![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
245 Cards in this Set
- Front
- Back
|
What are the two (or 3)major divisions of the cardiovascular system? |
1. pulmonary circulation - right side of the heart, takes deoxygenated blood from the body and move it to the lungs 2. Systemic circulation - left side of the heart, takes oxygenated blood from the lungs to the rest of the body systems 3. Cardiac circulation - coronary artery to cardiac vein |
|
|
What are the 3 components of the circulatory system? |
1. Heart - pump 2. Blood vessels - passageways 3. Blood - transport medium |
|
|
How long does it take for a RBC to make a full circuit through the body and lungs? |
About 30 seconds |
|
|
What does the cardiovascular system refer to? |
The heart and the blood vessels (Not the blood) |
|
|
What are the six purposes of the circulatory system? |
1. Move oxygen and nutrients to the body's cells 2. Remove waste products, like carbon dioxide, from cells 3. Carries hormones to target tissues 4. Pick up nutrients from the digestive system 5. Maintain water balance, via kidneys 6. Thermoregulation |
|
|
In what cavity is the heart located? |
It is located in the mediastinum-the space between the lungs |
|
|
Describe the position of the heart in the mediastinum. |
It is laterally encased by the lungs, posteriorly by the thoracic vertebrae, and anteriorly by the sternum. |
|
|
How is it clinically relevant that the heart takes up almost the entire space between the vertebrae in the ribs/sternum? |
CPR-compressions squeeze the heart |
|
|
What is the function of the pericardium? |
This sack around the heart allows the heart to be with minimal friction, provides room to expand but resists excessive expansion. |
|
|
What are the two parts of the parietal pericardium? |
1. The outer dense fibrous layer, tough layer of CT-to contain movement 2. Inner serous layer, is thin, smooth, and moist |
|
|
What is in the pericardial cavity? |
It is filled with pericardial fluid-5 to 30 mL |
|
|
What are the three layers of the heart wall? |
1. Epicardium 2. Myocardium 3. Endocardium |
|
|
What are the three layers of the heart wall? |
1. Epicardium 2. Myocardium 3. Endocardium |
|
|
What is the epicardium? |
It is the outermost layer of the heart wall. It is thin, smooth, moist serous layer that covers the hard surface. |
|
|
What is the myocardium? |
It is the muscular portion of the heart wall, it contains cardiac muscle fibers |
|
|
What is the endocardium? |
It is the Smooth, endothelial cell inner lining, it is a platelet repellent and prevents blood clots |
|
|
Describe the metabolism of cardiac muscle. |
1. Completely dependent on oxygen, aerobic respiration only (lactic acid = bad) |
|
|
The aortic valve prevents blood from flowing into which heart chamber? |
Left ventricle |
|
|
Why does the left side of the heart have thicker muscles? |
The blood from the left side of the heart sends blood to body and requires a lot of energy/pressure to accomplish this. More energy requires more muscle. |
|
|
Why does the left side of the heart have thicker muscles? |
The blood from the right side of the heart sends blood to body and requires a lot of energy/pressure to accomplish this. More energy requires more muscle. |
|
|
How much more blood volume does the left side of the heart move than the right? |
The right and left move the same volume of blood. |
|
|
What are the primary functions the of tendinous cords and papillary muscle? |
1. Structural support for av valves 2. Prevent prolapse (wrong way) |
|
|
What are the primary functions the of tendinitis cords and papillary muscle? |
1. Structural support for av valves 2. Prevent prolapse (wrong way) |
|
|
What do valves do? |
Ensure one way flow. |
|
|
What causes the sounds of a heart as heard by a stethoscope? |
1. Turbulent flow of blood as valves close A. S1-louder and longer, "LUBB", closing av valves B. S2-softer and sharper, "DUPP", closing semilunar valves |
|
|
What is a stenosis? |
Incomplete opening of valve, sometimes due to fatty build-up |
|
|
The mitral/bicuspid valve prevents blood from flowing into which heart chamber? |
Left atrium |
|
|
What are the three components that make up intercalated discs? |
1. Interdigitating folds - these increase the SA of the connection 2. Desmosomes - mechanical junctions 3. Gap junctions - allow movement of ions and electricity, coordinated contraction |
|
|
What are autorhythmic cells? |
Regular, spontaneous depolarization (self-fire action potential) |
|
|
What does myogenic mean? |
Heartbeat originates in heart |
|
|
What does myogenic mean? |
Heartbeat originates in heart |
|
|
What is pacemaker potential? |
Slow drift to threshold |
|
|
What are the 5 types of autorhythmic cells? |
1. Sinoatrial node (SA Node) 2. Atrioventricular node (AV Node) 3. Bundle of His 4. Purkinje fibers 5. Cardiac |
|
|
What is the sinoatrial (SA) node |
- most important - pacemaker - initiates heartbeat - sets heart rate |
|
|
What is the sinoatrial (SA) node? |
- most important - pacemaker - initiates heartbeat - sets heart rate |
