared to the Caucasian incidence of 0.91 per 1,000 (0.09%). If postaxial polydactyly is found in a patient of Caucasian ancestry then further workup for underlying syndromes (chondroectodermal dysplasia or Ellis-van Creveld syndrome) is needed. Ans2 |
|

The Bilhaut-Cloquet procedure for thumb duplication, where the central portions of bone and nail are removed and the radial half of one thumb is combined with the ulnar half of the other to create one thumb, is most appropriate in which Wassel Type shown in Figure A?
1. Type 2 2. Type 4 3. Type 5 4. Type 6 5. Type 7 |
Bilhaut-Cloquet procedure has been shown to be successful in Wassel Type 1, 2, and 3 deformities. Asymmetrical Type I or II duplications with distinct components may also be treated with ablation of the smaller thumb with transfer of the collateral ligament and centralization of the extensor tendon. Types 3 and 4 duplications (Type 4= most common duplication) are often treated with selection of a dominant thumb and ablation of the lesser counterpart after preservation and transfer of intrinics and collateral ligaments. The article by Ogino states that the ablation of the radial thumb is most common and Miller's Review states radial thumb ablation is preferred. Treatment of Types 5 and 6 duplication utilizes similar principles as Type 4 deformities, with the added complexity of additional intrinsic reconstruction. Type 7 is a triphalangeal thumb and has variable treatment based on the presentation, and reconstruction includes excision versus fusion of the extra phalanx.Ans1
|
|
|
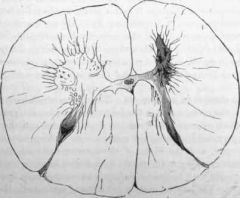
1-hallmark of polio? cause by?
2-postpolio syndrome? what is it NOT? how to treat? |
1-motor weakness w/ nl sensation, viral destruction of the anterior horn cells in the spinal cord and brain stem motor nuclei
2-aging phenomenon where more nerve cells become inactive with time, leads to increasing difficulty performing activities of daily living, aka may experience muscle weakness and fatigue as an adult tx-patients should exercise at sub-exhaustion levels to tone affected muscle groups without causing muscle breakdown |
|
A newly adopted 7-year-old girl from Liberia has a history of poliomyelitis 2 years ago. She had flaccid paralysis of her legs that made her bedridden for 6 months. She has recovered all strength and has no complaints at this time. The parents would like to know if they should be concerned about any residual effects of the infection. How should they be counseled?
1. The child has no risk of further paralysis or weakness from polio 2. The child may experience muscle weakness and fatigue as an adult 3. If the child has no recurrent episodes of paralysis by the time she reaches skeletal maturity, then she will never have further weakness 4. The child will certainly have weakness and possibly paralysis as an adult, and therefore she should abstain from sports to prevent further muscle injury 5. The child will most likely be wheelchair bound by the age of 25 years. |
Poliomyelitis is a viral infection that infects the central nervous system and can cause flaccid paralysis. Post-polio syndrome may occur in up to half of patients who have previously been afflicted with polio. The syndrome is characterized by muscle weakness, myalgia, and fatigue. Onset is typically 20-40 years following the initial infection. The exact mechanism is not completely understood. Patients exhibiting post-polio syndrome should be counseled to get regular exercise to sub-exhaustion levels. This is designed to keep the muscle groups toned without causing any muscle breakdown that could potentially have deleterious long-term effects.
Ans2 |
|
|
child c/o muscle weakness with normal sensation, from third world country.
1-Dx 1.2-KPEF 2-Tx indications 2.1-tendon transfers, contracture releases, and arthrodesis 2.2 lightweight orthoses 2.3 if orthoses do not achieve satisfactory standard of living |
1-polio
1.1 weakness nl sensation 2-vaccine, limited exercise with periods of rest, +/- lightweight orthosis 2.1 used to optimize functional capacity 2.2-first line of treatment 2.3-contracture release, tendon transfer, and arthrodesis |
|
1-what is the Modified Whelan Classification used for? define
describe type 2 & 3 & 4 of 5 Popliteal Artery Entrapment Syndrome, 2-Mc age and sex to get Popliteal Artery Entrapment Syndrome, 3-Pathophysiology Popliteal Artery Entrapment Syndrome |
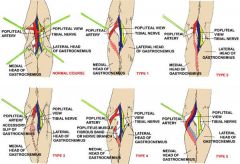
1-Popliteal Artery Entrapment Syndrome=A condition characterized by constriction of the popliteal artery by either adjacent muscles, tendons, fibrous tissues
Type II Medial head of the gastrocnemius is located laterally, no deviation of popliteal artery Type III There is an abnormal muscle bundle from the medial head of the gastrocnemius that surrounds and constricts the popliteal artery Type IV Popliteal artery is entrapped by the popliteus muscle 2-male predominance (about 4:1) patient age typically 25-40 years old 3-decreased blood flow distal to the popliteal fossa leading to signs and symptoms consistent with compartment syndrome |
|
|
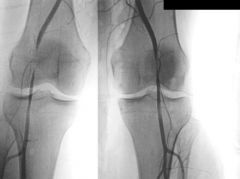
adult male c/o limb swelling & calf cramping following light exercise which improves with vigorous exercise. on PE=diminished pulses with active foot plantar flexion or passive foot dorsiflexion.
1.0-KIF(key image finding w/ 99% sensitivity) -->Dx 1.1other imaging use to make Dx(3) 1.2 Sx of Dx (4) 1.3 PE of Dx (3) 2-Tx indications 2.1mild symptoms with rigorous exercise only 2.2 if damage to the popliteal artery or vein 3-Complication (3) |

