![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
166 Cards in this Set
- Front
- Back
|
What does the MS system consists of?
|
bones, joints, muscles
|
|
|
effects of MS system
|
encase & protect vital organs
movement support erect body produce red blood cells in bone marrow mineral storage |
|
|
synovial joints
|
*freely moveable
-articulating bones do not touch each other and are covered by cartilage -synovial membrane lines cavity and secretes synovial fluid -joint capsule surrounds synovial membrane, strengthened by ligaments |
|
|
cartilaginous joints
|
*slightly moveable
-fribrocartilaginous discs separate bony surfaces -nucleus pulposus serves as cushion/shock absorber e.g. spine |
|
|
fibrous joints
|
*no appreciable movement
-bones almost in direct contact e.g. skull |
|
|
types of synovial joints
|
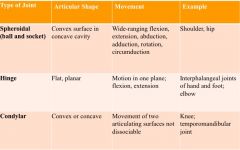
|
|
|
structure and function of joints
|
bursae--
synovial sac, allows adjacent muscles/muscles and tendons to glide over each other ligaments-- collagen fibrils connecting bones tendons-- collagen fibers connecting bones to muscles |
|
|
skeletal muscle movements
|
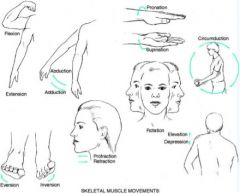
|
|
|
MS subjective data
|
joints- pain, stiffness, swelling?
muscles- pain, weakness? bones- pain, deformity, trauma? function- daily activities? self-care behaviors- exercise, nutrition? |
|
|
approach to MS exam
|
head to toe
proximal to distal joint should be examined at rest muscles should be soft and relaxed compare structure and function bilaterally |
|
|
"boggy" joints
|
thick/inflamed synovial membrane >> tenderness
|
|
|
MS exam order
|
inspect- size and contour, skin and tissues
palpate- skin temperature, muscles, boney articulations ROM- assess for pain, crepitus (palpable crunching, occurs when articular surfaces of joints get roughened) >> once you meet resistance, switch to passive muscle testing- apply opposing force, grade muscle strength |
|
|
muscle strength
|
0- no contraction, complete paralysis
1- slight contraction, severe weakness, no extremity movement 2- passive motion (full ROM, eliminate gravity) 3- moderate weakness (full ROM but not against resistance) 4- full ROM w/ some resistance 5- full ROM w/ full resistance |
|
|
TMJ
|
*most active in body
-swelling and tenderness associated w/ inflammation and arthritis expected ROM -protract & retract lower jaw -move jaw side to side |
|
|
glenohumeral joint
|

*shoulder, ball and socket
-subacromial bursa; hurts to raise arm during inflammation -surrounded by rotator cuff muscles; if surgery is needed at this site, a piece of acromion will be severed due to irritation to bursa inspect shoulders and axilla expected ROM -circumduction -abduct & adduct arms -external rotation & internal rotation |
|
|
elbow joint
|
*humerus w/ radius and ulna, hinge
-olecranon bursa -ulnar n. runs posteriorly to olecrannon process and medial epicondyle inspect joint in flexed & extended positions palpate joint & boney prominences expected ROM -extend & flex elbow -pronate & supinate hand |
|
|
T/F. There are ~206 bones in the body, half of which are localized in the hands and feet.
|
True
|
|
|
What nerve innervates the hand?
|
median n.
