![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
List and describe the different phases of mitosis |
Prophase:-chromosomes condense and themitotic spindle begins to form from centrosomes Prometaphase:- nuclear envelope breaksdown and the kinetochores of the mitotic spindle attach to thechromosomes Metaphase:- chromosomes are alignedat the equator in between the spindle poles and the kinetochoremicrotubules attach to single chromosomes Anaphase:- sister chomatids aresynchronously separated as they are pulled towards each of theopposing spindle poles – by the shortening of the kinetochoremicrotubules. The spindle poles also move further apart, helpingseperate the sister chomatids. Telophase:- the two sets ofchromosome arrive at each of the spindle poles and a nuclear envelopeforms around each of the sets. Cytokinesis: - a contractile ringformed of actin and myosin filaments pinches the centre of the cell,creating daughter cells with formed nuclei. |
|
|
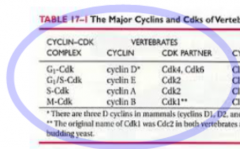
What are the main cyclins in the cell cycle? |
|
|
|
Describe how the cell cycle is regulated |
- mediated by the cellcycle control system which acts as a series of “molecular breaks”- controlled bycyclically activated kinases – Cyclin-Dependent Kinases (Cdks) - activation anddeactivation of Cdks is largely dependent on cyclins - named so attheir concentrations vary in a cyclical fashion - activity of Cdks isdependent on the formation of specific cyclin-Cdk complexes, andphosphorylation: there are three sites for phosphorylation. First, asight required for activity is phosphorylated, while the two othersites are dephosphorylated by a specific phosphatase (inhibitorysites). Another phosphatase then phosphorylates the two inhibitorysites, activating the cyclin-Cdk complex - active cyclin-Cdkcomplexes, in turn, phosphorylate other proteins, driving differentstages of the cell cycle |
|
|
Draw a diagram illustrating the activation of a CDK |

|
|
|
What is the importance of ubiquitin in the cell cycle |
-cyclin concentration rises slowly, but decreases abruptly -the abrupt decrease is due to targeted degradation of cyclins -this is achieved by specific enzyme complexes which add ubiquitinchains to the cyclins -this targets the cyclin for destruction: it is directed toproteosomes and destroyed by proteolysis-e.g. inactivation of M-Cdk (by the proteolysis of M-cyclin) drivesthe cell out of mitosis |
|
|
Define a mitogen |
a chemical substance that encourages a cell to commence cell division, triggering mitosis |
|
|
What is the importance of telomerase in carcinogenesis? |
-Telomerase is absent in most cells other than stem and germ cells. -As these cells replicate, telomeres positioned on the ends ofchromosome arms become progressively shorter. When the telomeresequences become sufficiently truncated, apoptosis is initiated. -The expression of telomorase prevents cell death, and thus enablesreplication to continue. These cells therefore become immortal, andare thus factors of uncontrolled replication - tumourogenesis. |
|
|
What are the two types of tumour supressor gene? |
- caretakersand gatekeepers. - Caretaker TSGs, such as BRCA1, BRCA2, andXP, maintain theintegrity of the genome by repairing damaged DNA. - Gatekeeper genes,such as p53, RB1 andAPC, inhibitproliferation or promote apoptosis of cells containing damaged DNA. |
|
|
what are the five types of oncogene? |
- growthfactors - growth factor receptors - signal mediators with tyrosinekinase activity - signal mediators with nucleotide binding activity - nuclear-binding transcription factors |
|
|
Give an example of a virus which can cause cancer and describe its pathology |
- HumanPapillomavirus (HPV) strains 16 and 18 are a leading cause ofCervical Intraepithelial Neoplasia (CIN) and cervical carcinomas. - The dsDNA virus is composed of three domains; a regulatory region, anearly region, and a late region. - The virus infects keratinocytes inthe basal layer of the cervical epithelium via microtrauma – suchas through sexual intercourse. - Entry is facilitated by the binding ofL1 receptors. The virus then replicates to ~50-100 copies per cell, anumber which is steadily maintained in dividing cells. However, aproblem for the virus is that it will only infect and replicate indifferentiated squamous epithelium, where the necessary cellular DNApolymerases and replication factors are not expressed. - whenthe host cell stops dividing and begins to differentiate into amature keratinocyte, there is an upregulation of all viral genes.Notable examples are Early region genes E6 and E7 and Late regiongenes L1 and L2. E6 binds p53 and E7 binds pRb – the product ofRB1.Both of these events inhibit their function as regulators ofproliferation and apoptosis - thus promoting an environment in whichthe virus is able to replicate, and conditions are suitable forcarcinogenseis. - The virus then replicates to >1000 copies percell, and the viralgenomes are then encapsidated by the coating proteins L1 and L2 -allowing release, subsequent re-infection, and metastasis. |
|
|
Give an example of a chemical carcinogen and describe the pathology |
- polycyclicaromatic hydrocarbons (PAHs) areprocarcinogens, meaning that they require metabolic conversion in thebody to become carcinogenic. - conversion occurstypically at that the site of entry - as conversion is enabled byoxidases, which are ubiquitous throughout the body. - Oxidases convertPAHs to polar hydroxy and epoxy derivatives. Epoxides are highlyreactive, and freely converted to compounds such as dihydrodiols,phenols, and various other chemically reactive intermediates. - Theformation of diol epoxides are considered the prominent carcinogenicand mutagenic molecules, They are easily converted to carbonium ions,(alkylating agents) which bind covalently to nucleophilic sites onDNA - Their direct interaction with DNA is ultimately the source ofaberration resulting in carcinogenesis. |