1.0-Arteriogram r/o will show stenosis, obliteration and post-stenotic dilation
1.1-Doppler US=less invasive than arteriogram r/o will show stenosis, obliteration and post-stenotic dilation -MRI/MRA and CT/CTA= for detection of popliteal artery entrapment 1.2-swelling, pts often report limb swelling as primary complaint; -paresthesias, foot numbness and paresthesias also common; tingling sensation of toes following vigorous exercise; -cramping, calf cramping following light exercise which improves with vigorous exercise; -limbs can occasionally be asymptomatic 1.3PE=diminished pulses with active foot plantar flexion or passive foot dorsiflexion -coolness of posterior calf and paresthesias may also be present -can easily be confused with posterior compartment syndrome 2.1activity modification and observation 2.2vascular bypass with saphenous vein vs endarterectomy 3-30% rate of return of entrapment (2)can result in need for amputation (3)wound infection (4) DVT |
|
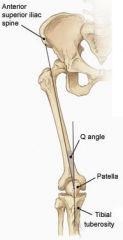
1-MCC of TKA? Most important variable in proper patellar tracking is__ in TKA?
2-Abnormal Q angle, an increase in the Q angle will lead to__? 3-***critical to avoid techniques that lead to increase Q angle. Common errors include (4) mn 4-the Q angle is defined as angle between __&__? 5-when referencing posterior condylar axis normal relation of the posterior condylar axis to the transepicondylar axis to maintain a rectangular flexion gap? mn lateral femoral condyle is hypoplastic, use of the posterior condylar axis may lead to --? 6-best way to obtain this is to have the tibial component centered over __? 7-preferred position of the patellar prosthesis is__?** if medialized then___? ***if patella laterally subluxes intraop during trialing, then___? |
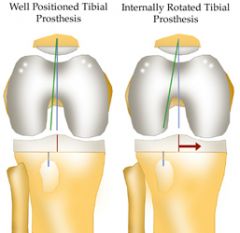
1-MCC TKA=Abnormal patellar tracking
-MIV=preservation->nl Q ang 2-abn Q=inc latel subluxation forces on the patella poss pain, mech sx, accelerated wear, even dislocation. 3-***avoid (4)- Injurious IR fem, IE tib, med of fem, lat of patella 4-axis of extensor mech (ASIS to center of patella) & axis of patellar T (cntr of patella to tibial tub) 5 PCA= 3 deg IR to transepicondylar axis Thus, the posterior femoral cut should be made in 3 deg of ER is Excellent from the posterior condylar axis in order to produce a rectangular flexion gap. ; hypo=IR of fem component 6-Tib pros=med 1/3 tibial tubercle 7-centered over the patella or medialized; med=smaller patellar prosthsis ***lat sublx=deflate tourniquet and recheck before performing a lateral release |
|
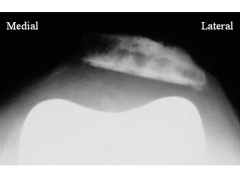
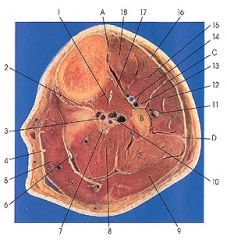
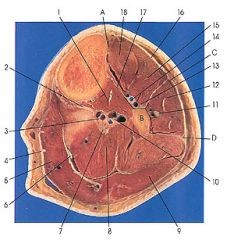
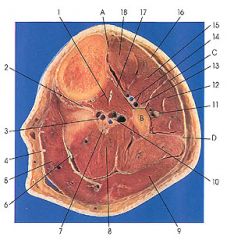
Following a left total knee arthroplasty, all of the following can cause the condition seen in Figure A EXCEPT:
1. Internal rotation of the femoral prosthesis 2. Internal rotation of the tibial prosthesis 3. Lateralization of the femoral prosthesis 4. Medialization of the tibial prosthesis 5. Lateralization of the patellar prosthesis |
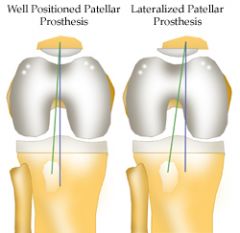
Lateralization of the femoral prosthesis would not lead to lateral patellar subluxation. However, lateralization of the patella or the tibial tray could lead to lateral patellar subluxation. Medialization, not lateralization of the femoral prosthesis will increase the Q angle and lead to lateral subluxation of the patella. Ans3
|
|
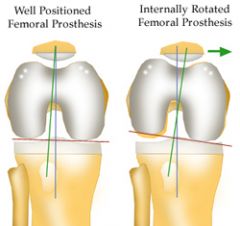
The posterior condylar axis may be used to determine the rotation of the femoral component in total knee arthroplasty. Which of the following describes the normal relation of the posterior condylar axis?
1. Parallel to the transepicondylar axis 2. Perpendicular to the anteroposterior axis (Whiteside's line) 3. 3 degrees externally rotated to the transepicondylar axis 4. 3 degrees internally rotated to the transepicondylar axis 5. 7 degrees externally rotated to the transepicondylar axis |
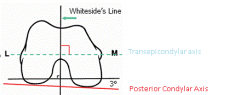
To recreate an appropriate rectangular flexion gap, the femoral component should be aligned parallel to the transepicondylar axis. The transepicondylar axis is perpendicular to the anteroposterior axis (Whiteside's line). The posterior condylar axis is normally 3 degrees internally rotated to the transepicondylar axis. Thus, the posterior femoral cut should be made in 3 degrees of external rotation from the posterior condylar axis in order to produce a rectangular flexion gap. Ans4
|
|

