![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
64 Cards in this Set
- Front
- Back
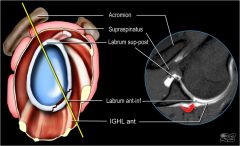
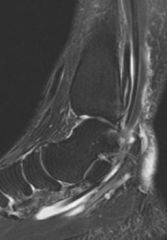
1-reverse Bankart lesion aka |
1-Posterior Labral Tear2-incomplete and sometimes concealed avulsion of posterior labrum3-post labrum4-Jerk-subluxation with posteriorly applied force while arm is in flexion and internal rotationkim-subluxation with posteriorly applied force as arm is dynamically adducted by examiner5-axillary nerve; KPEF- burning pain lat shoulder & teres minor weakness of external rotation (horn blowers sign)6-MRI arthrogram7- 1mm
|
|

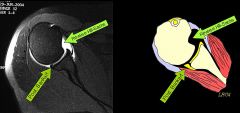
A 20-year-old college football offensive lineman undergoes arthroscopic right shoulder surgery for the injury shown in Figure A. Post-operatively he complains of burning pain in the region marked in yellow on Figure B. Which of the following nerves was most likely injured during the procedure? 1. Radial 2. Upper subscapular 3. Lower subscapular 4. Suprascapular 5. Axillary
|

The posterior branch of the axillary nerve travels within 1mm of the inferior capsule of the glenohumeral joint and can be injured with suture passing devices during posterior-inferior labral repairs. The superior-lateral brachial cutaneous nerve and the nerve to the teres minor always arise from the posterior branch. Injury can lead to teres weakness of external rotation and sensory symptoms in the lateral arm in the region marked by yellow in Figure B. posterior branch of the axillary nerve has an intimate association with the inferior aspects of the glenoid and shoulder joint capsule, which may place it at particular risk during capsular plication or thermal shrinkage procedures.Ans5
|
|
|
football linemen (blocking) injuries his shoulder. c/o shoulder pain, mechanical symptoms (clicking, popping) w/ ROM PE=(+) subluxation with posteriorly applied force while arm is in flexion and internal rotation, posterior joint line tenderness.1-KIF(key image finding) -->Dx & aka1.1 Sx/Dx (3)& PEF/Dx (4); 2 prov test1.2 MoI2-Tx indications2.1-NSAIDs, PT-rotator cuff strengthening and periscapular stabilization2.2-posterior labral repair with capsulorrhaphy3-(2)Complication ->Prevention/location
|

1-KIV=intra-articular contrast (MRI arthrogram) increases sensitivity for labral pathology, XRAY-nlDx-Posterior Labral Tear aka reverse Bankart lesion1.1-sx=shoulder pain, sense of instability, mechanical symptoms (clicking, popping) w/ ROMPEF-pos JL tenderness, Posterior Load & Shift, Jerk test=subluxation w/ pos applied force while arm is in flex & IR; Kim test=sublux w/pos applied force as arm is dynamically add by examiner1.2-pos directed force with arm flex, add, IR2.1-PT:I-first line of tx2.2 SAS:I-extensive nonop management fails3-Axillary nerve palsy-travels within 1 mm of the inferior shoulder capsule and glenoid rim-Overtightening of posterior capsulecan lead to anterior subluxation or coracoid impingement,
|
|
|
1-MMC adult-acquired flatfoot deformity? synergistic w/ PTT good forTT(tendon transfer)2-if young males with mild pes planus R/O what 2 categories of conditions?(7) mnx23-what nerve inn PTT? what else does this nerve innervate4-where is the watershed area of PTT? Triple arthrodesis what jnt?5-major antagonist to PTT is____? 5 functions of PTT 6-how to determine whether deformity is flexible or fixed, Cotton osteotomy def & purpose7-Simmon angle & Meary angle which xray view seen
|
1-PTTI;FDL NOT fhl2-seroneg spondyloarthropathy -PAIR P-psoriatic A- Ankylosing , I-inflamm bowel Dz, Reiters syn ALL HLAB27 & inflamm arths CRP-C-Crystals gout P-Pseudogout R-(RA)3-post tibial N-med plant N->LAFF- L-1st Lumbrical, A- Abd Hallucis, F- Flex digi brv, F- flex hall brev lat plant N-> quad plantae, flex dig mini, add hall, interossei, 3 lumbricals. abd dig mini. Cutan innerv-> lateral sole, lateral 1& 1/2 toes4-poor intrinsic blood supply exists bt/ navicular & disl med mall (2-6 cm prox to navicular insertion)3=calcaneocuboid, talonavicular, subtalar5-mjr antagonist PTT =peroneus brvsPTT(1)#1 dynamic support -> arch(2)hindfoot invertor (3)add & sup-> forefoot during stance of gait(4)acts as 2^ PF of ankle (5) locking of transverse tarsal jts creating a rigid lever->toe-off phase of gait6-Coleman block tst; Cotton=PF openg wedge med cuneiforum ostmy fix forft vars7-Simmon-AP incrd talo-1st MT >20, 0-20 nlMeary-Lat loss of parallelism between the 1st met
|
|

A 54-year-old female has a painful flatfoot that has not improved with over 8 months of conservative management with orthotics. Preoperatively, she was unable to perform a single-heel rise and her hindfoot was passively correctable. Figures A and B are radiographs of the affected left foot. She undergoes FDL tendon transfer to the navicular, medial slide calcaneal osteotomy, and tendoachilles lengthening procedures. Following these procedures, the appearance of the foot is demonstrated in Figure C. What is the next most appropriate intraoperative procedure to be performed during her foot reconstruction?1. Dorsiflexion closing wedge medial cuneiform osteotomy 2. In-situ 1st-3rd tarsometatarsal joint arthrodesis 3. Plantarflexion opening wedge medial cuneiform osteotomy 4. Lateral column closing wedge shortening osteotomy 5. Subtalar arthrodesis
|
The hx, PE, XR =Stage 2B PTTI. In acquired flat foot deformity, the hindfoot falls-> valgus w/compensatory varus developing ->forefoot. loss of parallelism between the 1st MT & talus on lat view and >30% of talonavicular uncoverage on the AP. PF opening wedge medial cuneiform osteotomy (Cotton osteotomy) is an adjunctive proced used to correct the residual forefoot vars component, as shown in Fig B, of a flatfoot deformy p/ hindfoot has been surgically corrected to neutral. The correction of the residual forefoot varus w the Cotton osteotomy creates a plantigrade foot &restores the tripod effect of ft. Incorrect 1: DF closing wedge medial cuneiform osteotomy would exacerbate the deformity.2: 1st-3rd TMT jnt arthrodesis can be performed in lisfranc injuries.4: Lateral column closing wedge shortening osteotomy is not indicated but an Evans lateral column lengthening osteotomy can be used in PTTI5: Subtalar arthrodesis is indicated subtalar Arthritisans3
|
|
A 44-year-old female has a Stage 2B acquired flat foot deformity that does not improve over 6 months of conservative management. She undergoes FDL tendon transfer to the navicular, calcaneal osteotomy, and tendoachilles lengthening. After this correction, it is thought that she would benefit from a opening wedge first cuneiform (Cotton) osteotomy. Which of the following best describes the Cotton osteotomy? 1. Plantarflexion osteotomy to correct residual forefoot varus 2. Medial opening wedge osteotomy to correct residual forefoot abduction 3. Plantarflexion osteotomy to correct residual forefoot valgus 4. Medial opening wedge osteotomy to correct residual hindfoot abduction 5. Plantarflexion osteotomy to correct residual hindfoot valgus
|

