![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
The Thyroid: Functional vs Anatomic Abnormalities--
|
*Functional abnormalities
-Hyperfunction -Hypofunction *Anatomic abnormalities -Goiter -Nodules (single or multiple, benign or malignant) *Thyroid disease often presents with both types of abnormalities – sometimes the abnormalities are related, sometimes not |
|
|
daaaaaaaaaaaaamnnnnn!
|
|
|
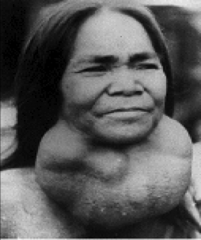
Goiter:
|
*Enlargement of the thyroid gland.
*Goiters occur for a variety of reasons and can be associated with normal thyroid function, hypothyroidism, or hyperthyroidism *Goiter is not generally associated with cancer in the absence of nodules |
|
|
Thyroid Nodule:
|
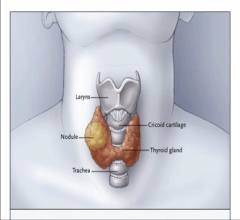
A thyroid nodule is a localized portion of the gland that has a different contour or consistency than the normal gland -- or on imaging, has a different “texture.”
|
|
|
Symptoms of Thyroid Nodules:
|
*Physical examination and symptoms will depend on size and location
*Small nodules- usually asymptomatic *Large nodules: -Often asymptomatic -Cosmetic concern -Hoarseness - Laryngeal n. compression -Stridor, cough, dysphagia, pressure sensation -Substernal or posterior extension (?Pemberton Sign) -Tracheal deviation or compression |
|

|
*Palpable and Visible Thyroid Nodule
|
|

|
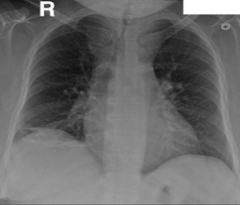
Thyroid Nodule Displacing Trachea
|
|
|
Goiter Causing Tracheal Compression
|
|
|
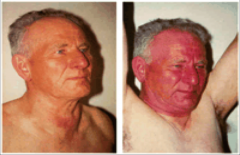
Pemberton Sign
|
|
|
Discuss the Prevalence of Thyroid Nodules:
|
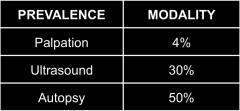
95% nodules are benign
|
|
|
Pathologic Classification of Thyroid Nodules:
|
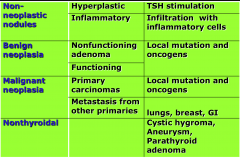
|
|
|
Benign Adenoma: Etiology--
|
*Environmental factors: iodine intake, natural goitrogens, tobacco
*Genetic mutations -Na-I Symporter: hypofunctional -TSH receptor: hyperfunctional *Age, gender, other |
|
|
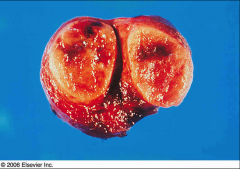
Thyroid adenoma: Pathological Characteristics--
|
*Discrete capsule
*Orderly architecture *Few mitoses *No lymphatic or arterial invasion |
|
|
Thyroid adenoma
*Discrete capsule *Orderly architecture *Few mitoses *No lymphatic or arterial invasion |
|
|
Benign Thyroid Nodule: Treatment Options--
|
*No treatment; continued monitoring
*Surgery *131I Radioiodine--Mainly for toxic nodules *Percutaneous ethanol injection--For cystic nodules *Radiofrequency ablation (RFA) and laser treatment-- (Experimental procedures) |
|
|
Thyroid Nodule: Diagnostic Testing:
|
*TSH
*Imaging: -Neck sonogram -Neck CT or MRI -Radioisotope scan *FNA |
|
|
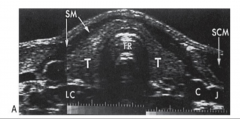
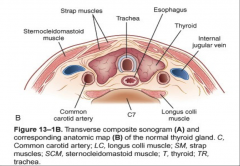
Thyroid Ultrasound:
|
*Sends and receives sound waves
*Image is created based on the density of the examined tissue *Thyroid and adjacent neck anatomy is visualized in detail |
|
|
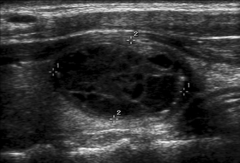
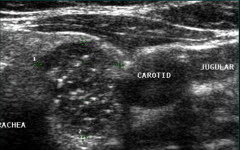
thyroid ultrasound
|
|
|
Thyroid nodule ultrasound Complex nodule
|
|
|
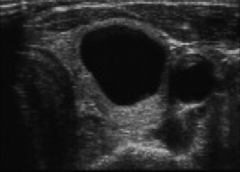
Thyroid nodule ultrasound Simple cyst
|
|
|
Thyroid Ultrasound: Features Associated with Increased Cancer Risk--
|
*Microcalcifications
*Hypoechoic, solid lesion *Infiltrative margins *Increased vascularity *Nodules < 10 mm diameter are not generally biopsied unless patient has a high-risk history for thyroid cancer |
|
|
ultrasound--Thyroid cancer-microcalcifications
|
|
|
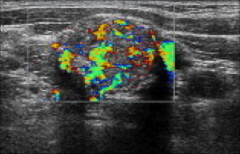
ultrasound--Thyroid cancer-chaotic vascularity
|
|
|
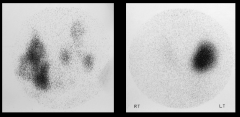
*Radioisotope Scan
L: Multiple cold nodules R: Hot nodule!!!!! *A scan is generally performed only in those patients with low TSH in order to identify toxic nodules, which don’t warrant FNA |
|
|
Thyroid Nodule: Role of CT/ MRI:
|
*To better characterize the relationship of thyroid gland to surrounding structures:
-Tracheal deviation or compression -Mediastinal extension -Deep neck or mediastinal lymph nodes |
|
|
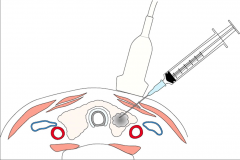
Thyroid FNA
|
|
|
Thyroid Nodule: Evaluation Algorithm:
|
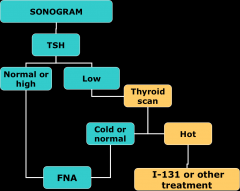
|
|
|
Recommendations for interpreting FNA results:
|
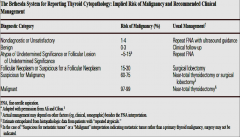
|
|
|
Thyroid Cancer: Molecular Biology--
|
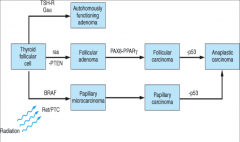
|
|
|
How are thyroid cancer rates in the US changing?