|
|
What is the atrioventricular (AV) node? |
- electrical gateway to ventricles - AV nodal delay |
|
|
What is the Bundle of His? |
- AV node to septum |
|
|
What is the Bundle of His? |
- AV node to septum |
|
|
How do the purkinje fibers ensure efficient pumping? |
- branches off bundle of His and connects to ventricle walls - 6x faster than gap junctions - extensive branching, contraction begins at apex |
|
|
What is fibrillation? |
Uncoordinated contraction of heart |
|
|
What are the 3 ion Chanel's that regulate pacemaker activity in the SA node? |
1. No voltage-gated NA+ channels - only NA+ leak channels, influx of NA+ = slow depolarization = pacemaker potential 2. Transient CA++ channel 3. Longer lasting CA++ channel |
|
|
What is a sinus rhythm? |
- normal rhythm - set by SA node - 70-80 BPM in adult |
|
|
What is an ectopic focus? |
Heart beat begins somewhere other than SA node - region of spontaneous firing (hypoxia, caffeine, nicotine, electrolyte imbalance) - nodal rhythm set by AV node - intrinsic ventricular rhythm |
|
|
What is an arrhythmia? |
Any abnormal cardiac rhythm (heart block: failure of conduction due to disease) |
|
|
What is tachycardia? |
- persistent resting heart rate above 100 - Candy due to stress, anxiety, drugs, heart disease, or rise in body temperature |
|
|
What is bradycardia? |
- A persistent, resting adult heart rate of below 60 - common in sleep and endurance trained athletes |
|
|
What three measurements does an EKG (electrocardiogram) read? |
1. P wave - impulse from SA node to atrium, signal to depolarize atrial muscle (signal to contract) 2. QRS wave - transmission through Purkinje fibers to ventricle, signal to depolarize ventricular muscle 3. T wave - recovery phase, repolarization of ventricular muscle |
|
|
Where is blood moving in the PQ segment of an EKG? |
From the atrium to the ventricle |
|
|
What are purkinje fibers? |
Bundle of His to myocardium - spread electrical signal to ventricles |
|
|
Where is the blood moving in the ST segment of an EKG? |
From the ventricles to out of the heart |
|
|
What is the resting potential of cardiac muscle? |
-90mV |
|
|
What is the action potential threshold of cardiac muscle,and what are the three phases of a cardiac muscle action potential? |
- -70mV - rising phase (NA+ channels, transient CA++ channels) - plateau phase ( long lasting Ca++ channels and decrease K+ permeability) - falling phase ( open K+ channels, close Ca++ channels) |
|
|
End-diastolic volume (EDV) |
Amount of blood in the ventricle before contraction |
|
|
End-systolic volume (ESV) |
Amount of blood in the ventricle after contraction |
|
|
Stroke volume (SV) |
Amount pumped by each ventricle per beat (EDV-ESV=SV) |
|
|
Ejection fraction |
SV/EDV - at rest ~54%, during exercise as high as 90%, diseased heart <50% |
|
|
What are the two types of extracellular fluid? |
1. Interstitial between cells 2. intravascular in blood and lymph vessels |
|
|
What two opposing forces make up the flow at capillaries? |
1. Filtration - primarily at beginning - fluid movement out of capillary - cell and protein-free filtrate enters the interstitial fluid 2. Reabsorption - primarily at end - fluid movement into capillary - from the interstitial fluid into the blood |
|
|
What is the formula for bulk flow? |
Bulk flow = filtration + reabsorption |
|
|
What are the 2 keys to efficient cardiac pumping? |
1. Coordinated contraction - both atria or both ventricles contract at once, fast spreading signal on conduction pathways, plus gap junctions 2. Top and bottom pumping - atria contract, then delay, then ventricles contract, ensures filling of ventricles and prevents backflow |
|
|
What is the role of bulk flow? |
1. Regulating distribution of ECF 2. Between plasma and interstitial fluid-particularly blood pressure/volume compensations |
|
|
What are not some of the rolls of bulk flow? |
1. Exchange of solutes-that happens mostly by passive diffusion - all solvents are moved with the water but in both directions |
|
|
What are the forces that contribute to filtration? |
1. Capillary blood pressure 2. Tissue colloidal osmotic pressure |
|
|
What are the forces that contribute to reabsorption in bulk flow? |
1. Blood colloidal osmotic pressure 2. Interstitial pressure |
|
|
What is capillary blood pressure (blood hydrostatic pressure)? |
- blood (hydrostatic) pressure inside capillaries pushing out - high on atrial end (37 mm Hg), low on venous end (17 mm Hg) - same force that drives blood flow through vessels - primary cause of filtration |
|
|
What is interstitial hydrostatic pressure (tissue hydrostatic pressure)? |
- constant along length of capillaries - pressure between tissue cells, outside of capillary - usually negligible but can be a cause of reabsorption |
|
|
What is colloidal osmotic pressure? |
1. Caused by colloidal dispersion of proteins in interstitial fluid 2. Increased concentration of proteins - decreased concentration of water - increased osmolarity of fluid 3. Drives osmosis, diffusion of water |
|
|
