![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
114 Cards in this Set
- Front
- Back
|
Anterior Thoracic Landmarks |
Suprasternal notch - hollowed, u-shaped depressions Sternum - "breastbones" |
|
|
Sternum Landmarks |
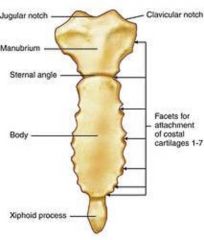
manubrium, body of sternum, xiphoid process, manubriosternal angle |
|
|
Manubrio sternal angle |
Angle found at the conjunction of the manubrium and body of sternum - this is where you start to count from the second rib! |
|
|
Costal Angle |
At the edge of the xiphoid process, angle where the left and right costal margins meet |
|
|
Posterior Thoracic Landmarks |
Vertebra Prominens - Occurs at the base of the neck, C7 Spinous Processes Scapula - inferior border usually at 7th or 8th rib |
|
|
References Lines |
Midsternal Midclavicular Axillary lines |
|
|
Thoracic Cavity |
Mediastinum - contains esophagus, trachea, heart, and great vessels Pleural - contains lungs Lung lobes - anterior, posterior, and lateral |
|
|
Four functions of the Respiratory System |
1. Suppy O2 to the body 2. Remove CO2 as a waste product 3. Maintain homeostasis (acid base balance) 4. Maintain heat exchange |
|
|
What kinds of cultural variations are there with respiratory? |
Asians have a higher tendency for TB Caucasians and African Americans have a larger chest volume than Native Americans and Asians Size of thoracic chest cavity and vital lung capacity varies by culture |
|
|
History Questions to ask |
Cough, Shortness of breath, Chest Pain, Past hx of respiratory infections, Family hx of allergies, asthma, TB, Smoking hx, Environmental exposure, Self-care behavior |
|
|
Tactile fremitus |
palpable vibration ("99") |
|
|
Adventitious Sounds |
1. Crackles (or rales) - popping noises associated with moisture in lungs 2. Wheezing - high pitched squeak, constriction 3. Coarse/rhonchi - low pitched hoarse sounds 4. Bronchophony - pt repeats "99" 5. Egophony - saying "eeee" 6. Whispered pectoriloquy - pt whispers "123" |
|
|
Barrel Chest |
Ribs are horizontal rather than downward slope, with a costal angle of >90 degrees. |
|
|
Pectus carinatum |
Pigeon breast/chest -- forward protusion of the sternum |
|
|
Tachypnea |
Increased RR, rapid/shallow breathing |
|
|
Bradypnea |
Slow breathing pattern, decreased RR, less than 10 breaths per minute |
|
|
Cheyne-Stokes respirations |
Respirations gradually wax and wane, occurs in a regular pattern with periods of apnea |
|
|
Pleural effusion |
excess fluid collecting in the intrapleural space (crackles with dullness) |
|
|
Pneumothorax |
Free air in the pleural space that causes lung collaspe (you hear nothing on the lung with the collaspe) |
|
|
Tuberculosis |
Positive PPD and CXR (skin test and chest x-ray), very contagious, productive cough with serum |
|
|
Bronchitis |
Inflammation of bronchi, may have partial obstruction of bronchi. Characterized by hacking, mucousy wet, productive cough. |
|
|
Pneumonia |
Infection of the lungs, alveoli becomes consolidated with bacteria and fluids Has a high fever |
|
|
Asthma |
Reactive airway disease, allergic response or hypersensitivity to allergins. Characterized by bronchospasm, inflammation, very thick mucous production (wheezes expiratory) |
|
|
Type of Artery (9) |
1. Temporal artery 2. Carotid artery 3. Brachial artery 4. Radial artery 5. Ulnar artery 6. Femoral artery 7. Popliteal artery 8. Posterior tibialis 9. Dorsal pedis |
|
|
History for Peripheral Vascular |
Ask for any leg cramps Any skin changes, color, temperature, sores. Ask for swellings Ask medications Any lymph nodes enlargements |
|
|
Allen's Test |
Checks intact of Radial and Ulnar arteries You compress both the radial and ulnar arteries and release individually to check for blood flow in each |
|
|
Raynaud's Test |
Decreased circulation in the hands and sometimes feet. Noticeable with cyanosis, discoloring from the cold/stress/vibrations
Pain and numbness with decreased circulation |
|
|
Lymphedema |
Abnormal drainage of lymph causing build up in interstitial spaces, raising osmotic pressure and promoting fluid leakage |
|
|
Arteriosclerosis/Ischemic Ulcer |
Build up of fatty plaques on intima, hardening of arterial walls |
|
|
Venous statis/ulcer |
Following acute deep vein thrombosis or following chronic incompetent valves in deep vein |
|
|
Varicose veins |
Incompetent valves allow reflux in veins, producing dilated tortuous veins |
|
|
Deep vein thrombitis |
Deep vein occluded by thrombus, causing inflammation and edema |
|
|
Aneurysm |
Sac formed by dilation in artery wall |
|
|
Heart |
Located between the 2nd and the 5th intercostal spaces, R border of the sternum to the L midclavicular line Top is the base, bottom is the apex |