palm of hand palmar surface of thumb, 2nd, 3rd, and half of 4th digit |
|
|
wrist/hand tendons
|
6 extensor tendons
2 flexor tendons >>passes through wrist and enters the finger inflammation in carpal tunnel can spread to tendon sheaths |
|
|
wrist/hand joints
|
radiocarpal joint
MCP- metacarpophalangeal joint DIP- distal interphalangeal joint PIP- proximal interphalangeal joint inspect dorsal and palmar surfaces of joints expected ROM -extend/flex hand -ulnar & radial deviation -spread fingers -make fist -touch thumb to each finger |
|
|
phalen's test
|
dorsal surfaces of hands touch one another for 60 seconds
if pt feels numbness/tenderness >> median n. is compressed (+) carpal tunnel |
|
|
tinel's sign
|
tap wrist for numbness
|
|
|
osteoarthritis (degenerative joint disease)
|
cartilage goes through destruction due to age >> new bone growth is abnormal
-hard, nontender nodules (2-3 mm) -herbenden's nodes (DIP) -bouchard's nodes (PIP) |
|
|
rheumatoid arthritis
|
autoimmune disease; synovial membrane gets inflamed, forms cyst & erosion >> overgrowth of fibrous tissue
*atrophy of muscles in between joints -symmetric involvement -tender, painful, stiff joints -swollen, red, warm -PIP and MCP -boutenniere deformity -swan neck deformity -ulnar deviation @ MCP |
|
|
boutonniere v. swan neck deformity
|
boutonniere--
flexion of PIP; hyperextension of DIP swan neck-- flexion of DIP; hyperextension of PIP |
|
|
hip joint
|
*acetabulum and femur
inspect while erect palpate while supine expected ROM -extension & flexion -external & internal rotation w/ knee -abduction & adduction -hyperextension |
|
|
knee joint
|
*femur and tibia; along w/ knee cap
-prepatella pouch is largest synovial cavity in body -bursa cups up and behind quadricep muscle -medial & lateral meniscus cushions tibia and femur -stabilized by cruciate ligaments (criss crossed to provide anterior and posterior stabilization) inspect joint and muscle expected ROM -extension & flexion -hyperextension |
|
|
tibiatalus joint
|
*ankle
*tibia & fibula and talus expected ROM -dosi & plantar flexion -inversion & eversion |
|
|
spine
|
cervical 7
thoracic 12 lumbar 5 sacral 5 coccyx 3-4 intervertebral discs are the joints of the spine large muscles include the trapezius and latissimus dorsi L4 is top of iliac crest |
|
|
cervical spine
|

inspect alignment of head & neck
palpate spinous processes and muscles expected ROM -extension & flexion (chin to chest) -lateral rotation (ear to shoulder) -rotation (chin to shoulder) |
|
|
spine
|
inspect while erect
palpate spinous processes expected ROM; hold patient's iliac spine while they perform ROM -flexion/extension -lateral bending -rotation |
|
|
CNS v. PNS
|
CNS- brain and spinal column
PNS- cranial nerves that extend |
|
|
cerebral cortex
|
*primarily gray matter
cerebrum- outer layer, highest functioning, greatest mass of brain tissue, divided into two hemisphere; L is dominant in 95% of people even if they are L handed frontal lobe parietal lobe occipital lobe wernicke's area broca's area |
|
|
diencephalon
|
*deep in brain, additional gray matter
basal ganglia- automatic movement (e.g. Parkinson's) thalamus- relay system hypothalamus- maintains homeostasis (VS), endocrine system, & some emotional behavior |
|
|
brainstem
|
*central, core of brain; mostly nerve fibers
midbrain- most anterior, has basic tubular structure of spinal cord, merges w/ thalamus and hypothalamus pons- ascending and descending tracts medulla- continuation of spinal cord *pyrimidal decussation- where crossing over occurs |
|
|
cerebellum
|