What is blood (plasma) colloidal osmotic pressure? |
- constant along length of capillary - proteins inside vessel = attract water into blood - primary cause of reabsorption |
|
|
What is tissue (interstitial fluid) colloidal osmotic pressure? |
- normally not very many proteins in interstitial fluid - proteins outside vessel = the attracts water into tissues - it is a weak cause of filtration - constant along length of capillary |
|
|
What are the 6 causes/influences of venous return? |
1. Pressure gradient 2. Skeletal muscle contractions 3. Venous valves 4. Cardiac suction 5. Sympathetically driven vasoconstriction 6. Thoracic pump |
|
|
What are the the 7 electrical links that ensure efficient pumping? |
1. Inter atrial pathway 2. Internodal pathway 3. AV nodal delay 4. Gap junctions 5. Fibrous skeleton 6. Bundle of His 7. Purkinje Fibers |
|
|
What thre factors control/cause blood pressure? |
1. Cardiac output 2. Blood volume 3. Peripheral resistance |
|
|
What is systolic pressure? |
BP during ventricular systole (contraction) |
|
|
What is diastolic pressure? |
BP during ventricular diastole (not contracted) |
|
|
What is a normal, young adult, BP? |
120(systolic)/75(diastolic) mm Hg |
|
|
How do you measure pulse pressure? |
Pulse pressure = systolic - diastolic - important measure of stress exerted on small arteries |
|
|
What is mean arterial pressure (MAP)? |
Measurements taken at intervals of cardiac cycle, best estimate: diastolic pressure + ( 1/3 of pulse pressure) - varies with gravity |
|
|
What is blood flow? |
Amount of blood flowing through a tissue at a given time (ml/min) |
|
|
What is perfusion? |
Rate of blood flow per given mass of tissue (ml/min/g) |
|
|
Describe the interatrial pathway. |
- SA node to left atrium - fast - ensures simultaneous contraction of atria |
|
|
Describe the internodal pathway. |
- only electrical link between atria (SA node) and ventricles |
|
|
Describe the AV nodal delay. |
- about 100 ms - allows atria to contract before ventricles |
|
|
How do gap junctions ensure efficient pumping? |
- electrical links between adjacent cardiac muscle cells ensure simultaneous contraction |
|
|
What is the fibrous skeleton? |
- separates atria and ventricles - electrically insulates atria from ventricles |
|
|
How does the bundle of His ensure efficient pumping? |
- two branches split fro AV node and 1 goes to each ventricle |
|
|
What is the Bundle of His? |
- AV node to septum |
|
|
How do the purkinje fibers ensure efficient pumping? |
- branches off bundle of His and connects to ventricle walls - 6x faster than gap junctions - extensive branching, contraction begins at apex |
|
|
What is fibrillation? |
Uncoordinated contraction of heart |
|
|
What are the 3 ion Chanel's that regulate pacemaker activity in the SA node? |
1. No voltage-gated NA+ channels - only NA+ leak channels, influx of NA+ = slow depolarization = pacemaker potential 2. Transient CA++ channel 3. Longer lasting CA++ channel |
|
|
What is a sinus rhythm? |
- normal rhythm - set by SA node - 70-80 BPM in adult |
|
|
What is an ectopic focus? |
Heart beat begins somewhere other than SA node - region of spontaneous firing (hypoxia, caffeine, nicotine, electrolyte imbalance) - nodal rhythm set by AV node - intrinsic ventricular rhythm |
|
|
What is an arrhythmia? |
Any abnormal cardiac rhythm (heart block: failure of conduction due to disease) |
|
|
What is tachycardia? |
- persistent resting heart rate above 100 - Candy due to stress, anxiety, drugs, heart disease, or rise in body temperature |
|
|
What is bradycardia? |
- A persistent, resting adult heart rate of below 60 - common in sleep and endurance trained athletes |
|
|
What three measurements does an EKG (electrocardiogram) read? |
1. P wave - impulse from SA node to atrium, signal to depolarize atrial muscle (signal to contract) 2. QRS wave - transmission through Purkinje fibers to ventricle, signal to depolarize ventricular muscle 3. T wave - recovery phase, repolarization of ventricular muscle |
|
|
Where is blood moving in the PQ segment of an EKG? |
From the atrium to the ventricle |
|
|
What are purkinje fibers? |
Bundle of His to myocardium - spread electrical signal to ventricles |
|
|
Where is the blood moving in the ST segment of an EKG? |
From the ventricles to out of the heart |
|
|
What is the resting potential of cardiac muscle? |
-90mV |
|
|
What is the action potential threshold of cardiac muscle,and what are the three phases of a cardiac muscle action potential? |
- -70mV - rising phase (NA+ channels, transient CA++ channels) - plateau phase ( long lasting Ca++ channels and decrease K+ permeability) - falling phase ( open K+ channels, close Ca++ channels) |
|
|
End-diastolic volume (EDV) |
Amount of blood in the ventricle before contraction |
|
|
What is tachycardia? |
- persistent resting heart rate above 100 - Can be due to stress, anxiety, drugs, heart disease, or rise in body temperature |
|
|
Stroke volume (SV) |
Amount pumped by each ventricle per beat (EDV-ESV=SV) |
|
|
Ejection fraction |
SV/EDV - at rest ~54%, during exercise as high as 90%, diseased heart <50% |