|
|
Precordium |
Area on anterior chest overlying the heart and great vessels |
|
|
Apical Impulse |
Apex of the heart beats against the chest wall, palpable between the 5th intercostal space |
|
|
Great vessels |
Lie bunched above the base of the heart |
|
|
Superior vena cava/Inferior vena cava |
Returns unoxygenated blood to the right side of the heart |
|
|
Pulmonary Artery |
Leaves R ventricle, carries blood to the lungs |
|
|
Pulmonary Vein |
Brings blood from the lungs, freshly oxygenated, to the L side of the heart |
|
|
Aorta |
Carries freshly oxygenated blood to the Left side of the heart to the body |
|
|
Pericardium |
Tough, fibrous, double walled sac that surrounds and protects the heart |
|
|
Myocardium |
Muscular wall of the heart, does all of the pumping! Contracts |
|
|
Endocardium |
Thin layer of endothelial tissue, lines inner surface of heart chambers and valves |
|
|
Valves |
Atrioventricular Valve (Tricuspid Valve, R AV Valve, Mitral Valve, L AV Valve) Semilunar Valve (Pulmonic Valve, R side of heart, Aortic Valve, L side of heart) |
|
|
Diastole |
AV valves open, the filling stage! |
|
|
Systole |
AV valves close, to prevent regurgitation of blood back into the atria |
|
|
Which side of the heart delivers blood where? |
Right side of the heart delivers blood up to the lungs, which returns to the left side. Left side of the heart delivers blood to the rest of the body. |
|
|
Normal Heart Sounds |
S1 - 1st heart sound, "lub", this is the sound of AV valves all closing. This starts systole -- loudest at apex S2 - 2nd heart sound, "dub", this is the closing of the semi-lunar valves, end of systole |
|
|
Abnormal Heart Sounds |
S3 - vibrations occurring during ventricular filling S4 - atria contract and pushes blood into a noncompliant ventricle creating vibrations Murmurs - turbulent blood flow and collision currents. Causes gentle blowing, swooshing sounds |
|
|
Neck Vessels |
Carotid Artery Internal jugular External jugular |
|
|
Cultural considerations with HTN |
African Americans, Mexican Americans, and Native Americans have higher incidence than Whites |
|
|
Cultural Considerations with Smoking |
In Adults, African American and Native American has higher incidence than White In Young Adult (18-24), White males and females have higher incidence of smoking than minority young adults |
|
|
Cultural considerations with Cholesterol |
White males and Mexican American have higher incidence than African Americans in adulthood |
|
|
Obesity |
African American males/females and Mexican American males -- 64% White males -- 62% Hispanic females -- 56% White females -- 43% Asian males -- 35% Asian females -- 25% |
|
|
What should you ask for cardiac hx? |
Hx of chest pain/tightness? Dyspnea/shortness of breath Orthopnea Cough Fatigue Cyanosis Edema Nocturia (waking up to pee) Past cardiac hx (HTN, elevated blood cholesterol, elevated triglycerides, heart murmur, congenital heart disease, rheumatic fever) Family hx (HTN, obesity, diabetes, coronary artery disease, sudden death) Self-care habits |
|
|
What are the grades for heart murmurs? |
Grade I/VI - barely audile Grade II/VI - clearly audible but faint Grade III/VI - moderately loud, easy to hear Grade IV/VI - loud, associated with a thrill palpable Grade V/VI - very loud, heart with 1 corner of stethescope lifted off chest wall, palpable thrill Grade VI/VI - loud, doesn't need stethescope, palpable thrill |
|
|
Common Heart Abnormalities |
Patent Ductus Arteriosus (PDA) Atrial Septal Defect (ASD) Ventricular Septal Defect (VSD) Tetralogy of Fallot Coarctation of the Aorta Mitral Regurgitation Congestive Heart Failure |
|
|
Patent Ductus Arteriosus (PDA) |
normal in fetus, spontaneously closes at birth so that blood is redirected to the lungs |
|
|
Atrial Septal Defect |
Abnormal opening of the atrial septum resulting usually in L to R shunt and causes a large increase in pulmonary blood flow |
|
|
Ventricular Septal Defect |
Abnormal opening in septum between ventricles |
|
|
Tetralogy of Fallot |
shunts a lot of venous blood directly into aorta away from pulmonary system so that blood never gets properly oxygenated 1. R ventricular outflow stenosis 2. VSD 3. R ventricular hypertrophy 4. Overriding aorta |
|
|
Coarctation of the Aorta |
Severe narrowing of descending aorta, increases workload of L ventricle -- picked up on lower extremities has a lower pulse |
|
|
Mitral Regurgitation |
Stream of blood regurgitates back into L atria during systole through incompetent mitral valve; in diastole, blood passes back into L ventricle again with new flow |