Plantarflexion opening wedge medial cuneiform osteotomy is an adjunctive procedure used to correct the forefoot varus (Illustration A) component of a flatfoot deformity as described in the review article by Tankson. In acquired flat foot deformity, the hindfoot falls into valgus with compensatory varus developing in the forefoot. After achieving surgical correction of the hindfoot to neutral, residual forefoot varus is addressed to obtain optimal foot reconstruction (Illustration B). Johnson et al performed a Level 4 study that showed that a Cotton osteotomy produced good results and may offer advantages over 1st metatarsal-cuneiform fusion including predictable union, preservation of first ray mobility, and the ability to easily vary the amount of correction. Illustration C is a drawing of the plantarflexion Cotton osteotomy.Ans1
|
|

A 56-year-old woman comes to your office with foot pain after a 9 month trial of orthotics. Your examination reveals the hindfoot is in valgus, the arch is depressed, and the forefoot is abducted when the foot is viewed posteriorly. She is unable to perform a single heel rise on the affected side. The hindfoot is flexible and there is an equinus contracture. What combination of surgical interventions is most appropriate 1. Tenosynovectomy followed by UCBL orthotic use 2. Dwyer closing wedge calcaneal osteotomy, 1st metatarsal closing wedge osteotomy, and plantar fasica release 3. Medial calcaneal displacement osteotomy, FDL tendon transfer, and tendoachilles lengthening 4. Arthrodesis of the subtalar, talonavicular, and calcaneocuboid 5. Lateral calcaneal displacement osteotomy, FDL tendon transfer, and tendoachilles lengthening
|

This patient presents with a Stage 2B acquired flatfoot deformity. The review articles by Myerson and Pinney discuss the classification and management of adult acquired flatfoot deformity. Stage 1 presents with medial ankle pain due to posterior tibial tendon synovitis. Stage 2 presents with a hindfoot in valgus and inability to perform a single limb heel rise. Stage 2A has a normal forefoot whereas Stage 2B has an abducted forefoot, exposing “too many toes” when the foot is viewed posteriorly. Stage 3 occurs over time as the hindfoot becomes rigid in a valgus position and Stage 4 develops as the deltoid ligament becomes incompetent and the talus tilts into valgus. Tenosynovectomy can be used in Stage 1 disease that fails conservative management. Answer 2 is used as a treatment for cavovarus feet. Answer 4 is a treatment option for Stage 3 disease. Answer 5 is not an option as a lateral displacement calcaneal osteotomy would exacerbate the patient's hindfoot valgus. Ans3
|
|

A 70-year-old female complains of progressive pain of the medial ankle and foot over the past 10 years. Orthotics no longer provide relief of her pain. The hindfoot deformity is unable to be passively corrected on physical exam. Figure A is a posterior view of the patient's foot upon standing and a current radiograph is provided in Figure B. Which of the following is the best treatment option? 1. Posterior tibialis tendon debridement 2. FDL transfer to navicular and calcaneal slide osteotomy 3. FDL transfer to navicular, calcaneal slide osteotomy, and lateral column lengthening through the cuboid 4. Talocalcaneal arthrodesis 5. Triple arthrodesis
|

Image demonstrates the "too many toes" sign consistent with posterior tibialis tendon dysfunction. Failure of the hindfoot to correct during physical exam renders this a fixed rather than flexible deformity (Stage III) warranting triple arthrodesis. Flexible deformity (Stage II) may be surgically treated with calcaneal osteotomy, FDL transfer, and lateral column lengthening. The review article by Deland and ICL by Myerson review the evaluation, diagnosis, and management of adult-acquired flatfoot deformity. Ans5
|
|

