![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
15 Cards in this Set
- Front
- Back

Hx;56yo M presents to your office 1 yr p/undergoing THA with the implant Fig A. He is concerned about the potential complications given the recent media attention his implant has received. He is currently asymptomatic. Which of the following statements is accurate regarding his prosthesis and future care? 1-He should have bi-annual LFTs measured, as metal ions are metabolized by the liver; 2-His risk of developing CA is dramatically >; 3-There is no correlation between activity level and serum levels of metal ions; 4-His prosthesis design is safe in women of child-bearing age as the ions cannot be transmitted via pregnancy; 5-His prosthesis design puts him at an >risk for dislocation.
|

metal-on-metal (MOM) hip replacements it has been shown that activity level does NOT affect serum metal ion levels. It was found no correlation between patient activity and serum levels of cobalt or chromium, or urine levels of chromium., Incorrect answers:
1. Metal ions are excreted by the kidneys, and there is NOT currently a concern regarding liver function in patients with MOM hip replacements. 2. Increased risk for developing cancer has not been shown. 4. Metal ions are capable of placental transmission and therefore should not be used in women of child-bearing age. 5. Increased incidence of hip dislocation is not a known complication of MOM hip replacements. Ans3 |
|

Hx:80yoM has a Charnley all-polyethylene acetabular shell shown in Fig A. When defining failure as revision for any reason, what is the failure rate at 35 years for this type of prosthesis? 1. < 10% ; 2-20% to 30%; 3-40% to 50%; 4-50% to 75%; 5-> 75%
|

77.3% survivorship for the component at a mean of 21 years, with revision or definite loosening as an endpoint. Kavanaugh et. al, reported that the probability of surviving 20 years without revision of the components was 84%. They did note that there is a significantly increased probability of revision based on the age of the patient at the time of the index THA(27% for <59 y.o., 13% for 59-65 y.o., 7.5% for 65-70 y.o., and 12% for >70 y.o.)
Callaghan, et. al. has demonstrated the remarkable durability of cemented Charnley total hip replacements over a span of three decades, with 88% of the original prostheses intact at 20 years, and 78% at 35 years. In conclusion, the rate of revision definitely varies, but should be somewhere between 20-30%.Ans2 |
|

Hx:88yo F fell onto her R hip sustaining the fx Fig A. PMH=mild dementia and moderate CAD. At baseline =ambulates w/a walker. There are concerns about her ability to maintain WB precautions AFTER surgery. Which is most appropriate for management of the femoral side? 1-Non-op management; 2-orif w/plate and cerclage wires; 3=Proximal femoral replacement w/megaprosthesis; 4-Impaction BG; 5-Cortical strut allograft with cerclage wiring
|

Vancouver B3 periprosthetic fracture with poor proximal femoral bone stock. Given her age, co-morbidities, and dementia, the appropriate management of her condition would be a proximal femoral replacement with megaprosthesis or Revision to a long, porous coated femoral stem with biplanar allograft struts. This can allow for immediate weight-bearing in the post-operative period.
Incorrect Answers: Answer 1: Operative management is indicated to reduce pain and prevent complications associated with bedrest. Answer 2: Given the degree of proximal femoral bone loss and loose stem, open reduction and internal fixation with a plate is not the best option. Answer 4: Impaction bone grafting is an option for Vancouver B3 fractures, but are typically reserved for younger patients who have bone stock that needs to be restored, B3 periprosthetic fractures are fractures around or just below the tip of a loose stem with poor proximal femoral bone stock. Options for management of this fracture include a fully coated stem, a fluted tapered stem, a proximal femoral replacement with megaprosthesis, allograft-prosthesis composite, and impaction bone grafting. In elderly patients with co-morbidities and an inability to maintain the strict weight-bearing precautions that impaction bone grafting and allograft prosthetic replacements require, proximal femoral replacement with a megaprosthesis is the best option. Answer 5: Given the degree of proximal femoral bone loss and loose stem, cortical strut allograft with cerclage wiring is not the best option.Ans3 |
|