base of brain, movement coordination, unconscious
|
|
|
spinal cord
|
spans from medulla to L1/L2; this is why punctures are done at L3/L4 level
pathways to connect to PNS |
|
|
broca's area v. wernicke's area
|
broca's *speech formation
patient have trouble speaking even if they know what they want to say wernicke's *speech comprehension patient can hear but will not understand |
|
|
frontal lobe
|
personality
behavior emotional intellectual |
|
|
temporal
|
hearing
taste smell |
|
|
precentral gyrus v. postcentral gyrus
|
precentral- primary motor area
postcentral- primary sensory area |
|
|
upper motor neurons
|
*CNS
located in cerebral cortex, brainstem >cranial n. synapse w/ motor neurons in the brain stem >peripheral n. synapse @ spinal cord |
|
|
lower motor neurons
|
*PNS
have cell bodies in spinal cord that transmit via anterior root |
|
|
major motor pathways
|
corticospinal/pyramidal tract
extrapyramidal tract cerebellar system |
|
|
corticospinal/pyramidal tract
|
-cortex to spine
-mediates voluntary movement -integrates skilled and discrete purposeful movement (e.g. writing) -info regarding muscle tone; motor fibers >> cross @ medulla >> synapse @ anterior horn |
|
|
extrapyramidal tract
|
-originate @ motor cortex, basal ganglia, brain stem, & spinal cord
-primitive -maintains muscle tone & gross autonomic movements |
|
|
cerebellar system
|
-receives sensory & motor
-coordinate movements, maintain posture -info re position of muscles and joints |
|
|
major sensory pathways
|
spinothalamic
posterior/dorsal column |
|
|
spinothalamic tract
|
sensory info travel via afferent fibers, PNS, goes into posterior portion of spinal column, up the spinal cord
pain, temperature, light touch (crude), synapses & crosses over >> thalamus, basic quality >> cortex, fine discrimination |
|
|
posterior/dorsal column
|
position, vibration, and fine localized touch
>> medulla, synapse and crosses over >> thalamus |
|
|
five requirements for reflex
|
1/ intact sensory n.
2/ functional synapse 3/ intact motor fiber 4/ intact neural muscular junction 5/ competent muscle |
|
|
PNS
|
cranial nerves
spinal nerves reflex arc |
|
|
reflex arc
|
-deep tendon
-involuntary -1 motor, 1 sensory, *only one synapse |
|
|
origination of nerves
|
CN I- fiber tract
CN II-XII- brainstem and diencephalon |
|
|
spinal column
|
8 cervical
12 thoracic 5 lumbar 5 sacral 1 coccygeal |
|
|
dermatome
|
band of skin innervated by single spinal nerve; overlap occurs as biological insurance
arms- cervical nerves legs- lumbar nerves |
|
|
neuro subjective data
|
1/ headache
2/ head injury, LOC? 3/ dizziness, vertigo 4/ seizures 5/ tremors 6/ weakness 7/ incoordination 8/ numbness, tingling 9/ difficulty swallowing 10/ difficulty speaking 11/ h/o CVA, meningitis 12/ environmental, occupational hazards |
|
|
neuro exam components
|
1/ mental status
2/ cranial nerves 3/ motor 4/ sensory 5/ coordination 6/ romberg/gait 7/ DTRs >>always consider symmetry and whether it's an upper or lower nerve problem |
|
|
mental status
|
general appearance & behavior
level of consciousness orientation attention- months in reverse, # span language- fluent, hesitant, read & can follow directions memory |
|
|
level of consciousness
|
alert
lethargic- drowsy obtunded- eyes open, slow response, confused stuporous- arise only to painful stimulus comatose- does not wake up |
|
|
Why don't we use ammonia to test CN I?
|
Besides being uncomfortable, it affects CN V.
|
|
|
ptosis
|
drooping of the eyes
|
|
|
Which CN is convergence checking for?
|
CN IV
|
|
|
How do you test for the vestibular portion of CN VIII?