|
|
What are the two types of extracellular fluid? |
1. Interstitial between cells 2. intravascular in blood and lymph vessels |
|
|
What two opposing forces make up the flow at capillaries? |
1. Filtration - primarily at beginning - fluid movement out of capillary - cell and protein-free filtrate enters the interstitial fluid 2. Reabsorption - primarily at end - fluid movement into capillary - from the interstitial fluid into the blood |
|
|
What is the formula for bulk flow? |
Bulk flow = filtration + reabsorption |
|
|
What are the 2 keys to efficient cardiac pumping? |
1. Coordinated contraction - both atria or both ventricles contract at once, fast spreading signal on conduction pathways, plus gap junctions 2. Top and bottom pumping - atria contract, then delay, then ventricles contract, ensures filling of ventricles and prevents backflow |
|
|
What is the role of bulk flow? |
1. Regulating distribution of ECF 2. Between plasma and interstitial fluid-particularly blood pressure/volume compensations |
|
|
What are not some of the rolls of bulk flow? |
1. Exchange of solutes-that happens mostly by passive diffusion - all solvents are moved with the water but in both directions |
|
|
What are the forces that contribute to filtration? |
1. Capillary blood pressure 2. Tissue colloidal osmotic pressure |
|
|
What are the forces that contribute to reabsorption in bulk flow? |
1. Blood colloidal osmotic pressure 2. Interstitial pressure |
|
|
What is capillary blood pressure (blood hydrostatic pressure)? |
- blood (hydrostatic) pressure inside capillaries pushing out - high on atrial end (37 mm Hg), low on venous end (17 mm Hg) - same force that drives blood flow through vessels - primary cause of filtration |
|
|
What is interstitial hydrostatic pressure (tissue hydrostatic pressure)? |
- constant along length of capillaries - pressure between tissue cells, outside of capillary - usually negligible but can be a cause of reabsorption |
|
|
What is colloidal osmotic pressure? |
1. Caused by colloidal dispersion of proteins in interstitial fluid 2. Increased concentration of proteins - decreased concentration of water - increased osmolarity of fluid 3. Drives osmosis, diffusion of water |
|
|
What is blood (plasma) colloidal osmotic pressure? |
- constant along length of capillary - proteins inside vessel = attract water into blood - primary cause of reabsorption |
|
|
What is tissue (interstitial fluid) colloidal osmotic pressure? |
- normally not very many proteins in interstitial fluid - proteins outside vessel = the attracts water into tissues - it is a weak cause of filtration - constant along length of capillary |
|
|
What are the 6 causes/influences of venous return? |
1. Pressure gradient 2. Skeletal muscle contractions 3. Venous valves 4. Cardiac suction 5. Sympathetically driven vasoconstriction 6. Thoracic pump |
|
|
What are the the 7 electrical links that ensure efficient pumping? |
1. Inter atrial pathway 2. Internodal pathway 3. AV nodal delay 4. Gap junctions 5. Fibrous skeleton 6. Bundle of His 7. Purkinje Fibers |
|
|
What thre factors control/cause blood pressure? |
1. Cardiac output 2. Blood volume 3. Peripheral resistance |
|
|
What is systolic pressure? |
BP during ventricular systole (contraction) |
|
|
What is diastolic pressure? |
BP during ventricular diastole (not contracted) |
|
|
What is a normal, young adult, BP? |
120(systolic)/75(diastolic) mm Hg |
|
|
How do you measure pulse pressure? |
Pulse pressure = systolic - diastolic - important measure of stress exerted on small arteries |
|
|
What is mean arterial pressure (MAP)? |
Measurements taken at intervals of cardiac cycle, best estimate: diastolic pressure + ( 1/3 of pulse pressure) - varies with gravity |
|
|
What three factors control/cause blood pressure? |
1. Cardiac output 2. Blood volume 3. Peripheral resistance |
|
|
What is perfusion? |
Rate of blood flow per given mass of tissue (ml/min/g) |
|
|
What are the three kinds of peripheral resistance? |
1. Blood viscosity 2. Vessel length 3. Vessel radius |
|
|
Describe the interatrial pathway. |
- SA node to left atrium - fast - ensures simultaneous contraction of atria |
|
|
Describe the internodal pathway. |
- only electrical link between atria (SA node) and ventricles |
|
|
Describe the AV nodal delay. |
- about 100 ms - allows atria to contract before ventricles |
|
|
How do gap junctions ensure efficient pumping? |
- electrical links between adjacent cardiac muscle cells ensure simultaneous contraction |
|
|
What is the fibrous skeleton? |
- separates atria and ventricles - electrically insulates atria from ventricles |
|
|
How does the bundle of His ensure efficient pumping? |
- two branches split fro AV node and 1 goes to each ventricle |
|
|
If systemic peripheral resistance increases, what effect might this have on the rest of the cardiovascular system over the long term? |
1. Increased afterload 2. Pulmonary edema 3. Hyper trophy of myocardium especially in the left ventricle |
|
|
What factors can regulate blood pressure in the short term? |
