![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
111 Cards in this Set
- Front
- Back
|
What are 3 top causes of amenorrhea?
|
1. Pregnancy
2. Anovulation 3. The patient lacks an endometrium which can reach the outside world |
|
|
What's the difference between preeclampsia and eclampsia?
|
Preeclampsia is characterized by hypertension and proteinuria in pregnancy. Eclampsia is preeclampsia with seizures.
|
|
|
What is the most common breast tumor in women younger than 35 years old?
|
Fibroadenoma
|
|
|
What embryonic structure(s) give rise to the epithelial lining of the uterus and fallopian tubes?
|
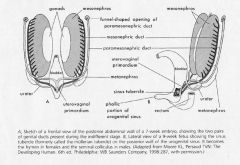
The epithelial lining of the uterus and tubes is derived from the paramesonephric duct. The surrounding mesenchyme gives rise to the myometrium and CT of the uterus. There’s a fusion of the caudal end of the paramesonephric duct that becomes the uterus, and the distal ends of the paramesonephric duct become the fallopian tubes.
|
|
|
A 15 y/o woman finds that she bleeds around her tampon. What disorder/abnormality does this bring to mind?
|

Longitudinal septum
(or Uterus didelphys) |
|
|
Mutations in what gene can cause Hand-Foot-Genital syndrome, an autosomal dominant condition characterized by skeletal malformations (shortened metacarpal, metatarsal, and phalangeal bones) and incomplete mullerian fusion?
|
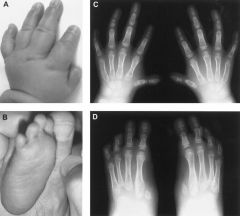
HOXA13 gene
|
|
|
What is Rokitansky syndrome?
|
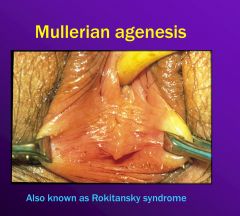
Rokitansky syndrome, or mullerian agenesis, is an absence of the uterus, cervix, and upper vagina. It’s the second most common cause of primary amenorrhea after gonadal failure. The women are not capable of carrying their own offspring, but they could have oocytes extracted and a surrogate mother.
|
|
|
What are the top 3 clinical features of Turner syndrome, in terms of frequency?
|
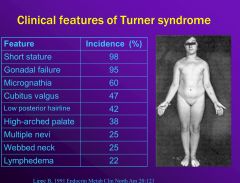
• Short stature
• Gonadal failure • Micrognathia |
|
|
How could diethylstilbestrol (DES) affect the uterus?
|

DES could cause a T-shaped uterus incapable of carrying a fetus to full term
|
|
|
What would you prescribe for a polycystic ovarian syndrome patient with severe hirsutism?
|
Spironolactone, a potassium-sparing diuretic with anti-androgenic properties may be prescribed.
|
|
|
What is the definition of dysfunctional uterine bleeding (DUB)?
|
Dysfunctional uterine bleeding is a woman who is anovulatory and has menometrorrhagia (abnormally frequent, heavy bleeding).
|
|
|
How do levels of AMH relate to a polycystic ovarian syndrome (PCOS)?
|
High levels of AMH (produced by granulosa cells) are indicative of PCOS.
|
|
|
What would the LH/FSH ratio be (high, low, normal) in a patient with polycystic ovarian syndrome (PCOS)?
|
LH/FSH ratio would be high in a woman with PCOS.
|
|
|
Why would you prescribe oral contraceptives for a woman with polycystic ovarian syndrome (PCOS)?
|
Oral contraceptives can help with cosmetic issues (acne, hirsutism), and it can also help protect the endometrium. An added benefit is that OCs cut the lifetime risk for ovarian cancer in half.
|
|
|
What would you prescribe to a hypothalamic amenorrheic patient to help prevent bone loss?
|
Combination oral contraceptives
|
|
|
What is the most common cause of menorrhagia?
|

Leiomyomata (fibroids)
|
|
|
What are the roles of Oct4 and Cdx2 in fetal development?
