![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back

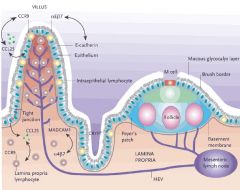
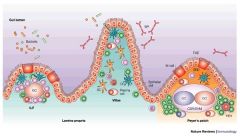
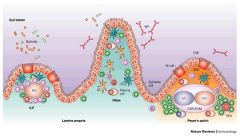
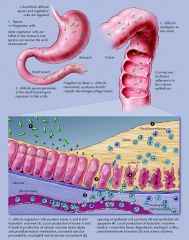
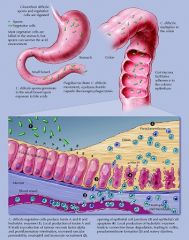
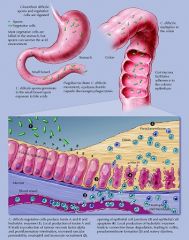
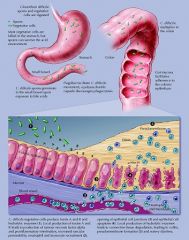
Describe the structure of Peyer's patches
|
Lymphoid FOLLICLES (not a node) covered by specialized epithelium (M cells)
B cells are primed here and leave via lymphatics to lamina propria (and other mucosal sites) where they mature into IgA secreting plasma cells |
|
What is the function of M cells?
|
Specialized epithelial cells that cover Peyer's patches; transport antigens from lumen across epithelium (via M = Microfold apex) into dendritic cell rich area; delivers antigens into underlying lymphoid tissue where T and B cells are primed
|
|
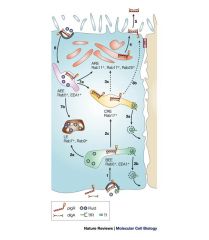
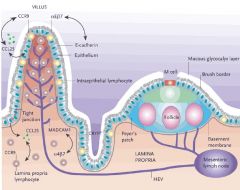
What is the role of CCR9 (chemokine receptor), A4B7 Integrin (adhesion molecule) and MAdCAM-I in lymphocyte homing to the lamina propria?
|
T cells in lamina propria express CCR9 and A4B7 integrin
MAdCAM-1 expressed by blood vessels in lamina propria is a ligand for A4B7 integrin |
|
Compare contrast intraepithelial lymphocytes (IELs) with lamina propria lymphocytes (LPLs)
|
IELs: CD8+ T cells, express CD45R0+, sustain epithelial integrity by rapidly eliminating infected and damaged cells
LPLs: CD4+/CD8+ T cells, NK and plasma cells, express CD45RO +, Many roles CD45RO+ = membrane protein which modulates lymphocyte ativation |
|
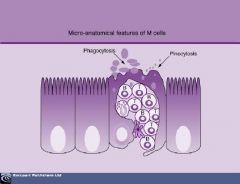
Which cells transport antigens across the epithelium to DCs in Peyer's patches?
|
M cells
|
|
|
Naive B cells in the follicles of lymphoid tissues express what immunoglobulins?
|
IgM and IgD
|
|
|
What class of MHC do DC use to present antigenic peptides to CD4+ B cells
|
MHC II
|
|
Where is IgA dominantly produced?
|
Mucosal sites; i.e. lamina propria
|
|
|
What is the structure and function of IgA?
|
IgA dimer exists but mostly monomeric in serum
Neutralizing antibody (neutralizes microbes/toxins); NOT an opsonizing Ab, does NOT bind/mediate lysis by complement |
|

What is the function of the secretory component of pIgR?
|
Stays attached to IgA after release into the lumen and protects it from proteolysis
|
|

What is the name of IgA with secretory component attached?
|
sIgA/secretory IgA
|
|
Which receptor mediates the transport of dimeric IgA across mucosal membranes?
|
pIgR (polymeric immunoglobulin receptor)
|
|

What is the difference between the inactivated polio vaccine and the oral polio vaccine?
|
IPV: killed polio, injected subcutaneously, LOW LEVELS of viral sIgA
OPV: live, orally, INDUCES sIgA BINDS VIRAL SURFACE ANTIGENS PREVENTS ATTACHMENT TO MUCOSAL CELLS; REMOVED BY PERISTALSIS Prevents virus from entering cells |
|

What is the difference in risk between IPV And OPV?
|
Since OPV is a live (3 attenuates strains) virus can revert to virulence
|
|
What is the rationale for oral administration of rotavirus vacine (or OPV)?
|
Induces productoin of sIgA which neutralizes virus at point of entry/prevents infection
Mimics virus's fecal-oral route of transmission |
|