|
(+) Romberg- loss of balance when patient stands with eyes closed
some people will sway, this is not a (+) Romberg |
|
|
CN IX
|
glossopharyngeal
sensory-- sensation in posterior 1/3 tongue, oropharynx, soft palate, vocal cords, & epiglottis taste in 1/3 of tongue motor-- innervates stylopharyngeus muscle |
|
|
CN X
|
sensory and motor fibers to muscles of palate and oropharynx
give rise to superior and inferior laryngeal nerve watch elevation of uvula; gag reflex in commatose patients |
|
|
motor system
|
inspect & palpate
size, contour tone strength involuntary movements |
|
|
muscle tone
|
spastic- increased resistance to passive lengthening, may suddenly give way "clasp-knife phenomenon"
rigid- constant state of resistance, basal ganglia system cogwheel rigidity is associated w/ parkinson's flaccid- limp, soft, flabby, weak, & easily fatigued |
|
|
muscle tone r/t nerve damage
|
damage to upper neurons (CNS) >> increased tone; rigidity and spastic
damage to lower neurons (PNS) >> decreased tone; flaccid |
|
|
abnormal muscle functions
|
fasciculation- rapid twitching
tics- twitching of muscle group @ inappropriate times, could be neuro or psychological myoclonus- sudden jerk e.g. seizure, hiccup tremors- oscillating movements caused by involuntary contraction of muscle groups (fine and resting) tetany- muscle spasms that may occur w/ tetany, hypo-calcemia or magnesium |
|
|
tests for fine discrimination
|
stereognosis
graphesthesia two-point discrimination extinction- simultaneously touch corresponding areas bilaterally |
|
|
dysdiadochokinesia
|
inability to arrest abruptly one motor imp use and substitute its opposite
e.g. pronation/supination |
|
|
dysergia v. dysmetria
|
dysergia- improper coordinated function of given muscle groups
dysmetria- inability to gauge the distance b/w two points or objects |
|
|
grading reflexes
|
0 no response
1+ diminished 2+ normal 3+/4+ hyperactive, may indicate disease >> test for clonus |
|
|
How do you test for clonus?
|
support knee
abruptly dorsiflex foot (+) clonus- limb will oscillate |
|
|
superficial reflexes
|
abdominal- stroke near umbilicus >> muscles should contract
cremasteric- lightly stroke the superior and medial thigh >> testicle should rise up plantar- toes should curl in; (+) babinski if toes go up, normal only in children >> upper neuron problem in adults |
|
|
What is more likely to occur if a child gets injured?
|
They are more likely to break the bone and less likely to have fractures/sprains b/c their ligaments and tendons are stronger.
|
|
|
T/F. There are more bones in the child's skeleton than the adult.
|
True; these bones will fuse throughout development
|
|
|
metaphysis
|
growth plate
|
|
|
What shape is the spine at birth?
|
C-shape; curves develop when you get strength at head and lowerback
|
|
|
A/N. Foot of the infant appears flat.
|
Normal
pes planus- until age 3 pigeon toes or toeing in can also be normal |
|
|
galeazzi test
|
difference in knee height
hip dysplagia- easily dislocated >> knee will be lower |
|
|
peds hip
|
barlow maneuver- adduct hip while pushing thigh posteriorly >> if it goes out of socket >> dislocatable (+)
ortolani maneuver- abduct thighs and apply downward pressure; this reduces the dislocated hip |
|
|
A/N. Lordosis is common in adolescents.
|
Abnormal
lordosis is common in toddlerhood scoliosis is common in adolescents as a result of the growth spurt |
|
|
genu varum v. genu valgum
|
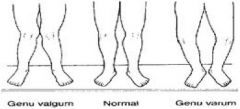
varum- bowlegged; normal until 2/3 yrs
valgum- knock kneed; prominent during 3/4 yrs and can be normal until 6/7 yrs |
|
|
nursemaid's elbow
|
subluxation of radial head; can go in and out, this is not considered a dislocation
child will present flexed and pronated |
|
|
How do you test for scoliosis?
|
forward bend test; look for asymmetry of scapula
|
|
|
What scale is used to classify growth plate fractures?