|
Oct4 is critical for maintaining the undifferentiated state of embryonic stem cells in cell culture (i.e., maintaining pluripotency), so it’s maintained at a high level in inner cell mass. When it decreases, Cdx2 gets increased, which allows outside cells to take on trophectoderm phenotype.
|
|
|
What are 3 risk factors for improper decidualization (which can result in abnormal placental implantation/invasion into the uterine wall)?
|
1. Placenta previa (the covering of the cervical os by the placenta)
2. Prior C section 3. Prior endometrial curettage (the removal of tissue from the uterus by a scoop-shaped surgical instrument) |
|
|
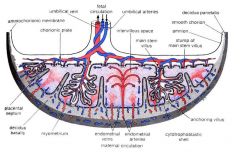
What’s the difference between placental accreta, increta and percreta?
|
1. Accreta – superficial implantation of chorionic tissue onto myometrium with no intervening decidua
2. Increta – deep implantation of placental tissue into myometrium with no intervening decidua 3. Percreta – penetration of placental tissue through the uterine wall serosa |
|
|
What is the most common site of ectopic implantation?
|
The fallopian tube (98% of ectopic pregnancies)
|
|
|
What are the classical clinical symptoms associated with an ectopic pregnancy?
|
1. Amenorrhea
2. Abdominal or pelvic pain 3. Vaginal bleeding |
|
|
What is misoprostol, and what is its use in relation to pregnancy?
|
Misoprostol is a prostaglandin, and it’s used 48 hours after mifepristone (an anti-progestin) to increase the success rate of abortion.
|
|
|
What is the most important risk factor for spontaneous abortion? What are other important risk factors?
|
• Age is the most important risk factor. Other risk factors:
• heavy smoking • increased caffeine ingestion • cocaine use • NSAIDs peri-implantation |
|
|
What is an anembryonic abortion?
|
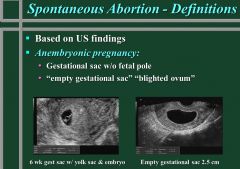
An anembryonic abortion is an abortion where the gestational sac is present but no fetal pole can be identified on ultrasound exam.
|
|
|
What is a missed abortion?
|
A missed abortion is when the pregnancy is nonviable but retained in the uterus for an extended period of time. Women may have light uterine bleeding but are otherwise asymptomatic and have not begun to actively miscarry the pregnancy.
|
|
|
What is a complete abortion? Incomplete abortion?
|
A complete abortion is total passage or evacuation of all products of conception, whereas an incomplete abortion is partial retention of products of conception.
|
|
|
What is recurrent abortion?
|
Recurrent abortion is defined as 3 or more abortions without a live birth.
|
|
|
What is the mechanism behind the use of mifepristone two days before a prostaglandin to enact abortion?
|
Mifepristone is an anti-progestinthat changes the way the myometrium contracts and enhances the production of gap junctions, so that instead of acting as individual fibrils, there’s chemical communication between the myofibrils of the myometrium that’s coded for by the estrogen receptor and normally blocked in the presence of progesterone. By giving an anti-progestin, you block the inhibition of the gap junctions. Then you have a myometrium that’s more receptive to prostaglandins. Thus you have a myometrium that can better contract as a syncytium to expel the conception material.
|
|
|
Which clotting factors do NOT increase during pregnancy?
|
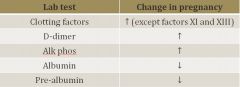
Factors 11 and 13
|
|
|
What is the “Chadwick sign?”
|
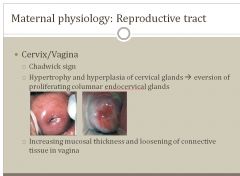
Hypertrophy and hyperplasia of cervical glands leading to eversion of proliferating columnar endocervical glands.
|
|
|
What is the maximal additional caloric intake for someone who’s pregnant?
|
300 kcal/day if activity level is the same
|
|
|
When do fetal breathing movements begin?
|
Fetal breathing movements begin at 16-22 weeks and are an important indicator that the fetus is well-oxygenated.
|
|
|
What is the definition of a preterm birth?
|
• A preterm birth is birth prior to 37 weeks of gestation.
