![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
16 Cards in this Set
- Front
- Back
|
Thyroid anatomy:
|

*By 11-12 weeks, the fetus is making thyroid hormone.
*PT glands on the back. |
|
|
Hypothalamic-Pituitary-Thyroid axis:
|
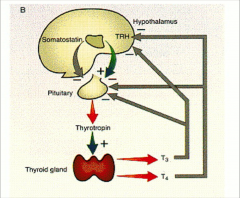
*Somatostatin only has small effect.
*T3 is much more potent in feedback. Thyroid makes much more T3 than T4. |
|
|
Regulation of thyroid hormone synthesis:
-hypothalamus -putuitary -diet |
*Hypothalamus: TRH: tripeptide that binds its receptor on pituitary cells to increase TSH & PROLACTIN.
-stimulated by cold (from uterus to the environment), decreased T3, leptin -inhibited by stress, feedback from T3/T4 *Pituitary: TSH: glycoprotein (shares alpha subunit with LH/FSH; ß subunit specific) that binds its receptor on thyroid follicular cells to signal via GSa (cAMP); increases secretion and synthesis of T4; very sensitive to feedback *Diet: Iodine: Na-I symporter actively transports I- from blood into thyroid cell; excreted by kidneys |
|
discuss
|
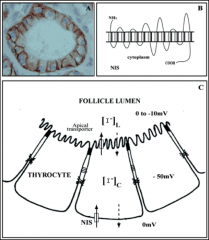
*Follicles consist of lumen containing TG and follicular cells (thyrocytes)
*Synthesis requires NIS, TG and TPO *Large amounts of I- suppress synthesis and function of NIS for a short time (“escape”) *Internal symporter is called pendrin. *Thyroid peroxidase (TPO) catalyzes iodination and coupling; inhibited by thiocarbamide drugs |
|
|
Synthesis and Secretion of Thyroid Hormones: 3 steps--
|

*Easier to combine 2 DITs, thus more T4 is secreted than T3.
*It later gets converted to T3. |
|
|
Synthesis of T4/T3:
|
*Follicular cells arranged in follicles with center lumen containing colloid (TG)
*TG contains the tyrosines which will be iodinated to become thyroid hormone *Requires Iodine from the diet (step 1: I transport) *Iodine oxidized by thyroid peroxidase (TPO) *Organification and coupling catalyzed by TPO *Endocytosis of iodinated TG (containing T4 and T3) and proteolysis lead to T4/T3 release *TSH stimulates all 3 steps; increases cell size, # |
|
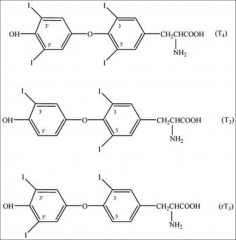
Why is T4 really a prohormone?
|
*T4:
~93% of thyroid's secreted product 80% is deiodinated (35% T3, 45% rT3) in tissues ½ life: 7 days *T3: ~7% secreted product ~90% converted from T4 Binds receptor 10X better than T4 !!! ½ life: 1 day Reverse T3= Inactive T3 |
|
|
Thyroid Binding Globulin:
|
*Liver-derived glycoprotein: binds 70% T4/T3
*Single binding site for T4 or T3 (prefers to bind T4) *X-linked; deficiency more common in males *Congenital deficiency 1:5000 births *Drugs can increase or decrease its synthesis *Estrogen decreases & androgens increase its clearance (thus OCs can increase TOTAL--not free--T4) *Free T4 levels normal, so TSH is normal!!! *30% binding: Transthyretin (aka prealbumin) binds T4>T3 and albumin binds with low affinity |
|
|
Metabolism of Thyroid Hormones:
|
*3 Deiodinase enzymes:
1) Type 1 5’-deiodinase: most abundant form, found in LIVER, KIDNEY and THYROID; outer ring activity provides T3 to the circulation; some inner ring activity produces rT3 and T2 2) Type 2 5’ deiodinase: BRAIN and PITUITARY; maintains intracellular T3 levels for feedback 3) Type 3 5’deiodinase: PLACENTA, infantile hemangiomas; only inner ring activity and thus inactivates T4 to rT3 |
|
|
Deiodinase metabolism of T4/T3 graphic:
|
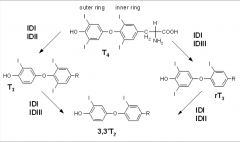
ID: iodo-deiodinase type I, II or III: IDI, IDII, IDIII
*Difference is outer ring vs. inner ring action. |
|
|
How do Thyroid Hormone receptors alpha and ß regulate gene transcription?
|

*Receptor sits on TRE (thyroid response element)
|
|
|
Thyroid hormone receptor mechanisms of action:
|
*2 TR genes: TRalpha (brain) and TRß (liver, tissues)
*TRs function as heterodimers and bind TRE upstream of transcription start sites on DNA *T3 binding to TR displaces corepressor complexes, promoting transcription *Non-genomic actions mediated by T4/T3: interactions with enzymes, membrane proteins, etc |
|
|
Discuss Specific Thyroid Hormone Transporters:
|

Monocarboxylate transporter (MCT) family:
MCT8 and MCT10 are T4/T3 specific *THR=repressor* |
|
|
Thyroid Hormone Functions: impacts on growth and development--
|
*Fetus: neural development; thyroid by ~11 weeks
*Birth: TSH surge due to temp ∆ *Post-natal: critical for CNS development and somatic growth *Pregnancy: increased thyroid hormone 1st trimester |
|
|
Thyroid Hormone Functions: impacts on metabolism--
|
*regulates basal metabolic rate, appetite
*stimulates carbohydrate/fat metabolism *increases protein synthesis and degradation *positive inotropic/chronotropic effects on heart *increases ß receptor expression on heart *Rarely, a cause of obesity |
|
|
Thyroid Disease--briefly touch on hypothyroidism, hyperthyroidism, and thyroid cancers:
|
Hypothyroidism: Primary
-Congenital: dysplasia, dyshormonogenesis -acquired: iodine deficiency, autoimmune *Hyperthyroidism -Autoimmune: Graves disease -Adenoma: e.g., Gsalpha mutations *Cancer: 1% of all malignancies (Boney: "fairly common") -Irradiation (e.g., s/p Chernobyl 1986) -spontaneous mutations in ret |