1. Baroreflex - cardiac output 2. Chemoreflex-cardiac output 3. Vasodilation/vasoconstriction-hormones in sympathetic nervous system |
|
|
What factors can regulate blood pressure in the short term? |
1. Baroreflex - cardiac output 2. Chemoreflex-cardiac output 3. Vasodilation/vasoconstriction-hormones in sympathetic nervous system |
|
|
What factors regulate blood pressure in the long term? |
1. Hormones 2. Blood volume-salt and water balance in the kidneys and liver |
|
|
What are barrow receptors? |
1. Pressure sensor in aortic arch and carotid sinus - stretch receptors - measure mean arterial blood pressure and pulse pressures by measuring the distention of artery wall 2. Fire more action potentials to increase blood pressure 3. Signal cardiovascular control center in Medela |
|
|
What are barrow receptors? |
1. Pressure sensor in aortic arch and carotid sinus - stretch receptors - measure mean arterial blood pressure and pulse pressures by measuring the distention of artery wall 2. Fire more action potentials to increase blood pressure 3. Signal cardiovascular control center in Medula |
|
|
What do you baroreceptors do if blood pressure is too high? |
1. Decrease heart rate, decrease stroke volume, parasympathetic nervous system 2. Systemic vasodilation, Lower peripheral resistance |
|
|
What do baroreceptors do if blood pressure is too low? |
1. Increased heart rate, increased stroke volume 2. Systemic vasoconstriction, sympathetic nervous system, increase peripheral resistance |
|
|
Where are chemoreceptors located? |
Chemoreceptors in aortic bodies in carotid bodies, located in aortic arch, subclavian arteries, and external carotid arteries. |
|
|
Where are chemoreceptors located? |
Chemoreceptors in aortic bodies in carotid bodies, located in aortic arch, subclavian arteries, and external carotid arteries. |
|
|
What do chemoreceptors do? |
They regulate the autonomic response to changes in blood chemistry. 1. pH, O2, CO2 2. primary role: adjust respiration 3. Secondary role: vasomotion/blood pressure - hypoxemia, hypercapnia and acidosis stimulate chemo receptors, instruct that's a motor center to cause vasoconstriction, increased blood pressure, increased long perfusion and gas exchange |
|
|
What is the medullary ischemic reflex? |
When there is inadequate perfusion of the brainstem, this reflex tries to keep blood flowing to the brain-cardiac in Vassar motor centers send sympathetic signals to heart and blood vessels, this increases cardiac output and causes widespread vasoconstriction, it also increases blood pressure |
|
|
Which hormones regulate blood pressure? |
1. Angiotensin two 2. Epinephrine/norepinephrine 3. Aldosterone 4. Atrial naturietic peptide 5. Anti diuretic hormone (ADH) |
|
|
How is angiotensin II created? |
Angiotensinogen is a plasma proteins and prohormone that is produced by the liver. It is activated by renin, an enzyme in the kidney that is released in response to low blood pressure, and becomes angiotensin one. ACE, or Angiotensin converting enzyme, which is located in the Lungsconverts angiotensin one into angiotensin II. |
|
|
How is angiotensin II created? |
Angiotensinogen is a plasma protein and prohormone that is produced by the liver. It is activated by renin, an enzyme in the kidney that is released in response to low blood pressure, and becomes angiotensin one. ACE, or Angiotensin converting enzyme, which is located in the Lungs converts angiotensin one into angiotensin II. |
|
|
What does angiotensin II do? |
It is a very potent vasoconstrictor that increases blood pressure and aldosterone |
|
|
what effect do ACE inhibitors have on blood pressure? |
- lowers blood pressure - ACE inhibitors block the conversion of angiotensin I to angiotensin II - prevents peripheral vasoconstriction and keeps peripheral resistance low |
|
|
what effect do ACE inhibitors have on blood pressure? |
- lowers blood pressure - ACE inhibitors block the conversion of angiotensin I to angiotensin II - prevents peripheral vasoconstriction and keeps peripheral resistance low |
|
|
What effect does epinephrine and norepinephrine have on blood pressure? |
- most blood vessels, binds to Alpha-adrenergic receptors, causes vasoconstriction, increases blood pressure - skeletal and cardiac muscle blood vessels, bonds to beta-adrenergic receptors, causes vasodilation |
|
|
What effect does anti diuretic hormone (ADH, vasopressin) have on blood pressure? |
Pathologically high concentrations, vasoconstriction, causes a long term blood volume change |
|
|
What affect does aldosterone have on blood pressure? |
- Water follows sodium ions - promotes retention ofsodium in water by the kidneys - increases blood volume and pressure, blood pressure rises - causes long term blood volume change |
|
|
What effect does atrial natriuretic factor have on blood pressure? |
- increase urinary sodium excretion (losesodium ions, lose water) - released by heart response to heart stretch - causes generalized vasodilation, decreases blood pressure - causes long term blood volume change |