• Incidence is 12%, and accounts for 85% of perinatal morbidity and mortality. |
|
|
What is the definition of PROM (premature rupture of membranes), and what is PPROM?
|
PROM is rupture of membranes prior to the onset of labor. PPROM (preterm premature rupture of membranes) is rupture of membranes prior to the onset of labor and before 37 weeks gestation.
|
|
|
What is the definition of placental abruption?
|
Placental abruption is premature separation of the placenta from the uterine wall and most typically characterized by vaginal bleeding in the presence of uterine contractions.
Risk factors: • Hypertension • Prior placental abruption • Abdominal trauma • Smoking • Cocaine • Submucosal fibroids • PPROM |
|
|
What drugs can be administered to help with preterm labor?
|
Antenatal corticosteroids can be administered, usually within 2 days. Beta-methaxone and dexamethaxone can cross the placental barrier and help improve lung maturity by binding to glucocorticoid receptors and upregulating various genes.
|
|
|
What are 2 of the most important contraindications to tocolytics?
|
Tocolytics can delay delivery an average of 48 hours and are usually given for only 48 hours. 2 major contraindications to tocolytics:
Intraamniotic infection (you have to deliver or the mom will get really sick) Significant maternal bleeding. |
|
|
What is placental previa?
|
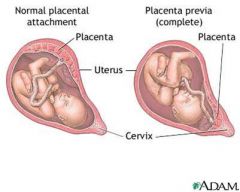
Placental previa is when the placenta covers the cervical os.
It's characteirzed by painless bright red vaginal bleeding. Accounts for 20% of 3rd trimester bleeding. |
|
|
Dr. Su gave only one example where bleeding during pregnancy would be fetal blood. In what context was this bleeding?
|
Vasa previa, an obstetric complication defined as "fetal vessels crossing or running in close proximity to the inner cervical os." These vessels course within the membranes (unsupported by the umbilical cord or placental tissue) and are at risk of rupture when the supporting membranes rupture.
|
|
|
What is the treatment for preeclampsia?
|
Delivery
|
|
|
If a woman has twins, and the placenta is monochorionic, what is the likelihood that the twins are dizygotic?
|
Monochorionic twins are nearly always monozygotic, whereas dichorionic twins could be either monozygotic or dizygotic.
|
|
Fibrinoid necrosis with acute atherosis is characteristic of what pathologic phenomenon ?
|
Preeclampsia
|
|
|
What is the main cause of pathology in fetal vasculature?
|
Obstruction:
• Thrombosis in fetal vessels • Avascular villi • Fetal thrombotic vasculopathy |
|
|
What type of vessel connections lead to significant net movement of blood from one twin to another in the context of a twin birth?
|
Artery-vein connections can lead to twin-twin transfusions.
|
|
|
Where does Beta-HCG come from (which cell type), and what is its function in pregnancy?
|
Beta-HCG comes from the Syncytiotrophoblasts, and its function is to maintain the corpus luteum of pregnancy by acting as an LH analogue.
|
|
|
Why is estrogen added to hormonal contraceptive pills?
|
• Estrogen has the effect of suppressing pituitary FSH.
• The more estrogen, the better endometrial control and the less spotting. • Estrogen was added, because it stabilizes the endometrium and makes the pill better tolerated. |
|
|
What are the 3 major mechanisms by which progestin provides contraception?
|
Progestin prevents ovulation by slowing the frequency of GnRH pulses and suppressing the LH surge. Progestin additionally:
• Induces endometrial atrophy, which impairs implantation • Thickens the cervical mucus, impeding sperm migration • Decreases tubal ciliary motility, which alters ovum and blastocyst transport |
|
|
What are important side effects of progestin?
|
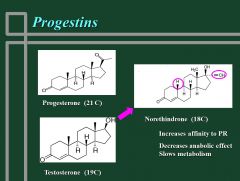
Progestin side effects are related to its homology with testosterone and activation of androgen receptors, whereby you get androgenic features, like:
• Acne • Oily skin • Lipid changes |
|
|
What’s the difference in terms of ovulation when giving progestin only versus progestin+estrogen combination oral contraceptive?