A 46-year-old obese female presents with foot pain and the radiographs shown in Figures A and B. Which of the following physical findings will most likely be present? 1. Achilles tendon contracture 2. Hallux varus 3. Forefoot adduction 4. Hindfoot varus 5. Clawing of the toes
|
The radiographs shown in Figures A and B demonstrate adult-acquired flatfoot deformity secondary to posterior tibial tendon dysfunction. Achilles tendon contracture will likely be present.In patients with this adult-acquired flatfoot deformity, the medial longitudinal arch collapses, the subtalar joint everts and the heel assumes a valgus position. As a result of the hindfoot valgus, the Achilles tendon is held lateral to axis of rotation of subtalar joint and begins to act as an evertor of the calcaneus. Untreated deformity can lead to a fixed equinus deformity of the hindfoot and an Achilles tendon contracture. Figure A demonstrates an adult-acquired flatfoot deformity. Note the uncovering of the talar head on the AP radiograph, and decreased distance between the medial cuneiform and floor on the lateral radiograph indicating collapse of the medial longitudinal arch. Ans1
|
|
|
60 yr obesity F c/o medial ankle/foot pain & weakness is seen early, progressive loss of arch PE=pes planus, "too many toes" sign ROM unable to perform single-limb heel rise, flexible.1-KIF(key image finding) -->Dx & classification1.1 SxF w/Dx & PEFw/Dx1.2 pathoantomy1.3image findings AP/ wb Lat1.4 DDX PTTI w/ pes planus2-If PE/xray/deformity, description of class then ____-Tx3-Complication & Prevention (DDx)
|
1-KIF-AP/LAt=r/o >40% talonavicular uncoverage vs subtalar DJD vs talar tilt of ankle mortiseDx->PTTI, 2B1.1 Sx=med ankle/foot pain & weakness early-> progressive loss of arch->lat ankle pain due to subfibular impingement late sxPE=pes planus=collapse of the med long arch, hindft vlgs +/-flex, too many toes" sign=foreft abd, tender just post to tip of med mall, assoc w/ equinus contrctr, +/-single-limb heel rise, flex/fix1.2 tendon degen -> watershed region distal to the med mall -> tenosynovitis & prog-> tendinosis w/ incompetent, painful tend w/NO excursion1.3 AP-increased talonavicular uncoverageincreased talo-first metatarsal angwb Lat=increased talo-1st MT ang, decr calcaneal pitch, decr med cuneiform-floor ht, subtalar arthritis MRI-tendon degeneration and arthritic changes in the talonavicular, subtalar, and tibiotalar jointsUS-increasing role in the evaluation1.4 DDX-midfoot path (OA or chronic Lisfranc injury) vs incompetence of the spring lig tx-recon
|
|
|
2-Tx of PTTI--stage & surgical treatment2.0 Most effective brace?2.1-If (+) single-leg toe raise + No deformity + xray=Nl 2.2-if flexible pes planovalgus deformity (can't do) single-leg heel raise + hindfoot valgus + Flex + too many toes-NOT present + xray=Arch collapse deformity2.3 painful flatfoot + unable to perform a single-heel rise & hindfoot was passively correctable2.4- unable to perform a single-heel rise+ rigid flatfoot, Subtalar arthritis2.5-rigid hindfoot, Talar tilt in ankle mortise, talotibial ankle joint is also arthritic2.6 equinus contracture
|
2.0=AFO found to be most effective, ex=Arizona brace is a molded leather gauntlet that provides stability to the tibiotalar joint, hindfoot, and longitudinal arch2.1. stg 1->immobilization in walking cast/boot for 3-4 months, custom-molded in-shoe orthosis, AFO family of braces (Arizona, molded, articulating) 2.2 stg 2A =medializing calcaneal osteotomy, 2.3 stge 2B=Lateral column lengthening, medializing calcaneal osteotomy, and FDL transfer to the navicular2.4stg3 = Triple arthrodesis=Arthrodesis of calcaneocuboid, talonavicular, and subtalar joints 2.5 stg4 =tibiotalocalcaneal arthrodesis and +/-TAL2.6 tendoachilles lengthening TAL
|
|
|
1-CC of ACL reconstruction failure?2-_____ works synergistically w/ the PCL to control ER, varus, and posterior translation 3-____is primary restraint to varus stress at 5° (55%) and 25° (69%) of knee flexion4- grade 3 PLC injury def=? if dial test > 10° external rotation asymmetry at 30° then ___? varus laxity at 30° indicates ____injury 5-indicated in patients with varus mechanical alignment___, arcuate fracture?6-assoc injuries w/PLC injury, what is the (most anterior structure inserting on the fibular head7-inserts on the posterior aspect of the fibula posterior to LCL, varus laxity at 0° indicates___?
|
1-missed PLC-Posterolateral Corner Injury 2-popliteus3-LCL 4->10mm of lateral opening and severe ligament disruption and no endpoint, isolated PLC injury , only LCL 5-HTO, avulsion fracture of the fibula6-peroneal n=N inju, LCL7-biceps femoris, both LCL & cruciate (ACL or PCL) injury
|
|
|
A 24-year-old male is involved in a motorcycle accident and sustains a right knee injury. Physical examination manuever performed at 30 degrees of knee flexion is shown in Figure A. Which of the following correctly describes the normal anatomic orientation of the region injured in this patient? 1. Popliteus inserts proximal to the LCL on the femur 2. Posterior oblique ligament originates from the adductor tubercle, just posterior and proximal to the medial collateral ligament 3. Biceps femoris inserts posterior to the LCL on the fibular head 4. Popliteofibular ligament inserts lateral to the LCL on the fibular head 5. Deep medial collateral ligament has both meniscofemoral and meniscotibial ligaments
|
pt has sustained a posterolateral corner (PLC) injury. Posterolateral subluxation of the lateral tibial plateau (Dial test) at 30° but not 90° indicates an isolated PLC injury, while subluxation at both 30° and 90° =PLC & PCL injury. The MRI is an example of a PLC injury. The iliotibial band (black arrow), lateral collateral ligament (asterisk), and popliteus (white arrow) are all injured. The coronary ligament (black arrowhead) is torn from the tibia, causing displacement of the lateral meniscus (plus sign). The biceps femoris inserts posterior to the LCL as shown in Illustrations B and C. The long head of the biceps femoris muscle has two main parts. A direct arm inserts onto the posterolateral aspect of the fibular head, and an ant arm crosses lateral to the LCL & inserts on the lateral aspect of the fibular head. short head of the biceps femoris has a direct tendon insertion onto the superior surface of the fibular head, med&post LCL insertion. Ans3
|
|
|
Which of the following best describes the anatomic relationships of the lateral collateral ligament in the posterolateral corner? 1. inserts directly anterior to popliteofibular ligament on the fibula and courses deep to popliteus 2. inserts anterolaterally to popliteofibular ligament on the fibula and courses superfical to popliteus 3. inserts posteromedially to popliteofibular ligament on the fibula and courses deep to popliteus 4. inserts directly posterior to popliteofibular ligament on the fibula and courses superficial to popliteus 5. inserts posterior and distal to biceps femoris tendon on the fibula and courses superficial to popliteus
|
The lateral collateral ligament originates on the lateral femoral condyle proximal to the insertion of the popliteus, runs superficial to popliteus, and inserts anterolaterally to the popliteofibular ligament on the fibula. The posterolateral corner (PLC) of the knee has received much attention as a restraint to control external rotation and posterior translation of the tibia in conjunction with the PCL. Injuries to the PLC rarely occur in isolation, less than 5% of the time. LaPrade et al performed anatomic dissections on 10 cadavers and provide a detailed description of the anatomic attachments of the PLC components, with the goal of helping guide surgeons performing anatomic reconstructions of an injured PLC. They found the lateral collateral ligament was the most anterior structure inserting on the fibular head. Stannard et al found that initial success rates of direct repair of the PLC were significantly inferior to early reconstruction. Ans2
|
|
|
A soccer player sustains a knee injury. He is noted to have a significant increase in tibial passive external rotation both at 30 and 90 degrees. Which of the following structures is least likely to be injured? 1. Fibular collateral ligament tear 2. Popliteus tendon tear 3. Posterior cruciate ligament tear 4. Arcuate ligament tear 5. Posterior oblique ligament tear
|
The posterior oblique ligament is a structure on the medial aspect of the knee. The fibular collateral ligament (also known as lateral collateral), Arcuate ligament, and popliteus tendon are all components of the postero-lateral corner (PLC). A positive dial test at 30 degrees indicates an isolated PLC injury, while a positive dial test at 30 and 90 degrees indicates PLC and concurrent posterior cruciate ligament (PCL) injury. Ans5
|
|
|
Which of the following injury patterns is most appropriately managed with an immediate postoperative physical therapy regimen that includes no active flexion but does allow active extension from 90 to 0 degrees? Topic Review TopicQID: 12101. Patellar tendon repair 2. Anterior cruciate ligament reconstruction 3. Anterior cruciate ligament reconstruction with medial collateral ligament repair 4. Anterior cruciate ligament reconstruction with posterolateral corner repair 5. Posterior cruciate ligament reconstruction with posterolateral corner repair