|
|
Congestive Heart Failure (CHF) |
heart's inability to pump enough blood to meet metabolic demands of the body. Kidney' compensatory mechanisms of abnormal retention of Na and H2O to compensate for decreased CO2. |
|
|
Types of Communication |
Verbal: Most direct interpretation, directly speaking to patient Non-Verbal: less conscious control, more reflective of feelings. Includes body language |
|
|
Internal factors for effective communication |
1. Genuinely liking people 2. Empathy (not feeling like someone, but feeling with) 3. Ability to listen, pay attention! |
|
|
External factors for effective communication |
1. Privacy 2. Minimal interruptions, limit distractions 3. Comfort/room temperature 4. Sufficient lighting, enough to see facial expressions 5. Seating, sit to eye level 6. Note taking, minimal notes |
|
|
Key points for Introduction to patient |
Introduce yourself! State name and your title. Provide direction for what is about to happen. |
|
|
Open-ended questions |
These are good! Allow the patient to provide broad background information in narrative form |
|
|
Closed-ended questions |
These are also good! Give direct, clear answers for specific information |
|
|
Good techniques for Data Collection |
1. Choosing language wisely (avoid medical jargon, say in layman's terms) 2. Facilitation (nodding your head) 3. Silence (allowing pt to fill in blanks) 4. Reflection (repeating back for clarification) 5. Empathy 6. Clarification (try to clear up info) 7. Confrontation (ex "you look tired") 8. Interpretation (drawing an inference/conclusion) |
|
|
Bad techniques to avoid for Data Collection |
1. False reassurance 2. Unwanted/unsolicitated advice (try to be as objective as possible!) 3. Using authority (ex "because I said so") 4. Avoidance language (slang "passed on") 5. Distancing (try to act personal) 6. Professional jargon (don't use scientific terms pt wouldn't understand) 7. Leading/biased questions (ex "you don't smoke, do you?") 8. Talking too much 9. Interrupting 10. "Why" questions (ex "why would you do this..") |
|
|
Examples for non-verbal cues |
1. Appearance - appear very professional and approachable 2. Posture - appear CONFIDENT! 3. Gestures - facilitating gestures 4. Facial expression - attentive, be sincere 5. Eye contact - appear interested but not intimidating 6. Voice - calm smooth 7. Tough - avoid initially until introducing yourself to your patient |
|
|
How should you close an interview? |
Always close an interview by thanking the patient and asking if they have any additional questions or requests! Give direction for what the next step will be. |
|
|
What are the 4 types of health histories? |
1. Complete Health History - biographical data, baseline 2. Focused Health History - focuses on 1 or 2 systems, limited short-term problem 3. Follow-Up Health History - short term or chronic illnesses, to evaluate any changes 4. Emergency Health History - emergency situations, allergies |
|
|
Why do we ask for patient history? |
This is to help individualize a care plan so that we can create a report |
|
|
What is included in biographical data? |
Name, DOB, gender, ethnic background, address, etc |
|
|
Chief Complaint |
Should always be in quotations! Exact words! This is a brief statement of why the patient is asking for care |
|
|
History of Present Illness |
1. Quality/Character 2. Severity 3. Location 4. Timing (onset, duration, frequency) 5. Patient Perception 6. Aggravating/Relieving Factors 7. Associated Factors 8. Radiation 9. Setting |
|
|
Childhood Illnesses to always ask for |
Measles Mumps Rubella Pertussis Scarlet fever Varicella |
|
|
Past Health to ask for |
Childhood illnesses Hospitalizations Operations Accidents/Injuries Serious/Chronic illnesses Obstetric History Immunizations Last exam date (physical, dental, vision, hearing) Allergies Medications |
|
|
What family history should you ask for? |
Ask for any disease processes that run in the family, anything genetic - If wanted, ask for a genogram! |
|
|
Psychosocial/Functional Health History |
1. Education 2. Activity/Exercise 3. Sleep/Rest 4. Nutrition 5. Roles and Relationships 6. Coping/Stress Management 7. Spiritual Resources 8. Personal habits 9. Occupational health 10. Environmental Hazards 11. Domestic Violence |
|
|
How should you document everything? |
Include a section for subjective, objective, assessment, and plan. SOAP Be very clear, accurate, and include pertinent negatives if needed. |
|
|
What is the platinum rule? |
Treat others as THEY want to be treated! |
|
|
Transcultural nursing |
strategy of caring that incorporates sensitivity and consideration of a patient's culture, values, beliefs, and practices