|
Suppression of ovulation isn’t as good for progestin given alone as compared to progestin is given with estrogen
|
|
|
Which of the following is not associated with oral contraceptive use:
A) Decreased risk for ovarian and endometrial cancer B) Decreased dysmenorrhea C) Decreased pelvic inflammatory disease D) Decreased bone density |
Answer: D) Decreased bone density; actually, increased bone density is associated with oral contraceptive use
|
|
|
What is the mechanism of the Plan B pill?
|
Delays ovulation and may also impede tubal transport and impede implantation due to endometrial changes.
|
|
|
What are the key parameters in the semen analysis of the male in an infertile couple?
|
Concentration (>15M/cc)
Motility (>40%) Morphology (>4% that are like absolutely perfect) |
|
|
Why is AMH used to assess ovarian reserve?
|
AMH is manufactured by granulosa cells, so AMH can be an indication of how many granulosa cells you have. Every primordial follicle has a certain number of granulosa cells, so you can therefore use AMH to determine how many eggs you have
|
|
|
Besides AMH, what biometrics are used to assess ovarian reserve?
|
Antral follicle count (AFC)
|
|
|
How does hyperprolactinemia cause anovulation?
|
• Elevated prolactin inhibits gonadotropin and estrogen secretion (accounts for 5-10% of women with anovulation).
• Could be caused by drugs (anti-psychotics), pituitary adenoma, hypothyroidism • Symptoms: galactorrhea, amenorrhea, oligomenorrhea, infertility |
|
|
How does obesity cause an increase in estrogen?
|
Adipose tissues synthesize androstenedione, which gets converted to estrone, increasing estrogen levels.
|
|
|
Which of the following is NOT associated with early menopause?
A) Cigarette smoking B) High altitudes C) Oral contraceptives D) Metabolic disorders |
Answer: C) Oral contraceptives. Age of menopause is NOT influenced by age of menarche, number of ovulations or pregnancies, lactation, or the use of OCP. Race, socioeconomic status, education, and height also have no effect on age of menopause.
|
|
|
Which of the following is NOT a long-term effect of menopause?
A) Cardiovascular disease B) Osteoporosis C) Genital atrophy/vaginal dryness D) Decreased risk of colon cancer E) New onset depression F) Introital narrowing |
Answer: D) Decreased risk of colon cancer
|
|
|
What is the median age of the onset of menopause?
|
51.5 years old
|
|
|
What is the definition of menopause?
|
Menopause is the permanent cessation of the menstrual period determined retrospectively after a woman has experienced 12 months of amenorrhea without any other obvious pathological or physiological cause.
|
|
|
How do the levels of inhibin B, serum FSH, and luteal phase progesterone levels change during the late productive years?
|
• Serum inhibin B and luteal phase progesterone levels decrease.
• Serum FSH increases slightly. |
|
|
According to the Women’s Health Initiative study, how does a combined estrogen-progestin medical regimen affect one’s risk for: CHD, stroke, breast cancer, colorectal cancer, hip fracture versus placebo?
|
• 29% increased risk for CHD
• 41% increased risk for stroke • 26% increased risk for breast cancer • 37% decreased risk for colorectal cancer • 34% decreased risk for hip fracture |
|
|
What’s the definition of premature ovarian insufficiency?
|
Premature ovarian insufficiency (POI) is menopause prior to the age of 40. It affects 1% of the population, and can be causesd by Turner syndrome, autoimmune disorders, smoking, chemotherapy, or can be due to unknown causes in many cases. Hot flashes/flushes are not common in this group of patients.
|
|
|
Which of the following does NOT increase your risk for fibroids?