|
A postoperative physical therapy regimen consisting of no active flexion and active extension from 90 to 0 degrees is most appropriate for a combined PCL and posterolateral corner injury. The first 4 weeks often consist of hinged knee bracing and crutches with partial weightbearing to allow the posterolateral corner to heal along with quadriceps exercises (quad sets and straight leg raises). Active knee flexion is avoided in the immediate postoperative period as hamstring contraction has the potential to subluxate the tibia posteriorly and compromise the repair. Ans5
|
|
|
A 20 year-old male football player sustains a knee injury after being hit below the knee while blocking. You suspect a posterolateral corner (PLC) injury, but are also concerned about a posterior cruciate ligament (PCL) tear. Which of the following positive exam findings is indicative of a combined PLC and PCL injury? 1. Positive Dial test at 30 degrees of flexion 2. Valgus stress test opening at 0 and 30 degrees of flexion 3. Positive Posterior drawer test 4. Positive Pivot shift test 5. Positive Dial test at 30 and 90 degrees of flexion
|
A combined posterolateral corner (PLC) and posterior cruciate ligament (PCL) injury is most likely suggested by a positive dial test at 30 and 90 degrees of knee flexion.The Dial test may be performed prone or supine and is tested at 30 and 90 degrees of knee flexion. The test is positive if there is an increase in tibiofemoral external rotation by 10-15° compared to the contralateral side. A postive test at 30 degrees that is normal at 90 degrees indicates an isolated PLC injury. A postive test at 30 and 90 degrees indicates a combined PLC and PCL injury. Ans5
|
|
|
footballer s/p blow to anteromedial knee, Sx=difficulty with reciprocating stairs, pivoting, and cutting, PE=gait exam varus thrust or hyperextension thrust, external rotation recurvatum & c/o altered sensation to dorsum of foot and weak ankle dorsiflexion.1.1 Sx/Dx & PEF/Dx1.2 MoI2-If PE/xray/deformity then classif____-& Tx:::Rehab/Time 2.1-If > 10° external rotation asymmetry at 30° only consistent with isolated PLC injury & varus laxity at 30° indicates LCL injury then the Tx is______2.2 IF-If > 10° external rotation asymmetry at 30° & 90° consistent with PLC and PCL injury & varus laxity at 0°3-Complication (3)
|
1.1 Sx=often have instability symptoms when knee is in full extensionPE=gait exam=varus thrust or hyperextension thrust, varus laxity at 30° indicates LCL injury, > 10° ER asymmetry at 30° only consistent with isolated PLC injury, external rotation recurvatum positive when lower leg falls into external rotation and recurvatum when leg suspended by toes in supine patient; posterolateral drawer test performed with the hip flexed 45°, knee flexed 80°, and foot is ER 15°1,2-MoI=blow to anteromedial knee, varus blow to flexed knee, contact and noncontact hyperextension injuries, knee dislocation2.2 then PLC repair/reconstruction, & PCL reconstuction, 3-ArthrofibrosisMissed PLC injuryfailure to identify a PLC injury combined with an ACL injury will lead to failure of the ACL reconstructionPeroneal nerve injury
|
|
|
1-what abnormal blood____ level should alert the physician to the possibility of steroid use in an athlete affects heart. 2-irreversible effects of steriods3-has a catabolic effect on skeletal muscle ?4-MCC w/creatinine? 5-MC behavioral side effects are agression, hostility, and violence with the medication?6-no widely accepted urine test to detect the use of which of the following performance-enhancing drugs?
|
1- decreased levels of HDL or "good" cholesterol, increased levels of LDL or "bad" cholesterol, 2-alopecia (irreversible), irreversible deepening of female voice3-glucogon4-dehydration & muscle cramping5- Stanozolol-synthetic anabolic steroid derived from dihydrotestosterone, a class of performance enhancing drug taken to increase muscle mass and strength, reduce recovery time, and decrease muscle catabolism. 6-hum growth hormone
|
|
|
Which of the following is a side-effect from anabolic steroid use? 1. Liver damage 2. Decrease in low density lipoprotein 3. Decreased blood pressure 4. Decrease in fat 5. Decrease in high density lipoprotein
|
Anabolic steroids decrease high-density lipoprotein levels. They may either increase or have not effect on low-density lipoprotein levels and are not proven to cause liver damage. Elevations in blood pressure have been observed in athletes who use anabolic steroids. They do not appear to decrease fat mass. Abnormally low high density lipoprotein levels may suggest steroid use in an athlete. Ans5
|
|
|
A 32-year-old professional cyclist suffered a heart attack 6 months ago secondary to long term anabolic steroid use. What is the mechanism by which steroids most likely caused this patient's heart disease? 1. Increased blood hematocrit causing cardiac overload 2. Direct myocyte apoptosis 3. Alteration of plasma levels of low density lipoproteins 4. Alteration of myocardial conduction patterns 5. Direct endothelial damage to coronary arteries
|
Anabolic steroid use causes decreased levels of HDL or "good" cholesterol, increased levels of LDL or "bad" cholesterol, and liver toxicity, along with a number of other side effects. Cases of acute myocardial infarction in steroid users are related to this change in plasma levels of low density lipoproteins which alters cardiac blood flow. Ans3
|
|
|
1-mn for gout x22- primary gout due to?3-podagra aka?4--Which of the following foot radiographs is most consistent with the diagnosis of gout?
|
1-Pseduogout crystals are: Positive birefringentPolygon shapedGout therefore is the negative needle shaped crystals. gouT classically strikes great Toe, and its hallmark is Tophi.BRAG = “blue right angle gout”. I.e. gouty urate crystals are negatively birefringent: blue when perpendicular to the plane of polarization.2-nucleic acid metabolism that leads to hyperuricemia and deposition of monosodium urate crystals in joints (a purine breakdown product3- (arthritis attacks of great toe)4-asymmetric polyarthropathy, well-defined erosions with sclerotic margins, overhanging bony edges and tophaceous formations.
|
|
|
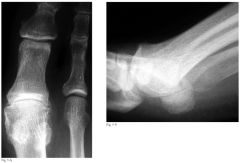
A 60-year-old man has had intermittent pain in his right great toe for the past 2 years. What is the most likely cause for the lesions indicated by the arrows in Figure A? 1. Monosodium urate crystal deposition 2. Calcium pyrophosphate deposition 3. Renal osteodystrophy 4. Tuberculosis 5. Sarcoidosis
|
Gout is a disorder of nucleic acid metabolism that leads to monosodium urate crystal deposition in the joints. The most common area of the body to be affected by gout is the first toe. The radiograph in Figure A demonstrates joint space narrowing of the 1st metarsalphalangeal joint and the arrows show medial soft tissue swelling at the 1st MTP with soft tissue radio-densities and some erosive changes consistent with gout. Incorrect Answers:Answer 2: Calcium pyrophosphate deposition is found with pseudogout and tophaceous depositions are rare in this disease.Answer 3: Renal osteodystrophy is a spectrum of disease seen in patients with chronic renal disease. It is characterized by bone mineralization deficiency due to the electrolyte and endocrine abnormalities associated with chronic kidney disease. It is a common cause of hypocalcemia, but does not present with the "tophi" seen in Figure A.Answer 4: Extrapulmonary manifestations of tuberculosis include CNS infection, Ans1
|
|
|
men 40, PMH of chemotherapy & renal stones, c/o pain in joint in toe PE=may have decreased range of motion due to pain & white toothpaste-like appearance of tophus aspirate1.1 Sx/Dx & PEF/Dx1.2 pathophysiology 1.3 labs2- Tx-acute gout attack? MoA2.1-chronic gout MoA 3-Prevention
|
1-Sx=pain in joint, can resemble septic arthritis, sx of renal stonesPE-may have decreased range of motion due to painwhite toothpaste-like appearance of tophus aspirate1.2 dysfunctional nucleic acid metabolism causing hyperuricemia, deposition of monosodium urate crystals in synovium of joint, crystals lead to an inflammatory response activating, proteasesprostaglandins, leukotriene B4, free oxygen radicals1.3-joint aspiration & crystal analysiscrystals are thin , tapered, needle shaped intracellular crystals, strongly negatively birefringent2-indomethacin (indocin), 50mg TID daily inhibits phagocytosiscolchicine=indicated in acute attacks if patient has a history of peptic ulcers, inhibits inflammatory mediators-Glucocorticoid-patient unable to take NSAID or colchicine2.1-allopurinol- xanthine oxidase inhibitor3colchicine-prophylaxis after recurrent attacks
|
|
|
1-CC of ST mass in children assoc w/ meniscal tears, why?2- where is child cyst located in knee bt/which 2 muscles?3- tx of Popliteal Cyst in Children
|
1-no, herniation of post knee capsule and synovium2-semimembranosus & medial head of gastrocnemius 3-observation
|
|