-- caring for the patient as they want to be cared for |
|
|
Cultural Assessment |
ACCESS 1. Assessment 2. Communication 3. Cultural negotiations/compromise 4. Establishing respect and rapport 5. Sensitivity 6. Safety |
|
|
What cultural goals should a nurse strive for? |
Culturally competent careAvoiding ethnocentrisim (which is a tendency to thinking your own way of life is the best way)Avoiding cultural imposition (imposing your beliefs, values, and patterns of behavior onto another culture)
|
|
|
Solid viscera |
Liver, pancreas, spleen, adrenal glands, kidneys, ovaries, uterus |
|
|
Hollow viscera |
Stomach, gallbladder, small intestine, colon, and bladder |
|
|
Four quadrants for the abdomen |
RUQ - liver, gallbladder, duodenum, head of pancreas, right kidney, part of ascending and transverse colon LUQ - stomach, spleen, L lobe of liver, body of pancreas, L kidney and adrenal, part of transverse and descending colon RLQ - cecum, R ovary, R ureter, R spermatic cord LLQ - part of descending colon, sigmoid, colon, L ovary, L ureter, L spermatic cord |
|
|
History questions to ask for abdomen |
1. Any change in appetite or weight loss 2. Dysphagia 3. Food Intolerance 4. Abdominal Pain 5. Nausea/Vomiting 6. Bowel Habits 7. Past Abdominal History 8. Medications 9. Nutritional Assessment -- 24hr recall |
|
|
Ascities |
Collection of excess fluid in the abdomen, leads to abdomen distention |
|
|
Constipation |
Bowels are evacuated within a long interval with difficulty straining. Stool is usually very hard! |
|
|
Umbilical hernia |
Soft skin covered mass with a protrusion of the intestine through a weakness or incomplete closure in the unbilical ring. This is reducable! |
|
|
Hepatitis |
Inflammation of the liver. Includes a enlarged liver and seen by heptatomegaly and jaundice |
|
|
Gastroesophageal Reflux |
Symptoms include esophatitis, heartburn that occurs 30-60 minutes after eating, and is more aggravated by lying down or bending over. |
|
|
Aortic Aneurysm |
80% palpable during an exam. Feels like a pulsating mass in the abdomen. Shows positive bruit and decreased femoral pulses |
|
|
Appendicitis |
Starts as a dull, diffuse pain in periumbilical region that shifts to a severe, sharp pain localized in RLQ. Aggravated by movement, coughing, fever |
|
|
Gastroenteritis/Gastritis (AGE) |
diffuse generalized abdominal pain with nausea and diarrhea |
|
|
Cholecystitis |
sudden pain in RUQ that could radiate to right and left scapula |
|
|
Rebound Tenderness |
Occurs when you press down and pain is felt when pressure is relieved |
|
|
Inspiratory Arrest |
Hold fingers under the liver border and have the patient take a deep breath in and no pain is felt |
|
|
Iliopsoas Muscle Test |
Lift RIGHT straight up and push down over the lower part while the pt resists. Normal is that NO pain is felt when pressure is pushed down |
|
|
Obturator Test |
Lift RIGHT leg up, flex at hip at a 90 degrees angle at the knee and rotate leg internally and externally |
|
|
Waist to hip ratio |
< 0.80 = normal range 0.81 - 0.84 = overweight 0.85 < = obesity |
|
|
What does the general survey accomplish? |
General Survey accomplishes the overall picture of a patient's health status -- includes general health and any obvious, observable physical characteristics |
|
|
Pretibial edema scale |
Edema is for pitting 1+ mild pitting, slight indentation, no swelling of leg 2+ moderate pitting, induration subsides rapidly 3+ deep pitting, indentation remains for a long time, leg appears swollen 4+ severe pitting, indentation lasts for a long time, leg is very swollen |
|
|
Functions of the Skin |
1. Protection - decreases injuries 2. Barrier - prevents any penetration 3. Temperature Regulation 4. Wound Repair 5. Absorption/Excretion 6. Production of Vitamin D 7. Perception/Sensation 8. Identification 9. Communication - expresses emotions |
|
|
3 Layers of the Skin |
Epidermis, Dermis, Subcutaneous Epidermis - outer most layer, consisted mostly of keratin, melanin, carotene pigment from basal cell layer // stratum corneum - horny cell layer consisting of dead keratinized cells Dermis - inner supportive layer, consists of collagen connectivity layers Subcutaneous - fatty layer |
|
|
Appendages of the skin |
1. Hair 2. Nails 3. Sebaceous Glands - secretes sebum 4. Sweat Glands |
|
|
Different types of Sweat Glands |
1. Eccrine glands - produces sweat 2. Apocrine glands - produces a more milky thick secretion that is activated in puberty |
|
|
What should you check for IV? |
Check for drainage, tenderness, erythema, if it is transparent, leaking |