Hx:78yo F undergoes THA through a minimally invasive surgical approach. During insertion of a metaphyseal fixation stem w/cementless press-fit technique, a crack in the calcar is ID. The stem is removed, two cable wires are passed around the calcar, and the same stem is reinserted. Which of the following statements is true? 1-The pt should be advised she is > risk of stem subsidence and early revision; 2-Female sex is a risk factor for intraop calcar fx; 3-a better outcome would be expected if a long-stem diaphyseal fixation stem had been inserted p/ recognition of the calcar fx;
4-Cementless press-fit technique is not a risk factor for intraop fx; 5-Minimally invasive surgical approach is not a risk factor for intraop fx |

only true statement is that female gender is a risk factor for intraoperative calcar fracture, Studies have shown that successful outcomes can be achieved with stem removal, cable wiring of the calcar, and re-insertion of the primary stem, The authors report no femoral component subsidence or failure otherwise at 16 year follow-up, "Risk factors for intraoperative periprosthetic fractures include the use of minimally invasive techniques; the use of press-fit cementless stems; revision operations, especially when a long cementless stem is used or when a short stem with impaction allografting is used; female sex; metabolic bone disease; bone diseases leading to altered morphology such as Paget disease; and technical errors at the time of the operation." The authors summarize techniques for treatment and postulate that long term outcome is unaffected when the intraoperative fracture is identified and treated appropriately.Ans2
|
|

In 1st day home p/ undergoing a THA 65yo M falls down the stairs and sustains the fx seen in Fig A & B. What is the preferred treatment for this injury? 1-ORIF w/cables & proximal fem locking plate;
2-ORIF w/ allograft strut & multiple cables; 3- Revision femoral component with proximal fem replacement; 4-Revision fem component w/long stem diaphyseal press-fit stem; 5-Revision fem component w/cemented stem |

Vancouver B2 peri-prosthetic fracture with loose femoral stem. In Vancouver B2 periprosthetic femur fx it is recommended that the fx be stabilized with the use of an uncemented extensively porous coated fem component. However, in order to increase the fem strength similar to the contralateral side, the surgeon must bypass the most distal cortical deficiency by two cortices.Ans4
|
|

A periprosthetic acetabular fx is noted intra-op during THA. The acetabular component is stable and well-fixed after implantation of an ingrowth acetabular shell. Which of the following treatment options will best maintain motion and clinical function? 1-ORIF of the posterior column and THA revision; 2-Cage reconstruction of acetabular component; 3-THA revision using a cemented acetabular component; 4-Placement of a hip abd brace and NWB; 5-No change in tx;
|

Acetabular fracture during total hip arthroplasty is a known complication that typically occurs during acetabular component impaction. If noticed intra-op, the stability of the component should be assessed by the surgeon to determine treatment. If the component is stable, no additional treatment is necessary. If the acetabular component is unstable, then it should be changed and/or supplemented with component screws until stability is obtained.Ans5
|
|

Hx:78yo M s/p SnF @t home 4 mth p/ R THA. PE=R leg deformity, pain, and inability to bear weight, He is neurovascularly intact. xray Fig A & B. The patient denies any prodromal groin pain prior to his fall. Which is the best treatment option? 1-Tx x 6 wks p/ by slow return to wb; 2-ORIF w/ a cable plate; 3- Revis to a long, cementless fem stem; 4-Revision to a long, cementless stem with strut allograft
5-Revision to a long, cemented stem |

Vancouver B1 periprosthetic femur fracture. The stem appears stable within the femur, and there is no evidence of subsidence with comparison to the initial post-THA radiographs. This fracture pattern is best treated with internal fixation. Periprosthetic fractures around a hemiarthroplasty should be treated with the same algorithm. However, if the patient had antecedent groin pain, then conversion to a total hip arthroplasty should be considered to prevent continued groin pain.Ans2
|
|