A 10-year-old boy presents with a mobile, soft, and painless mass over the posteromedial aspect of his knee. MRI demonstrates a simple cyst. What is the most appropriate next step in treatment? 1. CT with intravenous contrast 2. Bone scan 3. Radical excision 4. Arthroscopic resection 5. Observation
|

The description of the mass (soft and non-tender, in the posterior knee) in a young patient suggests that this is a popliteal, or Baker’s, cyst. The article by Dinham reviewed the natural history of 120 cases of popliteal cysts in children and reported that, of seventy untreated cysts, fifty-one disappeared spontaneously during a mean period of one year and eight months. The article also noted that those cysts which fail to regress spontaneously may respond to aspiration, but have a high recurrence rate. Given the lack of symptoms and the likelihood of resolution, observation is the first-line treatment for most popliteal cysts. Ans5
|
|

child c/o mobile, soft, and painless mass over the posteromedial aspect of his knee.1- PEF -->Dx1.1-KIF(key image finding) 1.2 Pathoanatomy2-Tx
|

1-mass will transilluminate1.1-MRI simple cyst & US1.2-semimembranosus & med head of gastruc 2-observation
|
|

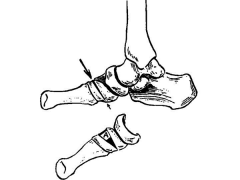
1-Transverse instability of the Lisfranc joint is the result of injury to ___?, MoI (3) def lat column of midfoot?2-what causes the Lis franc lig to tighten? is there direct lig attachment between 1st and 2nd MT3- which tarsometatarsal lig are weakest plantar or dorsal, clinical significance?4-5 critical radiographic signs that indicate presence of midfoot instability, on all 3 views5-fleck sign6-nonop candidates for lisfranc inj? MMComplic7-purely ligamentous arch injuries of lisfranc how to Tx in non athlete?***
|

1-both interosseous 1st cuneiform-2 MT lig & plantar ligament bt/ 1st cuneiform & 2nd & 3rd MT MoI=indirect rotational forces, axial load ->hyperplantar flex foreft; 4 & 5 TMT joints2-prontn & abd foreft: no3-dorsal, bony displacement with injury is often dorsal must Tx surgically4-(1)AP-disruption of the continuity of a line drawn-> med base 2nd MT to the med side of the mid cuneiform(2)AP-widening of the interval bt/ 1st & 2nd ray(3)oblique view=med side base of the 4 MT does not line up w/med side of cuboid (4) lat = MT base dorsal subluxation (5)lat=disruption of the med column line (line tangential to the medial aspect of the navicular and the medial cuneiform)5-bony fragment (fleck sign) in 1st interMT space, represents avulsion of Lisfranc lig from base of 2nd MT6-nonambul pts, presence of serious vascular dzsevere peripheral neuropathy, instability in only the transverse plane, <2mm MCC-posttraum arthts7-***Open red & arthrodesis med 2TMT jnt
|
|

40yo M sustains a R foot injury after a head-on motor vehicle collision. He is unable to place weight on the foot to ambulate, and pain is exacerbated with abduction of the midfoot. He is neurovascularly intact in the foot. An injury radiograph is shown in Figure A, while a clinical image of the foot is shown in Figure B. What is the most appropriate next step in management? 1. Open reduction and arthrodesis of the medial two tarsometatarsal joints 2. External fixation of the foot followed with staged open reduction and screw fixation across the medial two tarsometatarsal joints 3. Open reduction and screw fixation across the medial three tarsometatarsal joints and percutaneous pinning of the 4th and 5th tarsometatarsal joints 4. Debridement of Morel-Lavallee lesion and external fixation of the foot followed with staged open reduction and screw fixation across the medial two tarsometatarsal joints 5. Open reduction and screw fixation across the medial two tarsometatarsa
|

he history, clinical images, and radiographs are consistent with a Lisfranc injury. Instability of the Lisfranc joint is the result of injury to both the interosseous first cuneiform-second metatarsal ligament (Lisfranc's ligament) and the plantar ligament between the first cuneiform and the second and third metatarsals. They concluded that primary arthrodesis of the medial two or three rays has a better short and medium-term outcome than ORIF.Ans1
|
|

A 24-year-old man sustains an injury to his left foot. Stress radiographs are seen in Figure A. Injury to which ligament or ligaments are needed to produce the transverse instability seen here? 1. Spring ligament and bifurcate ligament 2. Interosseous first cuneiform-second metatarsal ligament 3. Interosseous first cuneiform-second metatarsal ligament and plantar ligament between the first cuneiform and the second and third metatarsals 4. Bifurcate ligament and Interosseous first cuneiform-second metatarsal ligament 5. Long plantar ligament and plantar ligament between the first cuneiform and the second and third metatarsals
|
Transverse instability of the Lisfranc joint is the result of injury to both the interosseous first cuneiform-second metatarsal ligament (Lisfranc's ligament) and the plantar ligament between the first cuneiform and the second and third metatarsals. Figure A shows a ligamentous Lisfranc injury.Kaar et al performed a cadaveric study in which sequential sectioning of the Lisfranc ligament followed by the plantar ligament between the first cuneiform and the second and third metatarsals was performed in order to simulate a low energy Lisfranc injury with transverse instability . Stress abduction radiographs were positive for all specimens in which both ligaments were sectioned, while sectioning of just the Lisfranc ligament was positive for only one specimen. Incorrect answers: The other options would not lead to a Lisfranc injury with transverse instability. Ans3
|
|
|
football players injuries his foot while being tackled. c/o severe pain in foot, inability to bear weight PE= medial plantar bruising, swelling throughout midfoot, tenderness over tarsometatarsal joint, grasp metatarsal heads and apply dorsal force to forefoot while other hand palpates the TMT joints produces instability. 1KIF(key image finding***) -->Dx?1.1 other images?1.2Sx/Dx & PEF/Dx1.3 MoI2-If PE/xray/deformity then Tx____ &post op rehab2.1 If no displacement on WB & stress xray & no evidence of bony injury on CT then the Tx is______? 4 types of pts2.2 indications open reduction and rigid internal fixation? rehab2.3 indications primary arthrodesis of the first, second and third tarsometatarsal joints2.4-indications -midfoot arthrodesis2.5-if grossly unstable and in presence of significant soft tissue swelling consider early external fixation3-MCComplication (2)
|

1-AP/lat/obliq:ft, stress xrays,WB xrays w/comparison lat=r/o dorsal displac prox base 1st or 2nd MTAP=malalignment med margin 2nd MT base & med edge of the mid cuneiform, r/o ***(fleck sign) in 1st interMT spaceobliq=malalignment 4th MT & cuboid1.1-CT scan= dx & preop MRI-r/o purely lig inj1.2-sx=severe pain &inability-.WBPEF-provocative tests-may reproduce pain w/pron & abd->forefoot & r/o instability test, always check for cmprt synd1.3 MoI=hyperflex/comprssn/abd moment ->foreft & transmitted to the TMTjnt2.1-SLC x 8 wks, certain nonop pts: nonambul pt, serious vascular dz, severe peripheral neuropathy, instability in only transverse plane2.2-ORIF:I=any evidence of instability (> 2mm shift) R-advance ->WBAT @ 8-10 wks RTS 9-12 mth2.3 1^fusion of 1,2,3 TMT jnt:I=pts w/ any evidence of instability, purely lig arch injuries R-NWB x 6 wk then WBAT @ 12 wks2.4-chrnc Lisfranc inj w/ advan midft DJDR:TTWBx6->10w2.5-ex-fix wait 2-3 wks 3-Posttrmtc OA, Nonunion
|
|