A patient presents with diarrhea. Labs reveal absent B cells and all serum Igs are low. Disorder?
|
X linked agammaglobulinemia (Bruton's disease); due to a defect in B cell Tyrosine Kinase (BTK)
|
|
|
A patient presents with diarrhea. You note the presence of many B cells that will not mature; all serum Igs are low
|
Common Variable Immunodeficiency Disorder (CVID) can be due to giardia infection
|
|
|
A patient presents with diarrhea. B cells are present; low serum IgA, IgG; HIGH serum IgM
|
Hyper-IgM syndrome due to CD40L deficiency (so B cells can't be activated to produce IgA or G)
Commonly due to enteric infection |
|
|
A patient presents with diarrhea. T cells and NK cells are absent but B cells are present.
|
SCID
|
|
If lymphocytes were isolated from the lamina propria, which lymphocyte types would be highest?
|
T lymphocytes expressing CCR9
|
|
|
What is the difference between food poisoning and food intoxication?
|
Food poisoning = microorganism ingested, replicates in GI tract, symptoms associated with toxins or virulence factors
Food intoxication; toxins in food produced by bacteria but organism not necessarily in food; symptoms APPEAR SOONER than food poisoning |
|
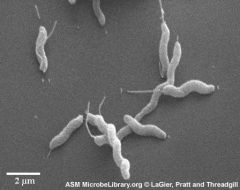
A patient presents with fever, headache, followed by half a day of abdominal cramps and a bloody, loose diarrhea. History is notable for eating chicken (poultry) and drinking unpasteurized milk. Labs show a gram negative, curved motile rod. What is the likely orgainsm?
|
campylobacter jejuni; most common cause of gastroenteritis in the US
|
|
|
A patient presents with bilateral crnial nerve palsias (diplopia) and difficulty swallowing (dysphagia). The patient is also notable for constipation. The patient notes consuming canned vegetables today. What is the likely organism?
|
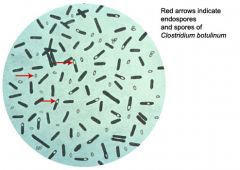
Clostridium botulinum; spores float through air and land on food which is then canned; respiratory paralysis can become severe if not fatal
|
|
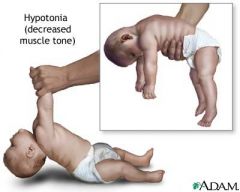
An infant presents with floppy baby syndrome and constipation for the past few days. The mother notes the infant got their hand into a honey jar earlier that week. What is the likely orgainsm?
|
Clostridium botulinum; good prognosis
|
|
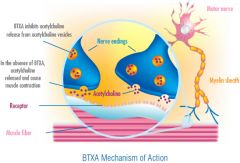
What is the mechanism of action of botulinum toxin?
|
A-B toxin; A subunit inactivates proteins necessary for acetylcholine release; B subunit needed for receptor binding in neurons
Stops acetylcholine from being released |
|
What is the major toxin of C. perfringens regarding food poisoning from contaminated meat?
|
Type A; the enterotoxin disrupts ion transport in the ileum leading to fluid loss
|
|
What is the major toxin of C. perfringens regarding necrotizing enteritis?
|
Type C - the beta toxin is pore forming and causes bloody diarrhea; necrotizing inflammation of the small bowel
|
|
A patient has been on the broad spectrum antibiotic Clindamycin and develops severe bloody diarrhea, abdominal cramping and fever. What is the likely organism?
|
Clostridium difficile
|
|
|
How does antibiotic use lead to diarrhea indirectly?
|
Broad spectrum antibiotics kills off normal flora allowing for oppotunistic pathogens to infect
Candida albicans and clostridium difficile are two examples |
|
What is the mechanism of action of Toxin A for C. difficile?
|
attracts neurotrphils to ileum via cytokine release and causes disruption of cell junctions, resulting in fluid movement into lumen and diarrhea
|
|
What is the mechanism of action of Toxin B for C. difficile?
|
Toxin B causes actin depolymerization and thus cytoskeletal damage it is 1000x more potent than Toxin A
|
|

What are two common complications of listeria monocytogenes infection?
|
Septicemia and meningitis
Not the most common cause of food poisoning but has the highest mortality rate |
|

What are the most common food sources associated with listeria monocytogenes?
|
Soft cheese!
Not the most common cause of food poisoning but has the highest mortality rate |
|
|
What is the major source of Vibrio cholerae infection?
|
Contaminated water; NOT usually spread person to person
|
|
|
What is the primary means of treatment for Vibrio cholerae infection?
|
Fluid and electrolye replacement; doxycycline
|
|
|
What are the two biotypes of vibrio cholerae?
|
O1 serogroup are divided into classical and El Tor
|
|
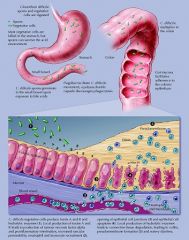
Mechanism of action of cholera toxin?
|
Vibrio cholerae synthesizes cholera toxin -> B subunit binds to epithelial cell which endocytoses A subunit; A subunit ribosylates G protein which constitutively activates adenylate cyclase; increased cAMP activates PKA through phosphorylates CFTR promotes water and Cl loss through channel
|
|
|
What is the mechanism of transmission of S. aureus associated food intoxication?
|
Heat stable enterotoxin; bacteria might be present if food was not heated or cooked
potato salad! |
|
|
What is the heat characteristic of the emetic vs the diarrheal form of bacillus cereus?
|
Emetic: Heat stable
Diarrheal: Heat labile |
|
A 3 month old female infant was brought to the EM with a history of constipation to which her mother had given a tablespoon of honey for treatment. The physical exam revealed dry mucosa, sluggish pupillary response, and significant hypotonia. Gram stain of the fecal sample revealed a gram positive spore forming rod. Diagnosis?
|
C. botulinum
|
|
|
A 67 yo man presents with fever, abdominal cramping and frequent diarrhea for four days. He had been on the broad spectrum antibiotic clindamycin three weeks earlier. Diagnosis?
|
C. difficile
|
|

24 people became ill within 3 hrs after eating a meal at an office party. Al had nausea, vomiting and crampy abdominal pain. The food preparer had served cold ham. Which toxin would likely be identified in the ham?
|
Toxin A via C. perfringens
|