1-common injuries seen with phalanx dislocation? (2)
-must get xray of___? 2-PIP dislocations MC in what direction? If this injury what MCC? if dorsal dislocation what may acts as block to reduction with longitudinal traction? 3-classif of PIP dislocations dorsal? classi of Dorsal PIP Fracture-Dislocations which stable? 4-MCC w/ Volar PIP Dislocation & Fracture-dislocations 5-what is name of one of phalangeal condyles is buttonholed between central slip and lateral band 6-MC block to reduction in irreducible closed DIP joint dislocation 7-additional tx option if highly comminuted injuries with significant soft tissue loss w/Dorsal DIP Dislocations & Fracture-Dislocations |

1-swan neck deformity, nail bed injuries
-hand xrays to rule out associated fractures & finger xrays-must get true lat of joint 2-PIP Dislocations=Dorsal doral=volar plate inj, swan neck inj block-volar plate 3-simple=middle phalanx in contact with condyles of proximal phalanx vs complex=base of middle phalanx not in contact with condyle of proximal phalanx, bayonet appearance Dor DID dislctn=stable=<30%-treat with dorsally based extension block splint unstable=> 40% 4-V PIP MCC= boutonneire deformity, injury to the central slip and at least one collateral ligament, 5-button hole=Rotatory PIP dislocation 6MCC block=volar plate interposition 7highly comm=amputation |
|