A) Increased # of births B) Older age C) Obesity D) Hypertension E) Excessive beer drinking |
Answer: A) Parity/Increased # of births actually decreases your risk for fibroids. Smoking also decreases your risk for fibroids.
|
|
|
What are risk factors for endometrial cancer?
|
• Lynch syndrome
• Obesity • Unopposed estrogen (the same risk factors as for hyperplasia) |
|
|
What is the most common gynecological cancer?
|
Endometrial carcinoma
|
|
|
Can leiomyomas degenerate into leiomyosarcomas?
|
No; they are distinct entities. Leiomyomas do NOT transform into leiomyosarcomas.
|
|
|
Which pathogens commonly cause urethritis? (in males)
|
• Neisseria gonorrhoeae
• Chlamydia trachomatis • Herpes simplex viruses (HSV) |
|
|
Which STDs cause pelvic inflammatory disease (PID)?
|
STDs that cause PID:
• N. gonorrhoeae • C. trachomatis • Vaginal flora (including anaerobes) |
|
|
What would you typically use to treat gonorrhea?
|
Penicillin has historically been the treatment of choice.
Ceftriaxone (a single IM shot) is appropriate. Anti-chlamydial treatment should also be given due to the high frequency of co-infection with these two bacteria. |
|
|
The Venereal Disease Research Laboratory (VDRL) test is useful for a presumptive diagnosis of syphilis but not a final diagnosis. Why not, and what would you use to confirm a diagnosis of syphilis?
|
The VDRL and nontreponemal serologic assays such as rapid plasma reagin (RPR) are not specific, so you would go to a treponemal serologic test like the Fluorescent treponemal antibody absorption (FTA-ABS) test or the T. pallidum passive particle agglutination (TP-PA) assay.
|
|
|
What would you typically use to treat chlamydia?
|
Azithromycin or doxycycline are recommended, but erythromycin, ofloxacin, and levofloxacin are also active.
|
|
|
In which stage of syphilis do patients typically contract generalized rash (especially on soles and palms) and enlarged lymph nodes?
|

Secondary syphilis
|
|
|
What is the drug of choice for syphilis?
|
Penicillin G
|
|
|
What pathogen can cause the production of a malodorous yellow-green vaginal discharge, vulvar itching, dysuria, urinary frequency and dyspareunia in women? How would you treat the patient?
|
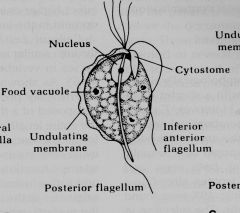
Trichomonas vaginalis; you can treat with metronidazole (Flagyl).
|
|

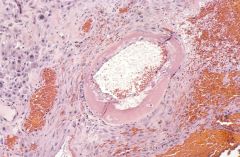
What pathogen is shown in this picture?
|
Clue cells, indicative of bacterial vaginosis
|
|
|
A 32 y/o female w/ h/o amenorrhea develops white nipple discharge. She eats a balanced diet and exercises regularly. She is not sexually active. Her family history is significant for her mom dying of breast cancer at 50. The most likely diagnosis in this patient is:A) Fibrocystic breast disease B) Fibro adenoma C) Intraductal papilloma D) Lobular breast carcinoma E) Pituitary adenoma
|
The correct response is E) Pituitary adenoma. A prolactin-secreting pituitary adenoma (prolactinoma) would explain the findings in this patient. Hyperprolactinemia causes galactorrhea and amenorrhea in females. Galactorrhea results from the direct stimulatory effect of prolactin on the mammary glands, and amenorrhea results from the inhibitory effect of prolactin on GnRH secretion.
|
|
|
How does clomiphene work to induce ovulation?
|
Clomiphene is an estrogen receptor modulator that decreases negative feedback inhibition on the hypothalamus by circulating estrogen and thereby increases gonadotropin production (e.g., FSH and LH) to induce ovulation.
|
|
|
A 73-year-old female presents with lower abdominal discomfort. Physical exam reveals an adenexal mass on the right side. What's the most likely cause of the patient's symptoms?
|
Ovarian malignancy is the most likely explanation for an adnexal mass in an elderly female.
|
|
|
What is the HELLP syndrome?
|
Hemolytic anemia, Elevated Liver enzymes, and Low Platelets
|
|
|
What would a granulosa-theca cell tumor most likely secrete? A) HCG B) AFP C) CA-125 D) Estrogen E) Androgen
|
D) Estrogen; granulosa cell tumors are sex-cord stromal tumors that secrete estrogen
|
|
|
What is the most common cause of postmenopausal bleeding?