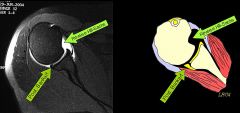
1-MC inj w/seizures and electric shock, r/o ***on xray, MC nerve injury w/ SAS for post dislocation2-(7) associated Lesions Associated with Posterior Instability of shoulder-3 bony 4 ST3-primary restraint->IR, primary dynamic restraint-ER, primary stabilizer to posterior subluxation w/shoulder in flex/abd/IR4-locked in an IR position=DX?mn hum vs labrum5-which 2 PE provocative test have a 97% sensitive for posterior labral tear?6-acute treatment of Post dislctn of shoulder?7-what is the McLaughlin procedure,indications & define, CI in SAS
|

1-post shoulder dislocation, r/o fx of lesser tuberosity MUST get axillary lat; axillary nerv I2(3) bony-Post glenoid rim fx, Lesser tuberosity fx, Reverse Hill-Sachs (hum)(4)-ST-Large capsular pouch, Posterior labral cyst, Posterior Bankart Lesn=Labrum, Avulsion of posterior band of IGHL 3-IR-posterior band of IGHL, ER-subscap4-posterior disloctn5-jerk=apply an axial force along axis of hum & add the arm to a forward-flex position, a ‘clunk’ is positive for post subluxation & kim test=flex shoulder -> 45 FF while simultaneously applying axial load elbow & post-infer force on the upper hum. test is (+) when pain is present6-acute redctn & immobilization ER x 4-6 wks7-chronic dislocation < 6 mths & reverse Hill-Sachs defect < 50%=open reduction with subscapularis and lesser tuberosity transfer to the defect CI=thermal shrinkage of capsule
|
|

Which of the following patients may benefit from a lesser tuberosity transfer (modified McLaughlin procedure)? 1. A kidney transplant recipient with AVN of the humeral head 2. A patient with severe rheumatoid arthritis 3. A young man with a locked posterior dislocation following an electric shock injury at work 4. A patient with a history of previous shoulder surgery that now has subscapularis insufficiency 5. A patient with a large Hill-Sachs defect following an anterior shoulder dislocation
|

Forceful posterior glenohumeral dislocations such as those resulting from seizures or electric shock may sustain a large reverse Hill-Sachs defect resulting in persistent instability in internal rotation or a locked posterior dislocation. These patients may benefit from having the lesser tuberosity along with the subscapularis advanced into the bony defect on the anterior humeral head (modified McLaughlin procedure). The original description by McLaughlin involved transferring the subscapularis tendon into the defect, and was later modified and popularized by Neer who recommended transferring the lesser tuberosity with the subscapularis. Incorrect Responses:None of the other patients meet the accepted indications for this stability procedure. 1. & 2. May benefit from other procedures such as a shoulder arthroplasty.4. May benefit from subscapularis repair or pectoralis tendon transfer to restore function.5. A Hill-Sachs defect is on the pos sup aspect of the humeral headAns3
|
|

Posterior glenohumeral dislocations are as common as anterior dislocations in which of the following patient groups?1. Football players 2. Marfan's syndrome patients 3. Renal failure patients 4. Epilepsy patients 5. Women
|
Millett et al and Robinson et al provide review articles on posterior shoulder dislocations, which are rare clinical entities that occur during seizures and electrocution (due to tetanic muscle contraction) or as a result of high energy trauma. Robinson et al noted that poor prognostic factors associated with posterior shoulder dislocation include late diagnosis, large bony defect of humeral head, associated proximal humerus fracture, and need for arthroplasty. In Gerber's series, posterior dislocations occurred with equal frequency to anterior in a cohort of epilepsy patients. Ans4
|
|
|
adult female c/o left shoulder pain and decreased range of motion 7 months after a fall onto her left side. PE= prominent posterior shoulder and coracoid, marked decrease in ER.1-KIF(key image finding) -->Dx 1.1 Sx/PMH=>Dx & PEF + (4)provocative test=>Dx1.2 MoI1.3 other images2-indications for Tx & Rehab/Time 2.1 If acute traumatic posterior dislocations then the Tx is______ & rehab2.2 if recurrent posterior shoulder instability then Tx=2.3 if chronic dislocation < 6 m & rev Hill-Sachs defect < 50%2.4 if chronic dislocation > 6 months old, reverse Hill-Sachs defect > 50%, severe humeral head arthritis2.5 if chronic dislocation > 6 months old, significant glenoid arthritis3-MCComplication & Cmn com
|

1-axillary lat=post dislocation, optionalVelpeau view if pt is unable to abd arm-> axillary1.1seizures and electric shock, 50% ER=undx'dPEF-locked in IR position, prominent post shoulder & coracoidposterior load & shift test, jerk=apply an axial force along axis of hum & add the arm to a FF position, a ‘clunk’ =(+) for post sublxn & kim test=flex shoulder -> 45 FF while simul applying axial load elbow & post-infer force ->uppr hum. test is (+) when pain is present, posterior stress test1.2MoI=flex/add/IR arm->high-risk pos1.3-CT-r/o bone loss in chrnc dislctn, MRI-r/o RCT2.1 acute dislo= immob ER x 4-6 wks then p/ 6 wks adv PT (rotator cuff strengtg & periscapular stabil & activity mod (avoid place arm in high-risk posi)2.2 recur dilsc=SAS w/ pos labral repair (Bankart) & capsular shift 2.3 chr<6 mth & <50%=Opn Redc w/ subscap & lesser tub transfer ->defect (McLaug2.4-chr>6 & >50=hemi2.5 TSA3MCC-recur; CC-adhes, stff, over tighting, axillry/supras merve
|
|
|
1-internervous plan of poster approach to hip?2-name of approach w/more extensile exposure used for complicated acetabular work?3-gluteus maximus innervation art & Nerve? at risk during release of glu max4-benefits of mini-incision approach in hip function?5-______ the hip to place the short external rotators on stretch 6-reflect backwards to protect sciatic nerve & maneuver of protect the nerve
|
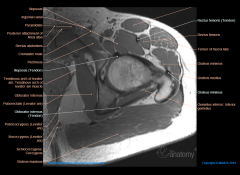
1-none2-Kocher-Langerbeck3-inf gluteal nerve & sup gluteal artgm-First perforating branch of profunda femoris4-mini-incision approach shows no long-term benefits to hip function 5-IR 6-detach piriformis & obturator internus close to femoral insertion, extend hip and flex knee to prevent injury
|
|
|
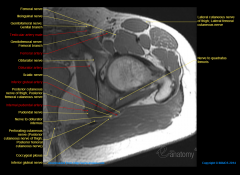
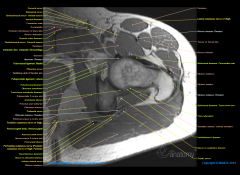
6-(7)structures at risk & how to protect mn7- complications& how to asses potential complications-PE-prov/motor/neuro;images;other8-cross sectional anatomy cartoon
|
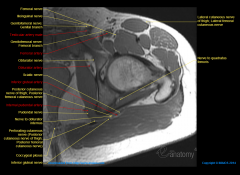
6-(1)Sciatic N->initially located along post surface of quadratus fem M:::prevtn=ext hip & flex knee to prvnt inj(2)Infr gluteal A->leaves below piriformis if cut and retracts into pelvis, flip patient, open abdomen, and tie off internal iliac artery(3)First perforating branch of profunda femorisduring release of gluteus maximus insertion(4)Fem vessels @ risk w/ failure to protect ant aspect of acetblm: prot placement of retractors ant to iliopsoas(5)Sup gluteal A & N-leaves the pelvis above the piriformis and enters the deep surface of the gluteus medius.(6)Quadratus fem=excessive retraction & injury must be avoided to prevent damage to Med Circ Art(7)Heterotopic ossification (HO)debride necrotic gluteus MINIMUS muscle to decrease incidence of HO
|
|
|
1-(5)Indications posterior approach to hip aka2-description of skin incision3-superficial dissection4-deep dissection5-objective of exposure and surgical approach
|
1-THA, hemi, removal of loose bodiesdrainage of septic hip, pedicle BG2-10 to 15 cm curved incision 1'' post to postr edge of grtr troch (GT)begin 7 cm above & post to GTcurve posterior to GT & continue down shaft of fem3-incise fascia lata to uncover vastus latrls distally lengthen fascial incision in line w/ skin incsnsplit fibers of glut max in prox incision cauterize vessels durg split to avoid excessive blood loss4-IR hip to place short ER on stretch place stay suture in piriformis & obturator; incise capsule w/ longit or T-shaped incsn dislocate hip w/ IR p/ capsulotomy5- Provides exposr->acetablm & prox fem
|
|
Where is the origin of the muscle located between the anterior acetabulum and iliac vessels? 1. Anterior superior iliac spine 2. Obturator foramen 3. Anterior inferior iliac spine 4. Pubic tubercle 5. Lumbar transverse processes
|