A 27-year-old man falls on his hand at work. He notices an immediate deformity of his ring finger. Radiographs are provided in Figure A. Which of the following is the most appropriate initial treatment?
1. Closed reduction, buddy taping, and early motion to prevent stiffness 2. Closed reduction and full time extension splinting 3. Open reduction and repair of the central slip of the extensor tendon 4. Open reduction and repair of the volar plate 5. Amputation and immediate return to play |
volar PIP dislocation. The central slip of the extensor tendon is frequently ruptured and will lead to a boutonneire deformity if left untreated. The PIP must be immobilized in extension to allow the extensor mechanism to heal. Immobilization in extension should be maintained for 6 weeks to allow soft tissue healing. Open reduction and repair of the central slip would be the appropriate treatment for a developing boutonneire deformity that presents in a subacute or chronic time basis. Illustrations A and B demonstrate a schematic and clinical photo of central slip disruption and secondary deformity with PIP flexion and DIP hyperextension (Boutonniere Deformity). Posner et al reviewed 7 patients with chronic palmar dislocations of the PIP joint who were treated with open reduction and reconstruction of the extensor mechanism. Ans2
|
|
|
1-treatment indications: |
1.1-D PIP D=reduce and buddy tape to adjacent finger (3-6 weeks) untx=swan-neck , volar plate and at least on collateral ligament, |
|
|
|
|
|
80% of child abuse occurs in children in what age group |
children less than 4 years of age |
|
was most common cause of femur fracture in nonambulatory implant |
child abuse |
|

if child abuse is not reported what are the risk of repeat abuse and a risk of death |
repeat abuse = 50% Death =10% |
|

Corner fracture caused by child abuse most likely affects what area of bone |
primary spongiosum of the metaphysis – highly specific for child abuse |
|
|
name 3 fractures there are characteristically seen with child abuse |

|
|
|
was the most common presenting lesion in child abuse |
skin lesions |
|
|
is suspect child abuse then what the next most appropriate steps in the management of this condition 3 |
|
|
|
|
|
|
|
|
|
what is the most common complication of the patella non-resurfaced in the total knee arthroplasty compared to resurfaced |
most common complication is increased anterior knee pain and increased need for secondary resurfacing however no increased risk of
|
|
|
The posterior condylar axis may be used to determine the rotation of the femoral component in total knee arthroplasty. Which of the following describes the normal relation of the posterior condylar axis? 1. Parallel to the transepicondylar axis 2. Perpendicular to the anteroposterior axis (Whiteside's line) 3. 3 degrees externally rotated to the transepicondylar axis 4. 3 degrees internally rotated to the transepicondylar axis 5. 7 degrees externally rotated to the transepicondylar axis |
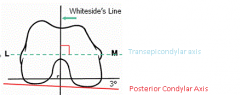
To recreate an appropriate rectangular flexion gap, the femoral component should be aligned parallel to the transepicondylar axis. The transepicondylar axis is perpendicular to the anteroposterior axis (Whiteside's line). The posterior condylar axis is normally 3 degrees internally rotated to the transepicondylar axis. Thus, the posterior femoral cut should be made in 3 degrees of external rotation from the posterior condylar axis in order to produce a rectangular flexion gap. |
|
|
when taking an x-ray of the hand to rule out the in an injury to the phalanx
|
|
|

|

|
|

|

|
|

|

|
|

|
|
|

|

|
|

A 27-year-old man falls on his hand at work. He notices an immediate deformity of his ring finger. Radiographs are provided in Figure A. Which of the following is the most appropriate initial treatment? 1. Closed reduction, buddy taping, and early motion to prevent stiffness 2. Closed reduction and full time extension splinting 3. Open reduction and repair of the central slip of the extensor tendon 4. Open reduction and repair of the volar plate 5. Amputation and immediate return to play |

