![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
6 Cards in this Set
- Front
- Back

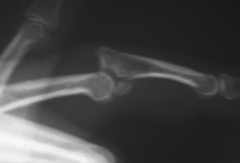
Hx: 34yo M sustains the closed finger inj Fig A x 1 wk ago. He undergoes CRPP Fig B to correct alignment. Which is responsible for the apex palmar fx deformity noted on the preop xray? 1. Indirect pull of the central slip on the distal fragment and the interossei insertions at the base of the prox phalanx; 2-Intrinsic muscle fibrosis and intrinsic minus contracture; 3-PIP jt volar plate attenuation and extensor tendon disruption
4-Rupture of the central slip with attenuation of the triangular lig & palmar migration of the lateral bands; 5-Flex tendon disruption w/ associated overpull of the extensor mechanism |

The clinical presentation is consistent with a transverse proximal phalanx fracture. These fracture have an apex palmar angulated deformity under the indirect pull of the central slip on the distal fragment and the interossei insertions at the base of the proximal phalanx, If proximal phalanx fractures are allowed to heal with the apex palmar deformity, an extensor lag will result. Therefore CRPP or ORIF is indicated in transverse fractures with > 10° angulation. To correct this deformity prior to surgical fixation, the MCP joint should be flexed, which allows the extensor mechanism as a whole to function as a tension band to help reduce the fracture. This is referred to as intrinsic plus splinting. Incorrect Answers:
Answer 2: Intrinsic muscle fibrosis and contracture is usually associated with chronic crush injuries and significant soft tissue damage. Answer 3: This is describing a swan neck deformity. Answer 4: This is describing a Boutonnierre deformity. Answer 5: Flexor tendon disruption is not likely in this closed injury pattern.Ans1 |
|

Hx:39yo M sustained an index finger injury 6 mths ago and has failed 8 wks of splinting. a current xray Fig B. Which of the following is true regarding open reduction and screw fixation of this injury? 1-High risk of symptomatic implant; 2-Immobilization of the DIP joint is required for 2 wks post-op
3-High rates of post-op infection are common 4-Open reduction via an approach through the nail bed leads to significant post-operative nail deformity; 5-ROM of the DIP joint in the affected finger is usually less than 10 degrees post-operatively |

Open reduction and internal fixation of distal phalanx fracture non-unions frequently requires the post-operative removal of the fixation implant after complete fracture healing.
Chim et al followed 14 patients with non-union of fractures of the shaft of the distal phalanx who were treated with open reduction and screw fixation. The implants required removal in 13/14 patients, and the mean post-operative range of motion of the DIP joints was 56 degrees. No immobilization was required postoperatively, and bone grafting was only necessary in two patients with severely comminuted fractures. Finally, the authors recommended approaching the fracture through the nailbed for the best exposure, and found no postoperative nail growth complications. Postoperative infections were not common in their series.Ans1 |
|
Hx:28yo professional baseball player injures his middle finger sliding into the catchers shin guard at home plate. c/o pain and deformity of the middle finger. xray fig A. All are true EXCEPT: 1-Anatomic reconstruction of the articular surface is prognostic of clinical function; 2-Proximal interphalangeal joint subluxation precludes a normal gliding flexion arc; 3-Hinging at the fracture site must be avoided
4-Early motion should be initiated in postoperative therapy; 5-Early degenerative arthritis can be expected if the joint is not adequately reduced. |

a dorsal fracture dislocation of the proximal interphalangeal joint of the middle finger. Kiefhaber and Stern review the presentation, evaluation, and treatment of PIP fractures. Congruent reduction of the joint to allow the middle phalangeal to glide around the proximal phalangeal head is paramount to prevent joint subluxation and instability. Anatomic reconstruction of the articular surface is desirable but not necessary for successful clinical outcome.Ans1
|
|

Hx:27yo M falls on his hand at work. He notices an immediate deformity of his ring finger. xrays Fig A. Which is the most appropriate initial tx? 1-CR, buddy taping, and early motion to prevent stiffness
2-CR & full time extension splinting; 3-Open reduction and repair of the central slip of the extensor tendon; 4-Open reduction and repair of the volar plate; 5-Amputation and immediate return to play |
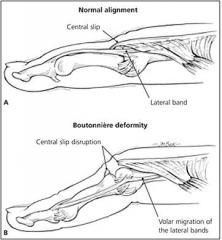
The radiograph demonstrates a volar PIP dislocation. The central slip of the extensor tendon is frequently ruptured and will lead to a boutonneire deformity if left untreated. The PIP must be immobilized in extension to allow the extensor mechanism to heal. Immobilization in extension should be maintained for 6 weeks to allow soft tissue healing. Open reduction and repair of the central slip would be the appropriate treatment for a developing boutonneire deformity that presents in a subacute or chronic time basis.Ans2
|
|

Hx:25yo F is involved in a motorcycle collision and presents with the injuries seen in Fig A. What is the best option for definitive management of the injuries seen? 1-ORIF; 2-CR & casting; 3-Ex-fix; 4-Immediate therapy; 5-Removable splint
|
Multiple metacarpal shaft fractures are best managed with open reduction and internal fixation as non-operative management is associated with loss of motion, asynchronous grasp and decreased grip strength.Ans1
|
|

A collegiate rower complains of dorsal wrist pain for 6 weeks refractory to NSAIDs and bracing. Maximal tenderness is palpated on the dorsoradial forearm approximately 5 cm proximal to the wrist. Pain is exacerbated with resisted wrist extension. Radiographs are unremarkable. A steroid injection should be directed into the compartment containing which of the following structures? 1-APL and EPB tendons; 2-ECRL and ECRB tendons; 3-EPL tendon; 4-APL and ECRB tendons; 5-Brachoradialis tendon
|
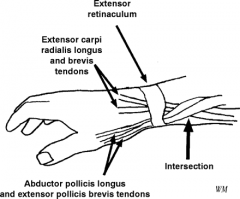
a inflammatory response to overuse at the site of the second dorsal compartment crossing under the first dorsal compartment approximately 5 cm proximal to the wrist. An anatomical depiction is provided in illustration A. Injections of the second dorsal compartment, which includes ECRL and ECRB, may relieve symptoms and quell inflammation. Intersection must be differentiated from DeQuervain's syndrome, which is tenosynovitis of the first dorsal compartment. Injections of the first dorsal compartment, which includes APL and EPB, are part of the treatment algorithm for Dequervain's.Ans2
|