|
The most common cause of postmenopausal bleeding is atrophy, but you should still do a biopsy to rule out endometrial cancer, which occurs 5-10% of the time due to unopposed estrogen.
|
|
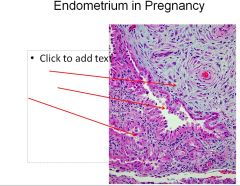
What is the name for the “reaction” that mimics carcinoma in the endometrium during pregnancy (3rd arrow)?
|
Arias-Stella reaction.
|
|
|
What’s the difference between type I and type II ovarian carcinomas?
|
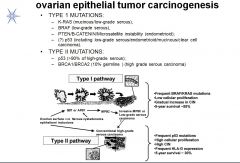
• Type I are associated with BRAF/KRAS mutations, whereas type II are associated with p53 mutations
• Type I has low cellular proliferation, whereas type II has high cellular proliferation • Type II has a worse prognosis |
|
|
What is the impact of serotonin on desire and arousal?
|
Both serotonin and prolactin actually inhibit both desire and arousal, whereas dopamine, NE, testosterone, estrogen are excitatory.
|
|
|
What illness is a common source of sexual dysfunction in women?
|
Diabetes
(arteriosclerosis for men can cause ED) |
|
|
What are current pharmacologic treatment options for Hypoactive Sexual Desire Disorder (HSDD)?
|
• Hormonal
o Estrogen o Testosterone • PDE inhibitors o Sildenafil |
|
|
In what group of women do you commonly see the phylloides tumor?
|
The phylloides tumor is usually seen in postmenopausal women. It arises from the stroma of the breast lobules. Phylloides tumor needs to be excised whereas the fibroadenoma does not need to be excised.
|
|
|
Which breast tumor can metastasize to the meninges?
|
Invasive lobular carcinoma
|
|
|
In what location of the breast do 50% of breast carcinomas arise?
|
The upper outer quadrant
|
|
|
Lobular carcinoma in situ (LCIS) almost always expresses which cancer biomarker(s)?
|
ER/PR
|
|
|
Even if you have negative axillary lymph node metastases, what’s your 10 year disease free survival rate?
|
70-80%
|
|
|
What antibodies are in a mother’s milk?
|
IgA
|
|
|
What is the most common breast malignancy?
|
Infiltrating ductal carcinoma is the most common breast malignancy (80%), originating from ductal epithelium and infiltrating supporting stroma and possibly beyond.
|
|
|
What factor determines whether or not the gonads develop into testis or ovaries?
|
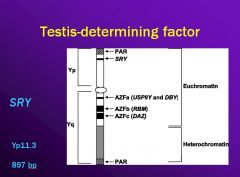
The testis determining factor (SRY)
|
|
|
What causes the mesonephric ducts to regress?
|
Mesonephric ducts regress due to lack of androgens.
|
|
|
What induces menarche, the first menses?
|
During puberty, the suppression of the hypothalamic-pituitary axis is reduced by decreased sensitivity to the inhibitory effects of estrogen on the axis. Pulsatile release of GnRH at night causes enough estrogen secretion form the ovary that the endometrium proliferates and then sheds.
|
|
|
What is adenomyosis? What is endometriosis?
|
Adenomyosis = glands and stroma in myometrium
Endometriosis = functioning glands and storma outside the uterus |
|
|
What are the 2 most common causes of dysmenorrhea?
|
1. primary dysmenorrhea - prostaglandin mediated
2. endometriosis Initial response to NSAIDs will often make an early distinction (prompt response to NSAIDs indicates primary dysmenorrhea). A definitive diagnosis of endometriosis often requires laparascopy. |
|
|
What are the endocrine features of polycystic ovarian syndrome (i.e., what lab tests would you expect for PCOS (e.g., AMH, LH/FSH, etc.))?