The radiograph demonstrates a volar PIP dislocation. The central slip of the extensor tendon is frequently ruptured and will lead to a boutonneire deformity if left untreated. The PIP must be immobilized in extension to allow the extensor mechanism to heal. Immobilization in extension should be maintained for 6 weeks to allow soft tissue healing. Open reduction and repair of the central slip would be the appropriate treatment for a developing boutonneire deformity that presents in a subacute or chronic time basis. Illustrations A and B demonstrate a schematic and clinical photo of central slip disruption and secondary deformity with PIP flexion and DIP hyperextension (Boutonniere Deformity). Posner et al reviewed 7 patients with chronic palmar dislocations of the PIP joint who were treated with open reduction and reconstruction of the extensor mechanism. All patients acheived satisfactory range of motion and the authors concluded that this technique is preferable to arthrodesis. Peimer et al reviewed 15 patients with palmar dislocations of the PIP joint. Twelve of the fifteen were evaluated on a delayed basis (average 11 weeks following injury) and underwent open reduction and surgical repair of the extensor tendon. Three of the fifteen were seen earlier following injury and were treated with closed reduction and pinning. All fifteen patients acheived satisfactory clinical outcomes although finger range of motion was not fully recovered in any case.Ans2 |
|

|
|
|

|
|
|

patient has pain 1st steps in the morning when getting out of bed and pain worse at the end of day with prolonged standing, BMI = 35
|

|
|
|
shock wave treatment for chronic heel pain lasting > 6 months |
|
For the treatment of new onset plantar fasciitis, which of the following modalities results in the highest patient satisfaction at 8 weeks of follow-up? 1. Achilles tendon–stretching program 2. Corticosteroid injection 3. Extracorporeal shock-wave therapy 4. Plantar fascia–specific stretching program 5. Distal tarsal tunnel decompression and partial plantar fascia release |

A plantar fascia-specific stretching program has the highest patient satisfaction at the 8 week follow-up interval. Symptoms of plantar fasciitis include “start-up” inferior heel pain with patients often preferring to walk on their toes for the first few steps when getting out of bed. The pain lessens with ambulation and then increases again with increased activity. Illustration A depicts a patient performing plantar fascia-specific stretching. Illustration B displays a patient performing an achilles tendon–stretching program. |
|
|
what is the most common form of polyethylene sterilization |
gamma radiation |
|
|
in the presence of oxygen free radical formation occurs what is the effect on the polyethylene |
the polyethylene is oxidized and leads to early failure by way of
|
|
|

the polyethylene is cross-linked which leads to improve resistant to adhesive and abrasive wear by way of
|
|

|
|
|
|
if well formed digit then reconstruction
|
|

|
|
|
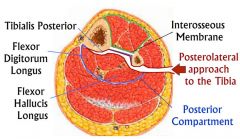
when performing a posterior lateral tibia
|
|
|
|
|
|
|
|
|
|
to the out to prevent and avoid injuryto the
|
|
|
|
What two muscles lie on the posterior aspect of the interosseous membrane and tibia in the lower leg, and must be elevated during a posterolateral approach to the tibia for treating a nonunion? 1. Flexor digitorum longus and tibialis posterior 2. Peroneus longus and peroneus brevis 3. Peroneus brevis and peroneus tertius 4. Tibialis posterior and tibialis anterior 5. Tibialis posterior and flexor hallucis longus |
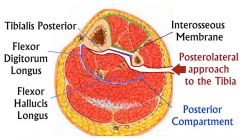
The flexor digitorum longus and tibialis posterior lie on the posterior aspect of the interosseous membrane and tibia. Flexor hallucis longus lies on the posterior border of the fibula. The superficial internervous plane lies between the gastrocnemius/soleus (tibial nerve) and peroneal muscles (superficial peroneal nerve). The deep dissection involves detaching FHL and soleus from the posterior border of the fibula and then dissecting medially to separate the posterior tibialis off the the posterior surface of the interosseous membrane and the posterior tibialis and flexor digitorum longus off the posterior surface of the tibia.ans1 |