|
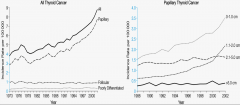
|
|
|
Thyroid Cancer- prevalence and general info:
|
*Prevalence: 5-10% of all thyroid nodules
*Possible 5% prevalence in general population when counting clinically insignificant micro-cancers *Well-differentiated thyroid cancer is one of the most curable malignancies |
|
|
How is survival from thyroid CA?
|
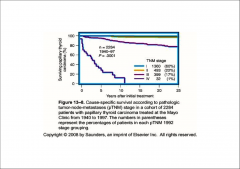
|
|
|
Clinical Features Indicating Higher Risk for Nodule Malignancy:
|
*Age-- <20 and >70
*Gender--Male *Fam Hx--Thyroid cancer, MEN2, Cowden Syndrome, Gardner Syndrome *H/O head or neck irradiation during childhood or adolescence *Prior h/o thyroid cancer *Abnormal lymph nodes *High calcitonin level |
|
|
Discuss the role of Ionizing Radiation in thyroid CA:
|
*Exposure before age 21 increases the risk of papillary thyroid cancer
*Risk increases with lower age and increasing radiation dose, 10cGy to 1500cGy *Risk of cancer can be increased >50x |
|
|
Thyroid Cancer: Classification--
|
*Epithelial
-Follicular cell: Papillary carcinoma, Follicular carcinoma, Hurtle cell carcinoma -Undifferentiated: Anaplastic -C-cell: Medullary *Nonepithelial Secondary tumors, lymphoma, sarcoma |
|
|
Papillary Thyroid Cancer:
|
*90% of all thyroid cancers
-Follicular cells arranged in papillary projections -Large pale irregular nuclei -40% contain Psammoma bodies *Multifocal in ~40% *Excellent prognosis for ~90% of patients *Tends to metastasize locally (~20%) *Distant metastases in <5% |
|
|
Follicular Thyroid Cancer:
|
*Cytological features:
-Cuboidal cells with large nuclei -Usually unifocal -Cells similar to follicular adenoma -Diagnosis based on invasion of blood vessels and/or tumor capsule *More aggressive then papillary thyroid cancer *Spreads hematogenously to lungs & bones *Local lymph node metastases are rare |
|
|
Medullary Thyroid Cancer:
|
*Arises from parafollicular C cells
-Calcitonin, Carcinoembryonic antigen *Sheets of cells separated by pink staining ‘amyloid like’ substance *More aggressive then papillary and follicular thyroid cancer *Metastases to both nodes and distant organs *RET proto-oncogene mutation |
|
|
Less common Cancers Involving the Thyroid:
|
*Anaplastic cancer
-Very aggressive with poor prognosis -Typically older patients with long-standing goiter or differentiated thyroid cancer -Invasive neck involvement and distant metastases are common *Lymphoma -30-80% have Hashimoto thyroiditis -Rapid enlargement of gland or nodules is typical, often causing neck symptoms *Secondary cancers -Melanoma, breast, lungs, colon, lymphoma |
|
|
Mortality rates for thyroid carcinoma:
|
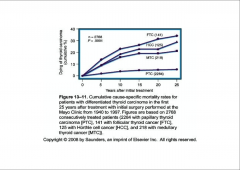
|
|
|
Treatment of Follicular and Papillary Thyroid Cancer:
|
*Surgery
-Near-total thyroidectomy -Partial thyroidectomy *Lymph node dissection *Radioiodine ablation/treatment *Levothyroxine (Low TSH target) *External beam radiation *Tyrosine kinase inhibitors *Chemotherapy: no benefit |
|
|
Radioactive Iodine Treatment:
|
*Adjunctive therapy for higher stage tumors
*Requires high TSH level and low dietary iodine intake to achieve therapeutic dose in cancer cells -Hypothyroidism (stop L-T4 or L-T3), or Recombinant TSH |
|
|
Other Thyroid Cancers: Treatment--
|
*Medullary
-Surgery for localized disease -External beam radiation *Anaplastic -No effective treatment -Debulking surgery for local disease *Lymphoma: Chemotherapy |

