![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back

Which part is the "expiratory" part and which is the "inspiratory" part of the curve?
|
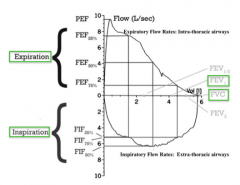
- Expiration: top of curve
- Inspiration: bottom of curve |
|
|
What are the possible patterns for the expiratory phase?
|
- Obstructive: steep slope with bunny hill at the end
- Normal - Restrictive: fast expiration but total amount is reduced |
|

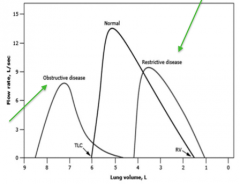
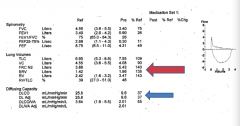
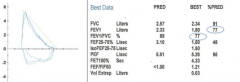
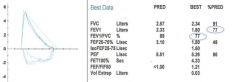
What does this spirometry represent?
|
Obstructive Disease
|
|
|
What does the FVC tell you?
|
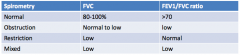
Forced Vital Capacity:
- Normal: 80-100% of expected - Obstruction: normal to low - Restriction: low - Mixed: low |
|
|
What does the FEV1/FVC ratio tell you?
|
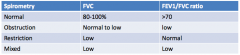
Forced Expiratory Volume in 1 second / Forced Vital Capacity:
- Normal: >70 - Obstruction: low - Restriction: normal - Mixed: low |
|
|
Which of the following would not usually cause an obstructive pattern on spirometry?
a) Moderate persistent asthma b) Tracheomalacia c) Kyphoscolosis d) COPD e) Cystic Fibrosis |
Kyphoscolosis (restrictive physiology - causes spine to crowd lungs making them shrunken)
- Tracheomalacia: softening of cartilage, makes it collapse, if they can blow out slowly they can have a normal curve but when doing it fast it is limited - Cystic Fibrosis: (infection leads to bronchiectasis, leads to floppy airways making an obstruction) |
|
|
What is a normal FVC and FEV1/FVC ratio?
|
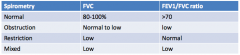
- FVC: 80-100% of expected
- FEV1/FVC: >70 |
|
|
What is the FVC and FEV1/FVC ratio in obstructive disease?
|
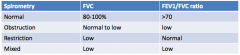
- FVC: normal to low
- FEV1/FVC: low |
|
|
What is the FVC and FEV1/FVC ratio in restrictive disease?
|
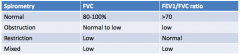
- FVC: low
- FEV1/FVC: normal |
|
|
What is the FVC and FEV1/FVC ratio in mixed disease?
|
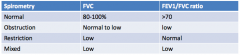
- FVC: low
- FEV1/FVC: low |
|
|
What pathology causes obstruction in the large conducting airways?
|
- Tumors
- Foreign bodies |
|
|
What pathology causes obstruction in the peripheral airways?
|
- Asthma
- Chronic Bronchitis - Cystic Fibrosis |
|
|
What pathology causes obstructive disease via pulmonary parenchymal disease?
|
Emphysematous changes from cigarette smoking
|
|

What does this spirometry represent?
|

Restrictive Ventilatory Defect
|
|
|
What can cause restrictive ventilatory defect?
|
- Interstitial lung disease: sarcoidosis, collagen vascular disease, pulmonary fibrosis
- Pneumonectomy - Pleural disease: pleural effusion - Chest wall disease: kyphosis, neuromuscular disorders - Extra-thoracic conditions: obesity |
|
|
What are the interstitial lung diseases? What expiratory pattern do they cause?
|
- Sarcoidosis
- Collagen vascular disease - Pulmonar fibrosis - Causes restrictive lung disease |
|
|
What kind of disease is caused by decreased compliance of the lungs/chest wall?
|
Restrictive Disease
|
|
|
What is compliance?
|
Combination of lung compliance and chest wall compliance
|
|
|
What is the amount of air that is inspired and expired in a normal breath?