|
salter-harris classifications
|
|
|
palmar & plantar reflex
|
palmar- baby will grab hand; until 3/4 months
plantar- toes will curve inward w/ applied pressure at bottom of foot; until 8/10 months present at birth |
|
|
moro
|
if you pretend to drop them--baby will be startled and their hands will be spread out
extinguishes 4/6 mos |
|
|
atonic neck reflex
|

fencing pose
extinguishes 4/6 mos |
|
|
babinski reflex
|
stroking of lateral plantar surface >> up going of great toe and fanning out of other toes
extinguishes 2 yrs |
|
|
swimmer's (galant) response
|
hold baby prone while supporting belly w/ hand; stroke along one side of spine >> baby flexes body toward the stroked side
extinguishes 3/4 mos |
|
|
parachute reflex
|
symmetrical/protective
*appears at 6/8 mos; does not disappear |
|
|
gower's sign
|
weak pelvic muscles
muscular dystrophy |
|
|
female genitalia subjective
|
menstrual history
obstetric history sexual activity self-care behavior urinary symptoms vaginal discharge contraceptive use STI |
|
|
menarche
|
norms--
onset 9-16 yrs cycle 24-32 days duration 3-7 days ask about flow; # of pads and tampons |
|
|
menopause
|
no bleeding for 12 consecutive months
~45-52 yrs usually follow pattern of mother's |
|
|
sexual history
|
*be professional and ask everyone the same questions
sexually active? men, women, both? # of partners? >5? want to be pregnant? contraceptive? STI? if more than 5 partners, higher risk for HPV and abnormal pap smears |
|
|
chlamydia
|
most common
asymptomatic in females 40% w/ chlamydia >> pelvic inflammation 20% w/ chlamydia >> infertile |
|
|
hernias in females
|
less common; if (+) for hernia, usually femoral
patient should be standing for examination painful patient can lose blood supply and become gangrene due to obesity, heavy lifting, and ascite palpate labia majora just upward & lateral to pubic tubercles |
|
|
urethritis
|
insert finger into vagina and milk urethra gently from inside outward; culture the discharge @ skene gland
|
|
|
external female genitalia
|
mons pubis
labia majora labia minora vestibule introitus perineum anus urethral opening |
|
|
mons pubis
|
hair/fat pad that overlies synthesis pubis
>> look for hair distribution female- upside down triangle shape male- diamond shape |
|
|
labia majora v. labia minora
|
majora- rounded folds of adipose tissue
minora- thinner; forms clitoris >> should be symmetrical, plump, well formed |
|
|
vestibule
|
boat shaped facia b/w labia minora
|
|
|
introitus
|
posterior vaginal opening
>> should not see bulges; if present 1/ cystoceal- bladder going into vagina 2/ erectusceal- rectum coming up against vagina 3/ prolapsed uterus- uterus into vagina |
|
|
perineum
|
vestibule to anus
|
|
|
urethral opening
|
located b/w vestibule and vaginal opening
opens up into vestibule skene glands- on both sides of urethral opening, empties into urethra >> swollen red urethral meatus may indicate prolapse |
|
|
bartholin gland
|
secretes mucus to lubricate vagina
|
|
|
internal female genitalia
|
vagina
uterus fallopian tubes ovary adnexa |
|
|
uterus
|
flattened fibrous muscular structure consisting of
1/ cervix- protrudes into vagina 2/ fundus- body; upper part of uterus >>when uterus is in abnormal position, may cause intense cramps during menstrual period |
|
|
vagina
|
-hollow tube extending b/w urethra and rectum
-terminates at fornix of cervix -rugae is fold of tissues, expandable |
|
|
ovaries
|
3.5 x 2 cm; palpable during reproductive years
|
|
|
cervix
|
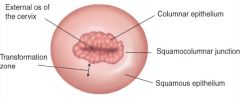
columnar epithelium- more red
*squamocolumnar junction- site of pap smears, common site of cancer squamous epithelium- more smooth >> as you age, columnar epithelium moves toward uterus and is not as visible |
|
|
anus
|
coarser skin and increased pigmentation in comparison w/ rest of genitalia
|
|
|
T/F. Younger women get more genital infections than older women.