|
|
While epinephrine causes most blood vessels to constrict, it causes cardiac blood vessels to dilate. What effect does the generalized vasoconstriction have? |
Increases blood pressure |
|
|
While epinephrine causes most blood vessels to constrict, it causes cardiac vessels to dilate. what effect does cardiac vasodilation have? |
Increases blood flow to the heart, using more nutrients to overcome the higher blood pressure and keep up with the increased heart rate |
|
|
What is hypertension? |
- chronic resting blood pressure greater than 140/90 - blood-pressure rises with H-arteries less distensible - can we can small arteries and cause aneurysms, folding weak spots in vessels, threaten hemorrhage |
|
|
What is hypertension? |
- chronic resting blood pressure greater than 140/90 - blood-pressure rises with H-arteries less distensible - can we can small arteries and cause aneurysms, folding weak spots in vessels, threaten hemorrhage |
|
|
What is hypotension? |
- chronic low resting blood pressure - caused by-blood loss, dehydration, anemia |
|
|
What is hypertension? |
- chronic resting blood pressure greater than 140/90 - blood-pressure rises with H-arteries less distensible - can weaken small arteries and cause aneurysms, folding weak spots in vessels, threaten hemorrhage |
|
|
What is hypotension? |
- chronic low resting blood pressure - caused by-blood loss, dehydration, anemia |
|
|
What are the three kinds of circulatory shock? |
1. Cardiogenic shock - in adequate pumping of heart, myocardial infarction 2. Neurogenic shock - loss of that so Millertown, vasodilation - caused by emotional shock or brainstem injury 3. Low venous return Schock - hypovolemic shock - most common cause of shock, loss of blood volume - obstructed venous return Schock-tumor or any reason - venous pooling, vascular, Schock-long periods of standing, sitting, or widespread vasodilation |
|
|
What are two common causes of hypovolemic shock? (Blood in tissue, not in vessels) |
1. Septic shock - bacterial toxins trigger vasodilation - increased capillary permeability 2. Anaphylactic shock - severe immune reaction to antigen, histamine release, generalized vasodilation - increased capillary permeability |
|
|
What are two common causes of hypovolemic shock? (Blood in tissue, not in vessels) |
1. Septic shock - bacterial toxins trigger vasodilation - increased capillary permeability 2. Anaphylactic shock - severe immune reaction to antigen, histamine release, generalized vasodilation - increased capillary permeability |
|
|
What is compensated shock? |
Homeostatic mechanisms correct for the problem - lowered blood-pressure triggers barrow reflex and production of angiotensin II, both stimulate vasoconstriction - if person faints, syncope, and falls to a horizontal position gravity restores the blood flow to the brain quicker if the feet are raised |
|
|
What is decompensated shock? |
when the body's response is not adequate to compensate for the shock - life-threatening positive feedback loop occurs |
|
|
What do you think vessels do? |
They are a vascular system separate from the blood system, they absorb and filter interstitial fluid |
|
|
What do lymph vessels do? |
They are a vascular system separate from the blood system, they absorb and filter interstitial fluid |
|
|
What is the lymph? |
Fluid inside lymph vessels, it is similar to blood plasma |
|
|
What are the four functions of the lymphatic system? |
1. Return of excess filtered fluid to the body, fluid that has been filtered but not rehab sort during book flow - it returns 2 to 3 L per day through the subclavian veins 2. Returns plasma proteins to blood, prevents edema 3. Immune defense, lymph nodes defend against antigens and help signal immune attack 4. Transport digested/absorb that from small intestine |
|
|
describe lymph flow back to the circulatory system. |
1. Rhythmic contraction of smooth muscle around lymph vessels, lymph pump 2. Squeezing of lymph vessel by skeletal muscle, vessels have one-way valves, identical to venous system |
|
|
What is the purpose of multiple lymph nodes in the lymph system? |
- lymph passes through several lymph nodes before returning to blood - more cleaning - more opportunities to destroy pathogens - protects central areas from peripheral infections |
|
|
What is contained in lymph follicles? |
- mostly B cells - some macrophages |
|
|
What is contained in lymph follicles? |
- mostly B cells - some macrophages |
|
|
What is contained in the germinal center of a lymph node? |
- activated B cells - memory B cells - plasma cells |
|
|
What is contained in lymph follicles? |
- mostly B cells - some macrophages |
|
|
What is contained in the germinal center of a lymph node? |
- activated B cells - memory B cells - plasma cells |
|
|
What is contained in the inner cortex of lymph nodes? |
T cells |
|
|
What is contained in lymph follicles? |
- mostly B cells - some macrophages |
|
|
What is contained in the germinal center of a lymph node? |
- activated B cells - memory B cells - plasma cells |
|
|