|
Tidal Volume
|
|
|
What is the extra amount of volume you can inspire ABOVE a normal inspiration?
|
Inspiratory Reserve Volume
|
|
|
What is the extra amount of volume you can expire ABOVE a normal expiration?
|
Expiratory Reserve Volume
|
|
|
What is the amount of volume in the lungs you CAN'T expire?
|
Residual Volume (RV)
|
|
|
What is the total amount of air in the lungs after a normal breath?
|
Functional Residual Capacity
|
|
|
What is the total volume of air that can be exhaled from a maximum inhalation?
|
Vital Capacity
|
|
|
What is the total amount of air that is stored in the lungs after a maximum inhalation?
|
Total Lung Capacity
|
|
|
What is the definition of Functional Residual Capacity (FRC)?
a)The amount of volume left in the lungs at the end of forced exhalation? b) The amount of volume breathe out from a maximal inspiration effort c) The amount of volume left in the lungs at the end exhalation from tidal breathing d) The amount of volume that can be exhaled at the end of exhalation from tidal breathing e) The amount of volume moved out of the lungs during quiet breathing |
The amount of volume left in the lungs at the end exhalation from tidal breathing
|
|
|
What are the key determinants of the diffusion of gases in the lung?
|
- Surface area of lung with contact to diffusing alveoli
- Thickness of alveolar capillary membrane - Volume of blood available in capillary bed of lung |
|
|
Which of the following is not associated with a low diffusing capacity?
a) Asthma b) COPD c) ILD d) Pulmonary Hypertension e) Sarcoidosis |
**Asthma
Pulmonary HTN - will affect blood flow through capillary bed, you would see a compromised diffusing capacity COPD - chronic obstructive PFTs d/t asthma |
|
|
What are some causes of a low diffusing capacity?
|
- Anemia
- Emphysema (loss of parenchyma) - Pulmonary Fibrosis (scarring) - Pulmonary Edema due to heart failure or in response to allergens (acute interstitial pneumonitis) - Pulmonary vasculitis - Pulmonary hypertension |
|
|
What diseases have an INCREASED diffusing capacity?
|
- Asthma
- Alveolar hemorrhage (acute) - Intracardiac shunt (L→R) - Erythrocytosis |
|
|
What are the types of Chronic Obstructive Pulmonary Disease (COPD)?
|
- Emphysema
- Chronic Bronchitis - Bronchiectasis - Chronic persistent Asthma (FEV1 remains abnormal after therapy) |
|
|
What causes emphysema?
|
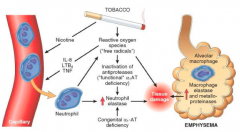
- Irritants activate macrophages and epithelial cells to release chemotactic factors
- Leads to recruitment to the area with more macrophages and neutrophils - Proteases are released that destroy structural elements in lungs - Reactive O2 species contribute to destructive power of proteases leading to breakdown of alveolar units |
|
|
What are the patterns of emphysema?
|
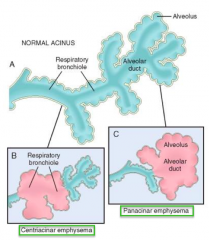
- Centriacinar emphysema (initially affects respiratory bronchioles)
- Panacinar emphysema (initial distention of alveolus and alveolar duct - Paraseptal |
|
|
What causes centriacinar emphysema?
|
Smoking
- Proximal part of acinus, respiratory bronchiole, +/- alveolus - Upper lobes of smokers may also see chronic bronchitis and bronchiolitis |
|
|
What causes panacinar emphysema?
|
α1-Antitrypsin (AT) deficiency
- Destruction involving the entire units (respiratory bronchiole - alveoli) - Associated with hepatitis and cirrhosis |
|
|
What causes paraseptal emphysema?
|
Distal destruction / enlargement of alveoli
- Upper lobe, subpleural location - Predisposes to spontaneous pneumothorax - Patchy distribution of parenchymal injury and +/- pulmonary scarring |
|
|
What happens to the airways in emphysema?