|
False; older women have less estrogen and are more likely to be infected
|
|
|
penis and bladder
|
shaft is composed of 3 columns of erectile tissues
1 corpus spongiosum- on both sides of urethra, forms glans 2 corpora cavernosa- on top of shaft, forms base of glans glans- bulb of penis prepuce- foreskin urethral meatus |
|
|
lower genitourinary tract
|
scrotum- loose pouch, divided into two for each teste
epididymis- posterior of testes; long tubular structure testes- L is usually lower than R, can be different sizes, ~4.5cm vas deferens- begins @ tail of epididymis, ascends to scrotal sac, passes iguinal canal, to ABD prostate |
|
|
landmarks of groin
|
inguinal ligament connects anterior superior iliac spine & public tubercle; right on top of this is the inguinal canal
|
|
|
inguinal canal
|
has two openings
1/ external inguinal ring- palpable 2/ internal inguinal ring- nonpalpable |
|
|
How do you find femoral canal to check for femoral hernias?
|
Place index finger on femoral artery
3rd finger will be placed on vein pinky will be on canal >> ask patient to cough or bear down; if you feel bulge, possible hernia |
|
|
male genitalia subjective
|
frequency, urgency, nocturia, hesistency can all be signs of an enlarged prostate
dsyuria urine color penis pain, lesion, discharge sexual activity and contraceptive use STI |
|
|
inspecting the corona
|
-check for scars and nodules
-urethra should be centered -testes should feel oval, rubbery & oval // epididymis should be palpable; describe to patient as "egg w/o shell" -scrotum may be more taut in CHF or ESRD patients if there is edema in that area |
|
|
How do you inspect a uncircumcised penis?
|
ask patient to pull back foreskin and check for smegma
smegma- secretion in foreskin; cheesy whitish color is normal |
|
|
inspecting the urethra
|
should be in the middle of urethral meatus
red w/ no discharge |
|
|
How do you check for hernia in men?
|
have patient stand, placing their weight on L leg so the R side is relaxed
invaginate fingers to palpate external ring (+) if you feel tap/push when they cough or bear-down |
|
|
indirect v. direct hernias
|
indirect-- "tap"
most common 60% usually occurs in infants, males 16-20 yrs if no pain/discomfort, not too concerning but it can come down the tunnel and become a direct hernia direct-- "push" 40+; ascites, obesity uncommon, associated w/ little pain goes OVER the tunnel |
|
|
ascites
|
excess fluid from ABD
common in liver & kidney disease, CHF |
|
|
anus and rectum
|
anal canal--
3.5-4 cm long modified skin, no hair merges with the rectum rectum-- 12 cm attach to sigmoid colon |
|
|
internal v. external rectal sphincter
|
internal- involuntary
external- voluntary |
|
|
anal column
|
each has artery and vein
once the veins get enlarged, they can develop into hemorrhoids |
|
|
prostate
|
-anterior wall of rectum
-2cm behind symphysis pubis -surrounds bladder neck and urethra has 15-30 ducts that opens up into urethra, secreting milky alkaline fluid that helps sperm viability has 2 lobes separated by shallow groove called the median sulcus, which feels intended >>once prostate is enlarged, median sulcus is no longer palpable |
|
|
rectal subjective questions
|
usual bowel routine; 1-3 days is normal
rectal bleeding; GI bleeding >> black tarry rectal condition iron >> dark stool >> guyaic test |
|
|
inspecting the perianal area
|
skin
anal opening sacrococcygeal area valsalva maneuver |
|
|
palpating anus and rectum
|
"anal winking" anus will tighten and then relax
place index finger in the anus palpate for hemorrhoids and masses check for roughness should be smooth, even, no nodules |
|
|
palpating the prostate
|
patient should be on L side or leaning over a table
prostate protrudes into rectum ~1 cm feeling for median sulcus, should be rubbery |
|
|
guyaic test
|
occult blood
>should not turn blue |
|
|
abdomen surface landmarks
|
four layers of large, flat muscles
1/ external oblique 2/ internal oblique 3/ transversus muscle 4/ rectus abdominia >> all joined at midline by tendon seam, the linea alba |
|
|
T/F. Linea alba is darkened in pregnant women.
|
True
|
|
|
Which muscle makes up the "six pack" ?
|
rectus abdominis
a six pack makes it difficult to feel the viscera and to perform the heimlich maneuver |
|
|
Which organs expand all four quadrants?