The psoas muscle serves to protect the iliac vessels from retractors/instruments anterior to the acetabulum, and this muscle originates off the transverse processes of L1-L5. The referenced article by Skaggs et el found that the iliac vessels were on average 1 cm away from the iliopsoas at the level of the pelvic brim, but could be as close as 4mm in children. They also found that the neurovascular structures were on average 3.1 cm away from the iliopsoas at the level of its insertion at the lesser trochanter. Ans5
|
|
The medial femoral circumflex artery and first perforating branch of the profunda femoris artery anastamose at which of the following locations? 1. Medial to the gluteus medius insertion 2. Medial to the gluteus maximus insertion 3. Anterior to the adductor magnus 4. Within the gluteus minimus muscle belly 5. Medial to the ischial tuberosity
|

The medial femoral circumflex artery is the primary blood supplier to the adult femoral head. This artery anastamoses with the first perforating branch of the profunda femoris just medial to the gluteus maximus insertion. This is important, as sectioning the gluteus maximus tendon during posterior approaches can put both of these vessels (and the anastamosis) at risk.ans2
|
|
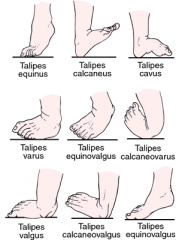
1-which bowing is physiologic? mn2-if PM bowing what is the assoc condition that affects the foot3-MC sequelae of posteromedial bowing is ___4-apex of deformity is ___w/ calcaneovalgus foot deformity?
|

1-PM-mn-Physiologic gone in Maturity 2-calcaneovalgus foot 3-PM-LLD 3-4 cm4-@ ankle
|
|
|
newborn w/apex of deformity is at the ankle & apex of deformity is in the distal tibia,1-KIF(key image finding) -->Dx & classification1.1 genetics1.2 MoI2-Tx2.1 If projected leg length discrepancy then the Tx is______3-Complication
|
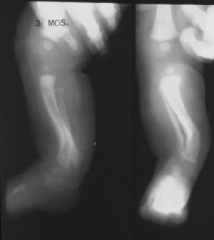
1xray-PM bowing=apex of deformity is in the distal tibia, calcaneovalgus foot deformity=apex of deformity is at the ankle1.1-none1.2-Physiologic bowing of tibia thought to be a result of intrauterine positioning2-observation2.1-age-appropriate epiphysiodesis of long limb3-2-5 cm leg length discrepancy at maturity
|
|

A 3-month-old child presents with the tibial deformity seen in Figure A. What foot deformity is commonly associated with this condition? 1. metatarsus primus varus 2. equinovarus 3. cavovarus 4. metatarsus adductus 5. calcaneovalgus
|

The radiographs show posteromedial bowing of the tibia and fibula, which is commonly associated with a calcaneovalgus foot deformity.Posteromedial tibial bowing is a form of physiologic bowing of tibia thought to be the result of intrauterine positioning. Treatment of this condition involves observation of the tibial deformity, which usually resolves at age 5 to 7. These patient often have a residual leg length discrepancy that may require further treatment.Ans5
|
|

An infant is born with a unilateral lower extremity deformity. A clinical photo is shown in figure A. Radiographs are shown in figure B. Which of the following conditions are associated with this type of deformity? |

The picture and radiograph demonstrate posteromedial tibial bowing which is thought to be a result of intrauterine positioning. While the tibial bowing deformity usually improves, a progressive leg length discrepancy develops which (like other types of congenital limb length inequality) remains proportional throughout growth. The ultimate difference ranges from 3 to 8 cm. Incorrect Answers:Answer 1: Knee instability is not associated with posteromedial tibial bowing but can be associated with other congenital femur, tibia, or fibula deficiencies.Answer 3: Pseudoarthrosis is associated with anterolateral bowing which is often seen with neurofibromatosis. Answer 4: Scoliosis is not associated with posteromedial tibial bowing.Answer 5: Tarsal coalition is associated with fibular hemimelia.Ans2
|
|

what is the most common cause of the adult acquired flatfoot deformity |
posterior tibial tendon insufficiency |
|

young male with mild pes planus may have what other 2 conditions |
seronegative spondyloarthropathy and inflammatory arthropathy |
|

posterior tibialis tendon
|
|
|
|
the patient has pes planus secondary to mid foot osteoarthritis for chronic Lisfranc injury what is the treatment |
midfoot fusion and realignment procedure |
|
|
if the patient has pes planus and an incompetent spring ligament in the absence of posterior tibialis tendon pathology what is the treatment |
Reconstruction spring ligament in addition to the standard flat foot reconstruction |
|

|
|
|

|
|
|

|
|
|
|
what is a triple arthrodesis |
|
|

|
|
|

|
|
|

A 58-year-old female with a history of acquired flatfoot deformity is taken to the operating room for surgical intervention. Representative radiographs are shown in Figures A and B. The position of the forefoot after the subtalar joint is aligned is shown in Figure C. What maneuver is indicated to prevent the development of weight-bearing based lateral border foot pain in this patient? Review Topic FIGURES: A B C QID: 4703
1. Dorsiflexion osteotomy of the medial cuneiform 2. Isolated talonavicular fusion 3. No further maneuvers are indicated 4. Derotation of the forefoot through the transverse tarsal joints 5. Derotation of the forefoot through the calcaneocuboid alone |
Plantarflexion opening wedge medial cuneiform osteotomy This patient has stage 3 posterior tibial tendon dysfunction. Derotation through the transverse tarsal joints is necessary to create a plantigrade foot and avoid lateral border foot pain. In stage 3 posterior tibial tendon dysfunction, there is degeneration of the subtalar, the talonavicular and the calcaneocuboid joints. The latter two joints compose the transverse tarsal joint. As the deformity progresses, abduction occurs through the transverse tarsal joints. Compensatory forefoot varus develops in an attempt to reestablish the mechanical tripod of the foot. The operative treatment of choice for stage 3 posterior tibial tendon dysfunction is a triple arthrodesis. After the subtalar joint is realigned, the forefoot varus will be unmasked if present. Derotation through the transverse tarsal joints as part of the arthrodesis procedure can address the forefoot varus and prevent lateral border foot pain. ans4 |
|