|
- Loss of elastic recoil
- Dynamic airway collapse due to loss of structural supports in smaller non-cartilaginous airways - As lungs expand they stretch chest wall and place diaphragm at mechanical disadvantage and upper chest wall muscles must now assist in breathing |
|
|
What happens to the ventilation/perfusion and deadspace in emphysema? Outcome?
|
- As more alveoli are lost, more mismatched ventilation perfusion and deadspace develop
- Eventually leads to hypoxemia as well as hypercapnia |
|
|
How do you calculate the volume of dead space?
|
Vds / Vt = (PaCO2 - P mixed expired CO2) / (PaCO2)
- Vds = Dead Space Volume in alveoli (not including windpipe) - Vt = Tidal Volume - PaCO2 = Arterial CO2 Pressure - P mixed expired CO2 = end-expired CO2 |
|
|
What is the dead space volume for a patient with a tidal volume of 500 mL, an arterial CO2 of 42 mmHg, and end-expired CO2 of 40 mmHg (measured using capnography?
|
Vds / Vt = (PaCO2 - P mixed expired CO2) / (PaCO2)
Vds / 500 mL = (42 mmHg - 40 mmHg) / (42 mmHg) = (2 mmHg)* 500 mL / 42 mmHg = 24 mL |
|
|
What is the genetic cause of emphysema? How is it inherited?
|
α-1 Antitrypsin Deficiency
- Autosomal recessive |
|
|
What is the genotype associated with Panacinar Emphysema?
a) MM b) MZ c) MS d) ZZ e) CFTR nonsense Mutation |
ZZ
|
|
|
What is the normal phenotype for α1-antitrypsin? Abnormal?
|
- Normal: MM
- Panacinar Emphysema: ZZ - Heterozygous MZ is also at risk, especially with smoking because only 1/2 the amount of α1AT |
|
|
Who should be screened for autosomal recessive α1-Antitrypsin Deficiency?
|
Patients with obstructive lung disease
|
|
|
How should you treat patients with α1-Antitrypsin Deficiency?
|
Replacement therapy of α1AT can stabilize function if no longer smoking
|
|
|
What causes Chronic Bronchitis?
|
- Inhaled smoke or other respiratory irritants or abnormal mucus d/t or resulting in recurrent bacterial infection
- Leads to mucus hypersecretion in bronchi → airflow obstruction in terminal bronchioles (more proximal than in emphysema) → irreversible fibrosis of terminal bronchioles |
|
|
Which part of the lung is affected by irreversible fibrosis in chronic bronchitis?
|
Terminal Bronchioles
|
|
|
What are the criteria for diagnosing Chronic Bronchitis?
|
Productive cough for at least 3 months for 2 consecutive years
|
|
|
What can cause Chronic Bronchitis?
|
- Smoking
- Chronic exposure to respiratory irritants (pollution, work related) - Cystic Fibrosis - Infection |
|
|
What are the clinical findings in patients with Chronic Bronchitis?
|
- Productive cough
- Cyanosis (d/t decreased O2 saturation from hypoxemia) - Blue bloaters - Dyspnea - Expiratory wheezing and rhonchi (d/t lots of phlegm) - Cor pulmonale (R heart failure) - Clubbing |
|
|
What are the findings on chest x-ray in a patient with Chronic Bronchitis?
|
- Enlarged heart
- Horizontally oriented heart - Increased bronchial markings |
|
|
What are the histologic findings in a patient with Chronic Bronchitis?
|
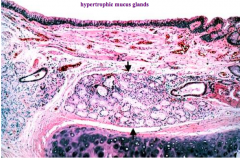
Increased mucus glands (hypertrophy)
|
|
|
What is the term/scale used to describe the microscopic changes in chronic bronchitis?
|
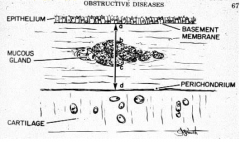
Reid Index:
- Ratio of the thickness of the mucus gland layer to the thickness of the wall between the epithelium and cartilage (normal <0.4) |
|
|
What is the term/scale used to determine the prognosis for patients with COPD?