What is contained in the inner cortex of lymph nodes? |
T cells |
|
|
What is contained in the medulla of length nodes? |
- plasma cells - activated B cells - plasma cells that make immunoglobulins, 2000 per second for several days in a row |
|
|
What are four causes of Adema? |
1. Blocked/removed lymph vessels-elephantitis 2. If you were plasma proteins in the blood-lowers plasma colloidal pressure and caused by liver disease in malnutrition 3. Increased capillary permeability Thomas more histamine, allergies, blisters 4. Increased arterial or venous pressure, hypertension, poor venous return, embolism, increases capillary blood pressure |
|
|
What are four causes of Adema? |
1. Blocked/removed lymph vessels-elephantitis 2. If you were plasma proteins in the blood-lowers plasma colloidal pressure and caused by liver disease in malnutrition 3. Increased capillary permeability Thomas more histamine, allergies, blisters 4. Increased arterial or venous pressure, hypertension, poor venous return, embolism, increases capillary blood pressure |
|
|
What are five consequences of edema? |
1. Circulatory shock 2. Tissue necrosis 3. Pulmonary edema 4. Cerebral edema 5. Ascites |
|
|
What is ascites? |
Increased peritoneal fluid, potbelly, can be caused by lack of plasma |
|
|
What are the 3 components of intercalated discs? |
1. Interdigitating folds - increase SA 2. Desmosomes - mechanical junctions 3. Gap junctions - for coordinated contractions |
|
|
What is the role of Ca++ in cardiac muscle? |
1. Action potentials allow Ca++ entry from ECF - via L-type Ca++ channels in T-tubules 2. Ca++ binds to troponin - pulls tropomyosin to expose binding sites |
|
|
Describe the cardiac muscle refractory period? |
It has a long absolute refractory period, almost as long as the contraction. There is no summation and tetanus. It is due to NA+ voltage gated channels |
|
|
Describe the cardiac muscle refractory period? |
It has a long absolute refractory period, almost as long as the contraction. There is no summation and tetanus. It is due to NA+ voltage gated channels |
|
|
What is the result of cardiac muscles long absolute refractory period? |
1. Strong contraction 2. Full relaxation |
|
|
Describe the cardiac muscle refractory period? |
It has a long absolute refractory period, almost as long as the contraction. There is no summation and tetanus. It is due to NA+ voltage gated channels |
|
|
What is the result of cardiac muscles long absolute refractory period? |
1. Strong contraction 2. Full relaxation |
|
|
What is systole? |
Contraction of chamber |
|
|
Describe the cardiac muscle refractory period? |
It has a long absolute refractory period, almost as long as the contraction. There is no summation and tetanus. It is due to NA+ voltage gated channels |
|
|
What is the result of cardiac muscles long absolute refractory period? |
1. Strong contraction 2. Full relaxation |
|
|
What is systole? |
Contraction of chamber |
|
|
What is diastole? |
Relaxation of chamber |
|
|
Describe the quiescent period (diastasis) of the cardiac cycle. |
1. All chambers relaxed 2. AV valves open 3. Semilunar valves closed 4. Blood moving into ventricles 5. EKG phase - P |
|
|
Describe the atrial systole phase of the cardiac cycle? |
1. SA node fires 2. AV valves are open 3. Semi lunar valves are closed 4. Atria depolarize and contract, this forces additional blood into the ventricles (atrial kick) 5. Ventricles now contain end diastolic volume of about 130 mL of blood 6. EKG phase-PQ |
|
|
Describe the ventricular isovolumetric contraction phase of the cardiac cycle. |
1. Atria repolarize and relax (blood flows into atria) 2. EKG phase-QRS 3. AV valves are closing at the beginning and closed for the majority of this phase (rising pressure closes the AV valves) 4. Semi lunar valves are closed, and open at the end of the phase 5. Ventricles depolarize in contract 6. no ejection of blood yet, no change in volume (pressure in ventricles not yet higher than in a order/pulmonary arteries) 7. Heart sound-S1 |
|
|
Describe the ventricular ejection phase of the cardiac cycle. |
1. Ventricles continue to contract 2. Rising pressure becomes higher than the pressure in the aorta/pulmonary trunk causing the semi lunar valves to open 3. Rapid ejection of blood into occurs and the pressure falls 4. AV valves are closed 5. EKG phase-ST 6. Atria are relaxed |
|
|
Describe the ventricular isovolumetric relaxation phase of the cardiac cycle. |
1. Ventricles repolarize and relax, begin to expand 2. EKG phase-T 3. Semi lunar valves close, aortic pressure curve shows dicrotic notch-back pressure pushes blood into coronary arteries 4. Heart sound S2 occurs 5. AV valves are closed 6. Atria is relaxed |
|
|
Describe the ventricular filling phase of the cardiac cycle. |
1. AV valve opens and rapid ventricular filling caused by ventricular relaxation - fills because of low pressure 2. Semilunar valves are closed 3. Blood moves into atria and ventricles 4. Atria and ventricles are relaxed |
|

Which column represents atrial "kick"? |
B |
|