|
* Elevated AMH
* Elevated LH/FSH ratio * Normal serum levels of TSH, prolactin, and 17-OH-Progesterone * High normal testosterone levels * High normal DHEA-S (of adrenal origin) levels |
|
|
Besides chromosomal abnormalities, what are some reasons that so many pregnancies fail?
|
* Exposure to teratogens - diabetes mellitus with poor glycemic control, drugs - (isotretinoin), maternal fever, environmental chemicals - (mercury)
* Uterine abnormalities – uterine septum, submucous fibroid, intrauterine adhesions – can interfere with implantation & growth * Maternal infection - eg, Listeria monocytogenes, Toxoplasma gondii, parvovirus B19, rubella, herpes simplex, cytomegalovirus, lymphocytic choriomeningitis virus * Inherited thrombophilias (Factor V Leiden, etc) * Unexplained |
|
|
What is the most common symptom for ectopic pregnancy?
|
* The most common symptom is bleeding/spotting in first trimester, which is due to sloughing of endometrium.
* Adnexal mass * Acute abdominal pain due to peritoneal irritation from abdominal bleeding. Blood is inflammatory and causes pain; it irritates the diaphragm and can cause referred pain to the shoulder. You can get liters of blood in the abdomen from an ectopic pregnancy. |
|
|
What are treatment options for ectopic pregnancy?
|
* Surgery is primary option
* Medical management would be with methotrexate, which is a folic acid antagonist that inhibits DNA synthesis and cell reproduction by blocking dihydrofolate reductase |
|
|
What are the causes of anovulation?
|
* Hypogonadotorpic hypogonadal anovulation (5-10% of anovulatory women)
-Low or low normal serum FSH and LH, low E2 * Polycystic Ovarian Syndrome (PCOS) -ovarian hyperandrogneism (must exclude other causes of hyperandrogenism) *Premature Ovarian Insufficiency (POI) (hypergonadotropic hypoestrogenic anovulation; 10-30% of cases of anovulaiton) -could be caused by Turners or abnormal karyotype, viral infections, auto-immune etiologies, fragile x pre-mutation -POI is the most common cause of primary amenorrhea * Hyperprolactinemia (5-10% of anovulatory women) -elevated prolactin inhibits gonadotropin and estrogen secretion |
|
|
What sets apart the NIH criteria for polycystic ovarian syndrome from the AES criteria and the Rotterdam criteria?
|
NIH criteria requires menstrual irregularity, and unlike the Rotterdam criteria does not require imaging proof of PCOS.
NIH criteria: 1. menstrual irregularity due to oligo or anovulation 2. evidence of hyperandrogenism 3. exclusion of other causes of hyperandrogenism and menstrual irregularity, such as congenital adrenal hyperplasia, androgen-secreting tumors, and hyperprolactinemia |
|
|
How does oral contraceptive use affect the risk for ovarian cancer?
|
Oral contraceptives decrease ovarian CA risk 36% with ever-use and 8-10% with every year of use. Protection may last for up to 10 years.
|
|
|
What are symptoms for ovarian cancer?
|
1) Bloating
2) Pelvic or abdominal pain 3) Difficulty eating or early satiety 4) Urinary symptoms (urgency or frequency) 5) Fatigue, back pain, dyspareunia, constipation, and menstrual irregularities Symptoms may persist or worsen, indicating ovarian CA. |
|
|
What is the most common benign cause of an elevated CA-125, the tumor marker?
|
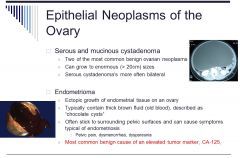
Endometrioma
|
|
|
What are first line chemotherapy agents for epithelial ovarian cancer treatment?
|
* Carboplatin (alkylating agent)
* Paclitaxel (microtubule inhibitor) |
|
|
Which histologic types of cancer are associated with BRCA1/BRCA2 mutations?
|
Medullary carcinoma (also tubular carcinoma, but more likely medullary)
|
|
|
Which of the following is more likely to become bilateral disease: infiltrating ductal carcinoma or infiltrating lobular carcinoma?
|
DCIS/infiltarting ductal carcinoma --> unilateral
lobular --> bilateral |