|
BODE Index:
- BMI: lower associated with worse outcome - Obstruction of airflow: FEV1 - Dyspnea: graded based on another scale (MMRC) - Exercise capacity: 6 min walk test |
|
|
What is the B in "BODE Index"? Implications?
|
BMI: lower BMI associated with worse outcomes in COPD
|
|
|
What is the O in "BODE Index"? Implications?
|
Obstruction of airflow (FEV1); involved in determining prognosis of COPD
|
|
|
What is the D in "BODE Index"? Implications?
|
Dyspnea: graded on another scale (MMRC); involved in determining prognosis of COPD
|
|
|
What is the E in "BODE Index"? Implications?
|
Exercise capacity: 6 minute walk test; involved in determining prognosis of COPD
|
|
|
How do you treat patients with COPD?
|
- Bronchodilators
- Anticholinergics - Inhaled corticosteroids - O2 therapy |
|
|
What is the effect of bronchodilators for patients with COPD?
|
Relaxes smooth muscle bronchoconstriction, increases cilia beat frequency
|
|
|
What is the effect of anticholinergics for patients with COPD?
|
Blocks muscarinic receptors, prevents bronchoconstriction, decreases mucus production
|
|
|
What is the effect of inhaled corticosteroids for patients with COPD?
|
May decrease exacerbations
|
|
|
What is the effect of O2 therapy for patients with COPD?
|
May decrease mortality in cor pulmonale
|
|
|
Case 1:
- 67 yo Caucasian man presents in clinic with complain of dyspnea and cough What are some general causes of dyspnea in this age group? |
- COPD
- Cardiac - Anemia - Deconditioning (out of shape) |
|
|
What should you think of if your patient with chest pain also complains of it radiating to the neck or arm, with diaphoresis, or with nausea? Mechanism?
|
Angina - myocardial ischemia with exercise leads to decreased diastolic relaxation or systolic dysfunction and acute pulmonary edema
|
|
|
What should you think of if your patient with chest pain also complains of chronic cough and has a history of tobacco use?
|
COPD
|
|
|
What should you think of if your patient with chest pain also complains of orthopnea, paroxysmal nocturnal dyspnea, and leg swelling? Mechanism?
|
Congestive Heart Failure - increased pulmonary venous pressures leads to decreased compliance of lungs and alveolar flooding due to capillary leak
|
|
|
Case 1:
- 67 yo Caucasian man presents in clinic with complain of dyspnea and cough - Progressive dyspnea - Cough productive sputum - Leg edema - Wheezing and nighttime breathing problems - Significant smoking history - Some hobby and occupational exposures (limited) to respiratory irritants What is the differential at this point? |
COPD:
- Chronic bronchitis - Emphysema - Asthma - Bronchiectasis |
|
|
Case 1:
- 67 yo Caucasian man presents in clinic with complain of dyspnea and cough - Progressive dyspnea - Cough productive sputum - Leg edema - Wheezing and nighttime breathing problems - Significant smoking history - Some hobby and occupational exposures (limited) to respiratory irritants Exam: - Speaking in short sentences (mild respiratory distress) - Tachycardia, low SpO2 - JVD, trace edema, cyanosis, barrel chested, hyper-resonance, decreased breath sounds, scattered wheezing What do you think he has? a) COPD b) Systolic Heart Failure c) Asthma d) Idiopathic pulmonary fibrosis e) Neuromuscular Disease |
COPD:
He probably does not have asthma, probably chronic bronchitis |
|
|
Case 1:
- 67 yo Caucasian man presents in clinic with complain of dyspnea and cough - Progressive dyspnea - Cough productive sputum - Leg edema - Wheezing and nighttime breathing problems - Significant smoking history - Some hobby and occupational exposures (limited) to respiratory irritants Exam: - Speaking in short sentences (mild respiratory distress) - Tachycardia, low SpO2 - JVD, trace edema, cyanosis, barrel chested, hyper-resonance, decreased breath sounds, scattered wheezing Why does this patient have JVD and leg swelling? |
Cor pulmonale - advanced lung disease can lead to RH failure
|
|
|
Case 1:
- 67 yo Caucasian man presents in clinic with complain of dyspnea and cough - Progressive dyspnea - Cough productive sputum - Leg edema - Wheezing and nighttime breathing problems - Significant smoking history - Some hobby and occupational exposures (limited) to respiratory irritants Exam: - Speaking in short sentences (mild respiratory distress) - Tachycardia, low SpO2 - JVD, trace edema, cyanosis, barrel chested, hyper-resonance, decreased breath sounds, scattered wheezing What kind of COPD is this? |
Chronic Bronchitis - blue bloater
|
|
|
Case 1:
- 67 yo Caucasian man presents in clinic with complain of dyspnea and cough - Progressive dyspnea - Cough productive sputum - Leg edema - Wheezing and nighttime breathing problems - Significant smoking history - Some hobby and occupational exposures (limited) to respiratory irritants Exam: - Speaking in short sentences (mild respiratory distress) - Tachycardia, low SpO2 - JVD, trace edema, cyanosis, barrel chested, hyper-resonance, decreased breath sounds, scattered wheezing What tests do you think will help you diagnose and care for this patient? |
- Chest x-ray
- Pulmonary function studies - Arterial blood gases - Echocardiogram - EKG - BNP |
|
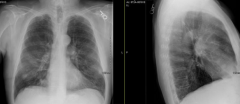
Case 1:
- What do you notice about his chest x-ray? |
- AP diameter is enlarged (hyperinflation)
- More air retrosternally than expected - Flat diaphragm - Decreased lung markings |
|

Case 1:
Which flow volume loop would this patient have? |

A - bunny hill is a sign of obstructive disease (Chronic Bronchitis)
|
|
|
Case 1:
What would you expect to see if we did a diffusion study on this patient? |
He is already hypoxic, so diffusion capacity would probably be <40% (bad)
|
|
|
Case 2:
- 9yo girl presents with complaints of SOB and wheeze What is the differential diagnosis for a young patient with these complaints? |
- Cardiac: CHF and Bronchial compression
- Lungs: asthma, cystic fibrosis, pneumonia, pertussis, croup, aspiration, bronchiolitis - Upper airway: rhinitis (allergic or non), adenoid hypertrophy, paroxysmal vocal fold motion, laryngeal edema/anaphylaxis, tumor - Other: myopathy, anemia, hyperventilation, deconditioning |
|
|
Case 2:
- 9yo girl presents with complaints of SOB and wheeze - Symptoms occur about 5-10 minutes into playing soccer with chest tightness - Similar feeling after playing with cats and following viral colds - Otherwise denies SOB, wheeze, or chest tightness at other times - Coughs in middle of night about 2x/week What is the top differentials for this patient? |
- Asthma
- Paradoxical vocal fold motion - Rhinitis (allergies) |
|
|
Case 2:
- 9yo girl presents with complaints of SOB and wheeze - Symptoms: intermittent SOB, wheeze, chest tightness, night cough - Course: episodic - Triggers: exercise, cats, viral colds - Takes albuterol which partially helps, not used with aerochamber - Nebulized albuterol and 5 days of oral prednisone after a viral URI cleared symptoms - PMH: eczema, sinusitis 2-3x/year - Meds: albuterol, benadryl - FHx: mom has asthma, sister has peanut allergy - Environmental: dad smokes, pet dog - Good student, plays on select soccer team How does this information support the differential diagnoses? |
Asthma:
- Personal and family history of atopy (allergy/hypersensitivity) - Smoke and pet in home Allergic Rhinitis: - Personal history of seasonal rhinoconjunctivitis Paradoxical Vocal Fold Motion: - Student athlete (type A personality, very competitive) Cystic Fibrosis - May be atypical presentation(?) |
|
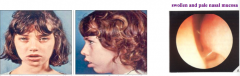
Case 2:
- 9yo girl presents with complaints of SOB and wheeze - Symptoms: intermittent SOB, wheeze, chest tightness, night cough - Course: episodic - Triggers: exercise, cats, viral colds - Albuterol - partially helps, no aerochamber - Nebulized albuterol & 5 days of oral prednisone after viral URI cleared symptoms - PMH: eczema, sinusitis 2-3x/year - Meds: albuterol, benadryl - FHx: mom - asthma, sister - peanut allergy - Envir: dad smokes, pet dog - Good student, plays on select soccer team Exam: - Mouth breathing, nasal mucosa pale, oropharynx w/ cobblestoning - Prolonged expiratory phase, wheeze on expiration - Dry plaques (eczema) What tests should be ordered? |
- Spirometry
- Allergy testing |
|
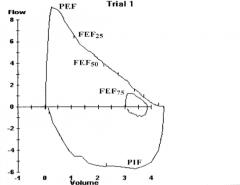
What does this spirometry show? If this was the patient in case 2's spirometry, what diagnosis would you suspect?