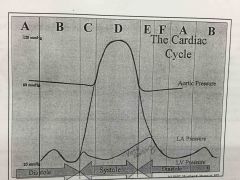
Which column represents isovolumetric ventricular relaxation? |
E |
|

In which column is the dicrotic notch take place? |
E |
|

In which column does ventricular ejection occur? |
D |
|

In which column does isovolumetric ventricular contraction occur? |
C |
|
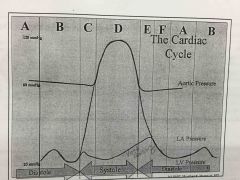
In which column does isovolumetric ventricular contraction occur? |
C |
|
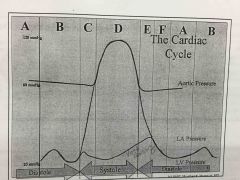
In which column does diastasis occur? |
A |
|
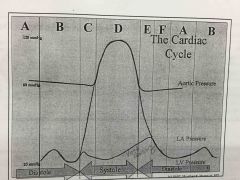
In which column does rapid filling of the ventricles occur? |
F |
|

In which column does the tricuspid valve open? |
E and F |
|
|
Describe stroke volume. |
Amount of blood pumped by each ventricle per beat (EDV - ESV) about 70 mL |
|
|
Describe stroke volume. |
Amount of blood pumped by each ventricle per beat (EDV - ESV) about 70 mL |
|
|
What is the Frank-Starling law of the heart? |
Heart pumps all blood returned to it. - venous return increase = stroke volume increase - increased stretch of cardiac muscle = increased contraction strength |
|
|
What is pulmonary edema? |
1. Right ventricular output exceeds left ventricular output 2. Pressure backs up 3. Fluid accumulates in pulmonary tissue |
|
|
What is pulmonary edema? |
1. Right ventricular output exceeds left ventricular output 2. Pressure backs up 3. Fluid accumulates in pulmonary tissue |
|
|
What is systemic edema? |
1. Left ventricular output exceeds right ventricular output 2. Pressure backs up 3. Fluid accumulates in systemic tissue |
|
|
Define cardiac output. |
- volume of blood pumped by each ventricle per minute - heart rate x volume per stroke |
|
|
What is preload? |
- amount of tension in ventricular myocardium before it contracts - increased preload causes increased contraction strength = increased SV |
|
|
What is afterload? |
- pressure in arteries above semilunar valves opposes opening of valves - increased afterload = decreased SV |
|
|
Why does an increase in afterload cause a decrease in stroke volume? |
- more energy is used to overcome resistance - less energy is used to move blood |
|
|
What are some causes or diseases that could increase afterload? |
- increased blood viscosity (polycythemia, leukemia, dehydration) - stenosis - increased vessel length |
|
|
What is contractility? |
- contraction force for a given preload - tension caused by factors that adjust myocyte's responsiveness to stimulation - increased contractility are positive inotropic agents |
|
|
How do chronotropic agents effect heart rate? |
Positive chronotropic agents increase HR Negative chronotropic agents decrease HR |
|
|
What region of the brain regulates chronotropic effects? |
- cardiac center of Medula oblongata - sympathetic by cardioacceleratory center - parasympathetic by cardio inhibitory center |
|
|
What is myocardial infarction? |
Sudden death of heart tissue caused by interruption of blood flow from vessel narrowing or occlusion |
|
|
What is an anastomoses and what is its function? |
It is an alternate blood pathway that defends against blood flow interruption |
|
|
What is an arteriovenous shunt? |
- a type of anastomoses - capillary bypass - artery flows directly into vein |
|
|
What is a venous anastomosis? |
- most common, blockage less serious - alternate drainage of organs |
|
|
What are arterial anastomosis? |
- at critical organs - collateral circulation (coronary) |
|
|
What is vasa vasorum? |
Walls of large vessels require their own blood supply Blood supply for large blood vessel |
|
|
What are arterioles? |
Control amount of blood to various organs with smooth muscle Controls where blood goes/doesn't go |
|
|
What are prevail lady sphincters? |
- control which vascular beds are well perfused - controls if blood goes to capillaries - only .25 of the capillaries are open at a given time |
|
|
What are the three types of capillaries? |
1. Continuous 2. Fenestrated 3. Sinusoids |
|
|
Describe continuous capillaries. |
- in most tissues - endothelial cells have tight junctions with intercellular clefts - allow passage of solutes, restricts passage of blood cells and large proteins |
|
|
Describe Fenestrated capillaries. |
- in kidneys and small intestines - organs that require rapid absorption or filtration - endothelial cells have filtration pores that allow passage of small molecules |
|
|
Describe sinusoid capillaries. |
- in liver, bone marrow, spleen - irregular blood filled spaces; some have extra large fenestrations that allow proteins and blood cells to enter blood stream |
|
|
What are the 3 routes across endothelial cells? |
1. Intercellular clefts 2. Fenestrations 3. Through the cell |
|
|
What are the 3 mechanisms of capillary exchange? |
1. Diffusion 2. Transcytosis 3. Bulk flow |
|
|
Describe how different kinds of molecules diffuse. |
- lipid permeable diffuse through the wall - lipid insoluble pass through intercellular clefts or fenestrations - large particles held back in blood |
|
|
Describe transcytosis. |
Pinocytosis (cell drinking) transport vesicles across cell via exocytosis |