A 54-year-old female has a painful flatfoot that has not improved with over 8 months of conservative management with orthotics. Preoperatively, she was unable to perform a single-heel rise and her hindfoot was passively correctable. Figures Stage 2B posterior tibial tendon insufficiency.xrays left foot. She undergoes FDL tendon transfer to the navicular, medial slide calcaneal osteotomy, and tendoachilles lengthening procedures. Following these procedures, the appearance of the foot is demonstrated in Figure C. What is the next most appropriate intraoperative procedure to be performed during her foot reconstruction? 1. Dorsiflexion closing wedge medial cuneiform osteotomy 2. In-situ 1st-3rd tarsometatarsal joint arthrodesis 3. Plantarflexion opening wedge medial cuneiform osteotomy 4. Lateral column closing wedge shortening osteotomy 5. Subtalar arthrodesis |
The history, physical examination, and images are consistent with a Stage 2B posterior tibial tendon insufficiency. In acquired flat foot deformity, the hindfoot falls into valgus with compensatory varus developing in the forefoot. |
|

A 53-year-old female has a 20 month history of left hindfoot pain that has failed to respond to AFO bracing and physical therapy. She has a unilateral planovalgus deformity, shown in Figure A, which is flexible. She is unable to do a single leg-heel rise. Which of the following surgical options is most appropriate? 1. Triple arthrodesis 2. Isolated FDL transfer to the navicular 3. Dorsiflexion osteotomy of the 1st ray with peroneus longus-to-brevis transfer 4. Lateralizing calcaneal osteotomy with FDL to navicular transfer 5. Lateral column lengthening, medializing calcaneal osteotomy, and FDL transfer to the navicula |
he patient is presenting with Stage II posterior tibial tendon dysfunction (PTTD) as she is not able to do a single leg-heel rise (Stage 1 can do a heel rise) and has a flexible deformity (Stage 3 is not flexible). First line of treatment, regardless of stage, is non-operative. Operative management of Stage II disease is controversial, but there is a growing interest in combining bone procedures with tendon transfer to replace the incompetent PTT which relieves pain and corrects the underlying deformity. |
|
|
A 56-year-old woman comes to your office with foot pain after a 9 month trial of orthotics. Your examination reveals the hindfoot is in valgus, the arch is depressed, and the forefoot is abducted when the foot is viewed posteriorly. She is unable to perform a single heel rise on the affected side. The hindfoot is flexible and there is an equinus contracture. What combination of surgical interventions is most appropriate 1. Tenosynovectomy followed by UCBL orthotic use 2. Dwyer closing wedge calcaneal osteotomy, 1st metatarsal closing wedge osteotomy, and plantar fasica release 3. Medial calcaneal displacement osteotomy, FDL tendon transfer, and tendoachilles lengthening 4. Arthrodesis of the subtalar, talonavicular, and calcaneocuboid 5. Lateral calcaneal displacement osteotomy, FDL tendon transfer, and tendoachilles lengthening
|
This patient presents with a Stage 2B acquired flatfoot deformity. The review articles by Myerson and Pinney discuss the classification and management of adult acquired flatfoot deformity. Stage 1 presents with medial ankle pain due to posterior tibial tendon synovitis. Stage 2 presents with a hindfoot in valgus and inability to perform a single limb heel rise. Stage 2A has a normal forefoot whereas Stage 2B has an abducted forefoot, exposing “too many toes” when the foot is viewed posteriorly. Stage 3 occurs over time as the hindfoot becomes rigid in a valgus position and Stage 4 develops as the deltoid ligament becomes incompetent and the talus tilts into valgus. Tenosynovectomy can be used in Stage 1 disease that fails conservative management. Answer 2 is used as a treatment for cavovarus feet. Answer 4 is a treatment option for Stage 3 disease. Answer 5 is not an option as a lateral displacement calcaneal osteotomy would exacerbate the patient's hindfoot valgus. |
|
patient complains of shoe irritation of the 1st MTP joint physical exam positive with grinding test
|

|
|

|
|
|
|
patient injured his foot while being tackled in football this severe pain he is unable weight-bear physical exam positive for instability
|

|
|

A 40-year-old male sustains a right foot injury after a head-on motor vehicle collision. He is unable to place weight on the foot to ambulate, and pain is exacerbated with abduction of the midfoot. He is neurovascularly intact in the foot. An injury radiograph is shown in Figure A, while a clinical image of the foot is shown in Figure B. What is the most appropriate next step in management? 1. Open reduction and arthrodesis of the medial two tarsometatarsal joints 2. External fixation of the foot followed with staged open reduction and screw fixation across the medial two tarsometatarsal joints 3. Open reduction and screw fixation across the medial three tarsometatarsal joints and percutaneous pinning of the 4th and 5th tarsometatarsal joints 4. Debridement of Morel-Lavallee lesion and external fixation of the foot followed with staged open reduction and screw fixation across the medial two tarsometatarsal joints 5. Open reduction and screw fixation across the medial two tarsometatarsal joints with anatomic ligamentous reconstruction |

The history, clinical images, and radiographs are consistent with a Lisfranc injury. Instability of the Lisfranc joint is the result of injury to both the interosseous first cuneiform-second metatarsal ligament (Lisfranc's ligament) and the plantar ligament between the first cuneiform and the second and third metatarsals.an1 |
|

As an alternative to open reduction and internal fixation for the injury pattern seen in Figure A, what alternative treatment has been shown to be more effective? 1. open reduction and primary arthrodesis of the medial and middle column 2. open reduction and primary arthrodesis of the medial, middle, and lateral column 3. closed percutanous pinning 4. closed reduction and casting 5. partial weight bearing in removable boot |

The lateral radiographs shows a ligamentous Lisfranc injury. There does not need to be a fracture to be called a Lisfranc injury; and the ligamentous ones typically have even worse outcomes than similar fracture-type injuries. These uniformly have poor, painful outcomes if treated non-operatively because recurrence of the dislocation occurs without rigid bony fixation to allow soft tissues to heal. Typically, these have been treated with ORIF, but outcomes are often poor and many times the deformity recurs because the soft tissues may not heal strong enough to resist weight bearing forces, as compared to fractures which are strong once healed. ans1 |