|
Normal - could be associated with allergic rhinitis
- Or could be cystic fibrosis |
|
What does this spirometry show? If this was the patient in case 2's spirometry, what diagnosis would you suspect?
|
Flattened inspiratory loop
- Could be d/t paradoxical vocal fold motion - On inspiration, vocal folds close up causing flattening of inspiratory part of loop |
|
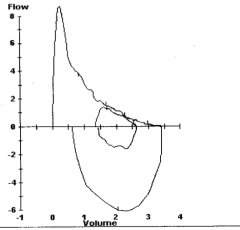
What does this spirometry show? If this was the patient in case 2's spirometry, what diagnosis would you suspect?
|
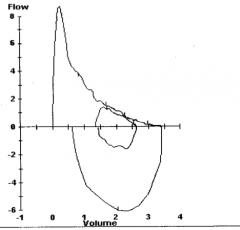
Obstructive - probably asthma
|
|
Spirometry reveals mild obstruction. Four inhalations of a bronchodilator, albuterol, was administered. What defines significant reversibility?
a) Increase in FVC by 12% and 200 ml b) Increase in FEV1 by 12% and 200 ml c) Increase in FVC by 20% and 400 ml d) Increase in FEV1 by 20% and 400 ml e) Increase in FEV1/FVC by 12% and 200 ml |
Increase in FEV1 by 12% and 200 ml
Definition of significant airway reversibility, need BOTH |
|
|
In allergy skin testing, what antibody are you detecting?
a) IgG b) IgM c) IgE d) IgA e) IgD |
IgE is associated w/ type 1 hypersensitivity (allergic reactions)
|
|
|
Case 2:
- 9yo - Symptoms: shortness of breath, wheeze, chest tightness, and cough - Triggers: exercise, cat, viral colds - Personal and family history of atopy - Exam with expiratory wheeze and other signs consistent with atopy - Spirometry reveal reversible airway obstruction - Allergic What is causing our patient’s respiratory symptoms? a) Paradoxical vocal fold motion b) Asthma c) Allergic rhinitis d) Cystic Fibrosis |
Asthma
|
|
|
What is the definition of asthma?
|
Complex clinical syndrome characterized by:
- Variable airflow obstruction - Airway inflammation - Bronchial hyper-responsiveness |
|
|
Why do patients with asthma have a nocturnal cough?
|
- Cooling of airway
- Lower levels of endogenous epi and cortisol - Lungs function best in afternoon, worst at 4am because epi and cortisol keep lungs functioning by reducing inflammatory response |
|
|
What should you consider if someone presents with a nocturnal cough?
|
Asthma
|
|
|
Why was the patient in case 2 only getting partial relief with albuterol?
|
She wasn't using an aerochamber - this allows the meds to get into lungs not in back of throat
|
|
|
What test can you do to confirm if a patient has asthma if the reversibility test didn't work?
|
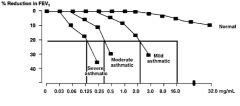
Methacholine Challenge:
- Methacholine causes bronchoconstriction - Patients with asthma will have a reduction in FEV1 with higher concentrations of methacholine and as it is diluted the FEV1 should improve to normal - The more severe the asthma, the more dilute the methacholine can be to still cause significant reduction in FEV1 |
|
|
What are the theoretical causes for the increased prevalence of asthma?