What percentage of patients with complete peroneal nerve palsy after total hip arthroplasty will never recover full strength? 1-90% to 95%; 2-60% to 65%; 3-40% to 45%; 4-20% to 25%; 5-0% to 5%
|
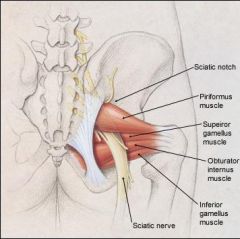
likelihood of complete functional recovery to preoperative strength levels is 35% to 40%, Nerve palsy is an uncommon but acknowledged complication of total hip replacement. The overall preval= 1%. The sciatic nerve, or the peroneal division of the sciatic nerve, is involved in nearly 80% of cases. The risk of nerve palsy in association with THA is >for female compared with male patients, with a DDH, and with pt = revision surgery. A preoperative diagnosis of developmental dysplasia of the hip or posttraumatic arthritis, the use of a posterior approach, lengthening of the extremity, and use of an uncemented femoral implant increased the odds ratio of sustaining a motor nerve palsy (in Farrell study). In the majority of cases, the origin of the palsy is unknown. Because peripheral nerves are sensitive to compression, unrecognized compression may play a role in these cases.Ans
|
|

In pts with SCD and asymptomatic ON of the femoral head identified with MRI, what % will eventually go on to femoral head collapse? 1. < 10%; 2. 11% to 25%; 3. 26 to 50%; 4. 51 to 75%; 5. > 75%
|

Untreated asymptomatic osteonecrosis of the femoral head in patients with sickle cell disease has a > 75% likelihood of progression to pain and collapse.
In contrast to asymptomatic osteonecrosis in patients without sickle cell disease, patients with sickle cell disease have a high incidence of progression to collapse and functional impairment secondary to pain (33% compared to 75%, respectively). In patients with sickle cell disease who present with a symptomatic hip, the contralateral (presumably asymptomatic) hip should be screened carefully and periodically for signs of disease. Given the high rate of progression, some argue for operative treatment of the asymptomatic hip at the same time the symptomatic hip is being treated. patients with sickle cell disease who had symptomatic avascular necrosis (AVN) in one hip and asymptomatic AVN in the contralateral hip. Their goal was to understand the natural history of the asymptomatic side. Ninety-one percent eventually developed pain and 77% developed collapse. Collapse was preceded by symptoms of pain in all patients.Ans5 |
|

A 65-year-old healthy patient fell 18 years after a THA and sustained the fx Fig A. What is the most appropriate tx? 1-Percutaneous locked plating; 2-ORIF with a cable plate and allograft strut; 3-revision to a long, porous coated femoral stem with biplanar allograft struts; 4-Revision to a cemented revision femoral stem that bypasses the fx site by 5 cm; 5- 3 mths of NWB
|

Vancouver classification of periprosthetic femur fractures is based on the fracture site, implant stability, and remaining bone stock. The patient in the question has a type B3 fracture. The cemented stem is loose and there is very poor remaining bone stock. He should be treated with a long, cementless revision stem with biplanar strut grafts. A tumor prosthesis or allograft-prosthesis composite would be alternate possibilities.Ans3
|
|

Hx:82yo f falls and sustains the fx fig A. She denies any hx of dislocation or prodromal pain prior to her fall. What is the tx? 1-TTWB; 2-ORIF w/a cable plate
3-Revision of the fem w/ a long, cementless stem 4-Revision of the fem w/ a long, cemented stem 5-Girdlestone resection arthroplasty |

The long spiral fracture is consistent with a loose implant. The bone stock is sufficient. Therefore, this fracture pattern would classify as a B2 using the Vancouver classification system. The Vancouver classification for periprosthetic femoral fractures is simple yet incorporates all the pertinent factors such a location, stem fixation, and bone stock. Type A is a trochanteric fracture- lesser or greater. These can be treated non-operatively usually and ORIF if symptomatic. Type B fractures are around or just below the stem and are subdivided into three types. Type B1 is a fracture with a well fixed stem. The treatment is cable plating or allograft struts or a combination of the two. Type B2 is a fracture with a loose stem with good bone stock. The treatment is a cementless porous coated long stem atleast two diameter length past the fracture site.Ans 3
|
|