|
small intestine
|
|
|
location of organs
|
RLQ
cecum appendix bladder, pubic symphysis RUQ liver gallbladder LUQ spleen stomach LLQ descending colon sigmoid colon |
|
|
ABD subjective
|
appetite
dysphagia food intolerance n/v/bowel habits |
|
|
ABD pain types
|
visceral- internal organ;
dull, poorly localized parietal- inflammation of overlying peritoneum; sharp, localized, aggravated by movement referred- when person gives history of ABD pain; location may not necessarily be directly over involved organ |
|
|
referred pain
|
human brain doesn't have picture of organs and will refer it to area where organ was during fetal development
*GERD- heart pancreatitis- L shoulder cholecystitis- gall bladder inflammation, back below scapula apendicitis- RLQ, upper gastric rectal- sacral kidney stones- groin/middle back |
|
|
umbilical hernia v. incisional hernia
|
umbilical- weakening in muscle wall, intestines are pushing through
incisional- intestine is putting so much pressure that the staples can no longer hold the incision together |
|
|
auscultating for bowel sounds
|
begin at ileoceccal valve in RLQ
5-30 bowel sounds/min don't have to count, just note character & frequency (e.g. absent, normal, hyperactive, hypoactive) |
|
|
hyperactive bowel sounds
|
hyperactive- "tinkling" sound
diarrhea, early intestinal obstruction |
|
|
absent bowel sounds
|
listen up to 5 minutes before saying that bowel sounds are absent
common in patients s/p surgery, peritoneal inflammation |
|
|
borborygmi bowel sounds
|
can hear w/o stethoscope; gurgling sound
|
|
|
T/F. Arterial bruits w/ a systolic component suggest a partial occlusion of aorta or large arteries.
|
Fasle; systolic and diastolic component
|
|
|
percussing the liver span
|
6-12 cm at midclavicular line
4-8 cm at midsternal line >> enlargements may indicate hepatitis patients w/ barrel chest will have livers that are slightly lower, but the range in size should be the same |
|
|
liver scratch test
|
for pregnant, obese, peritonitis, or ascite patients
place steth over liver, start from RLQ up >> when sound becomes magnified, you've found the liver |
|
|
percussing the spleen
|
ask patient to take deep breath, should hear tympani
if it changes to dullness in deep inspiration, (+) and may indicate splenomegaly |
|
|
How can you palpate patients who are ticklish?
|
place their hand on stomach and feel around it
|
|
|
solid v. fluid v. hollow organs
|
solid- liver, spleen, kidney, ovary, pancreas
fluid- gall bladder, aorta, urinary tract hollow- stomach, intestine, colon; not usually palpable |
|
|
normally palpable structures
|

xiphoid process
liver edge right kidney uterus aorta rectus muscles -colon can be felt if filled w/ stool -sacral can be felt if person is very thin -mild tenderness is normal in the sigmoid colon |
|
|
What is an indication of an enlarged liver?
|
if it is 2 cm below the ribcage
|
|
|
T/F. An enlarged spleen can reach the groin.
|
True
|
|
|
When palpating the kidneys, where do you want to position your hand?
|
use duck bill method
*should be lateral to rectus muscles |
|
|
aortic aneurysm
|
95% of ABD aneurysms are palpable
usually above umbilicus and below renal artery will hear bruit decreased femoral pusses |
|
|
tests for apendicitis
|
rebound tenderness
rovsing's sign psoas sign obturator test |
|
|
rebound tenderness v. rovsing's sign
|
rebound tenderness- when palpating on R, patient will feel pain on the R side
rovsing's sign- when palpating on R, patient will feel pain on L side |
|
|
iliopsoas muscle test v. obturator muscle test
|
iliopsoas--
patient raise R leg agains pressure if pain is felt at RLQ >> appendicitis obturator-- internal/external rotation of R hip if pain felt at RLQ >> appendicitis |
|
|
murphy's sign
|
assessing for cholecystitis- gall bladder inflammation
hook fingers to feel liver, ask patient to hold breath >> if pain causes them to hold breath, (+) |