|
|
Describe how ionising radiation causes cancer |
- isa high-frequency electromagnetic wave. It is termed as ionising as ithas sufficient energy to displace electrons from its orbit around anucleus. Examples include X-rays and gamma rays. -Damage can occur to DNA either directly or indirectly. In the former,a displaced electron can hit and break DNA strands. In the latter, anelectron can react with a water molecule to produce a hydroxylradical – which then interacts with the DNA, also introducingstrand breaks by abstraction of deoxyribose hydrogen atoms. |
|
|
Describe how x-rays work |
- x-rays are ionisingradiation; part of the electromagnetic spectrum - x-rays are produced byheating a tungsten filamanet (the cathode) within a vacuum - electrons are releasedwhich are focused to an anode due to the potential difference (i.e.gradient). - bombardment of theanode with electrons causes the release of x-ray photons - most x-ray photons areabsorbed by the casing, but a small amount travel through the body toa photographic film/digital image system - an image is producedbased on the amount of x-rays which have reached film i.e. notabsorbed by the body |
|
|
Describe what can be sen with an x-ray |
- air: appears blackest(least absorbance) - fat: a lighter shade ofgrey than air - soft tissue/fluid: bothhave the same density e.g. you cannot differentiate between the heart muscle and theblood flowing through it - calcium (typically,bones) - metal: appear whitest(highest absorbance) |
|
|
What is an x-ray typically used for? |
- highly suitable forbones - also useful for organsin the abdomen e.g. liver and bladder - used for lung diseasese.g. pneumonia or lung cancer - mammography- x-ray fluoroscopy |
|
|
Describe how a CT works |
- similar to x-rays inthat it also uses x ray photons- differs from x-rays inthat there are multiple detectors (digtal image system) and arotating x-ray tube. - creates images sliceswhich can then be analysed to produced three dimensional,cross-sectional images. - axial is theconventional form of CT. In axial, the machine would rotate once360°, the patient would moveforward the width of the x-ray , and then the x-ray tube would rotatethe other. This would continue until the sufficient area had beencovered. - in helical/spiral CT,the x-ray tube moves continuously as the patient table moves throughthe machine. This technique is far more rapid, allowing the thorax tobe done in around 10 seconds. |
|
|
How can CT be enhanced? What is it used for? |
- contrast agents can be used to enhance differentiation; barium can be introducedrectally to enhance images of the gastrointestinal tract,iodine-based agents are typically introduced intravenously todifferentiate vessels. - good for showing bone,soft tissue and blood vessels |
|
|
How does an MRI work? |
- application of amagnetic field causes the protons in rotating hydrogen atoms to alignwith the magnetic field -a second magnetic field is then introduced in the form of a radiofrequency (RF) pulse, which disrupts alignment. When the RF signal isremoved, the hydrogens return to their original position. The energywhich is given off during this transition is detected and theirintensityis plotted on a grey scale to produce cross sectional images. -different tissues relax at different rates, allowing detailed imagesto be produced. One measurement is the time it takes for the hydrogenatom to return to its original location (T1), the other is the timeneeded for the axial spin to return to its normal position (T2). As arule, T1 images produce good anatomical detail, while T2 imagesproduce images more representative of the tissue type. |
|
|
What is MRI good for? |
- provides excellentcontrast of soft tissue and without the need for contrast - excellent for grey andwhite matter in the brain and lesions in the liver - like CT, can producecross-sectional images, though has higher resolution of soft tissuethan CT |
|
|
What are the disadvantages of MRI? |
- generally takes longerthan other radiological imaging. However, MRIs are becomingincreasingly quick, some even rivalling that of spiral CTs. - noisy - requires patient to bestill - not possible for somepeople due to presence of metal e.g. pacemaker |
|
|
How does ultrasound work? |
- an electromagneticfield changes the shape of piezoelectric crystals within a probe,releasing sound waves - the high frequencywaves enter the body, reflect of internal structure, and are thenscattered as they return to the probe - images are producedbased on the “echogenicity” of tissues: fatty tissues: brighterthan surrounding tissue; fluid: black - unlike most imagingtechniques, in that it is dynamic |
|
|
How does doppler ultrasound work? |
- sameprincipal as normal ultrasound i.e. reflection of sound waves - used in relation toblood flow e.g. occlusion - as the sound bounces offlowing cells it creates variation in pitch; this is used to createrepresentative graphs or pictures i.e. doppler shift |
|
|
What are the advantages and disadvantages of ultasound? |
Advantages - non-invasive andpainless - no contrast needed - useful diagnosingdisease in multiple areas e.g. abdomen (e.g. pregnancy), pelvismuscles, bones and joints Disadvantages - requires high level ofskill to accurately interpret the images - image quality can beeasily affected e.g. by air, areas of calcification and body size - sometimes requiresspecial conditions e.g. fasting or full bladder |