Hx;67yo M who underwent THA 4 yrs ago fell on to his R hip. His pre-injury right hip film Fig A; current fx= Fig B and C. Prior to the fall he had no thigh or hip pain. His ESR and CRP are within normal limits. During intraop assessment, the acetabular and femoral stems are found to be well fixed. What is the next best course of action? 1-Revision of the acetabular component and ORIF of the femur with locking plates and cerclage wires; 2-Revison of the femoral component, bypassing the fx by 2 cortical diameters; 3-Revision of the fem component w/ impaction grafting and cerclage wires; 4-Revision to a cemented component, bypassing the fx by 2 cortical diameters; 5-ORIF of the fem w/ locking plates and cerclage wires
|

The patient in the scenario has well-fixed femoral and acetabular components with a fracture at the level of the implant extending to tip. This corresponds to a Vancouver B1 fracture. Treatment for B1 fractures is open or closed reduction, followed by internal fixation with locking plates.Ans5
|
|
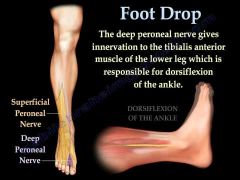
Hx:67yo F s/p THA Postop, she c/o complete peroneal palsy that does not improve with flexion of the knee and removal of compressive dressings. All of the following are associated with a post-operative nerve palsy EXCEPT:1-DDH; 2-LL of the extremity; 3-Surgeon self-rating the procedure as being a difficult intervention; 4-AVN of the femoral head; 5-Posttraumatic OA
|
This patient has a motor and sensory (complete) peroneal nerve palsy. The incidence of postoperative nerve injury ranges from 0% to 3% and most often affects the peroneal branch of the sciatic nerve. Eggli et al reviewed 370 patients following total hip arthroplasty and found the only factor that correlated to nerve palsy was the surgeon self-rating the procedure as difficult potentially leading to direct or indirect mechanical trauma. Farrell et al reviewed 27,004 total hip arthroplasties and found that developmental dysplasia, extremity lengthening, posterior approach, posttraumatic arthritis, and uncemented femoral component increased the odds ratio of a nerve palsy. They found less than a 50% rate of nerve recovery.Ans 4
|
|
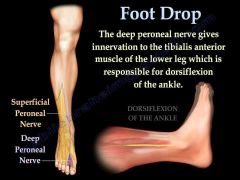
Risk factors for a motor nerve palsy following primary THA include all of the following EXCEPT? 1-DDH; 2-LLD; 3-Posttraumatic arthritis; 4-Obesity; 5-Posterior approach
|
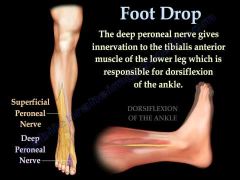
a hx of (DDH), limb lengthening, posttraumatic arthritis, cementless fem fixation, and the post approach, Body-mass index (BMI) was NOT assoc w/ >risk of nerve palsy, Of note, the average time to maximal recovery for both incomplete and complete nerve palsies was approx 2 ys. Pt should be counseled regarding this complication especially if one of the above risk factors is present. Ans4
|
|
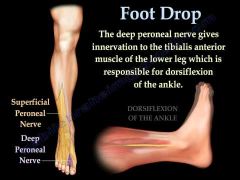
All of the following are risk factors for developing a sciatic nerve palsy following THA EXCEPT: 1-Fem gender; 2--DDH; 3-Revision surgery; 4-RA; 5-LL of the extremity
|
Female gender, DDH, Revision surgery, and extremity lengthening are all risk factor for the development of a post-operative sciatic nerve palsy following total hip arthroplasty. Rheumatoid arthritis is not a risk factor.Ans1
|