|
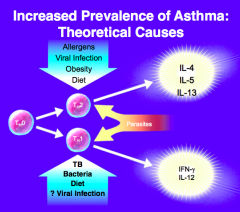
Th2:
- Allergens - Viral infections - Obesity - Diet Th1: - Tuberculosis - Bacteria - Diets - Viral infections |
|
|
What are the implications of the persistent inflammation in asthma?
|
– Infiltration of airway by inflammatory cells
– Hypertrophy of airway smooth muscle – Thickening of basement membrane (lamina reticularis) – Hyperplasia and hypertrophy of submucosal glands – Goblet cell hyperplasia and hypertrophy – Hyperplasia of microvascular dilation – Loss of epithelial cells |
|
|
What is the predominant and characteristic cell seen in the airways of asthma inflammation?
a) Neutrophil b) Eosinophil c) Macrophage d) Lymphocyte e) Basophil |
Eosinophils
|
|
|
What finding in sputum is characteristic of asthma?
a) Lipid laden macrophages b) Neutrophils c) Charcot-Leyden Crystals d) Basophils e) Glycoproteins |
Charcot-Leyden Crystals
|
|
|
What are the potential triggers of asthma?
|
• Allergic
• Viral respiratory infections: RSV, rhinovirus • Exercise • Aspirin • Irritants: Smoke, perfume, pollution • Weather changes: Cold air, humidity |
|
|
What happens when an antigen a patient is allergic to enters their system?
|
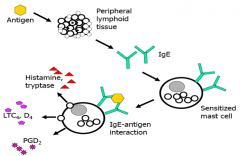
- Peripheral lymphoid tissue recognizes antigen and presents it to B cells
- B cells produce IgE - IgE that is on sensitized mast cells will bind antigen and release histamine/tryptase, LTC4/D4, and PGD2 |
|
|
What do sensitized mast cells release when antigen binds their IgE?
|
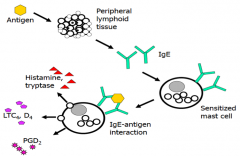
- Histamine, Tryptase
- LTC4, D4 - PGD2 |
|
|
What happens minutes after antigen binds to sensitized mast cells with IgE?
|
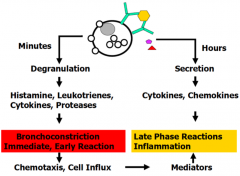
- Degranulation →
- Release of pre-formed Histamine, Leukotrienes (LTC4, D4), Cytokines, and Proteases → - Bronchoconstriction (immediate, early reaction) → - Chemotaxis and cell influx (also helps stimulate late phase reactions / inflammation) |
|
|
What happens hours after antigen binds to sensitized mast cells with IgE?
|
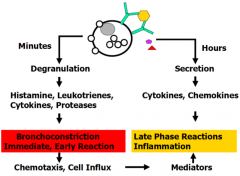
- Secretion of cytokines and chemokines →
- Late phase reactions and inflammation |
|
|
How does exercise trigger asthma?
|
Cooler, drier air causes release of bronchoconstrictor mediators from airway mast cells (cysLTs: LTC4, LTD4, and histamine)
- Normally the airway is humidified, when exercising we don't have time to humidify air so it comes in cooler and drier, releasing the bronchoconstrictor molecules from airway mast cells |
|
|
How does aspirin trigger asthma?
|
- Patients with asthma have a baseline increase in leukotrienes
- Aspirin blocks cyclooxygenase pathway (to produce prostaglandins), thus more substrate (arachidonic acid) gets acted on by 5-lipoxygenase - This leads to more production of leukotrienes that can exacerbate inflammatory effects - Not everyone has this response |
|
|
What are the general principles of treating patients with asthma?
|
- Avoidance of triggers
- Medications |
|
|
What are some methods for avoiding asthma triggers?
|
- Pollen: stay in air-conditioned buildings
- Mold: repair water leaks - Pets: bathe frequently, keep out of bedroom - Cockroach: professional extermination - Dust mite: encasements over bedding |
|
|
How do you determine which asthma medications to give your patient?
|
Depends on severity and what has worked or not worked in the past
|
|
|
What is step 1 in treating patients with intermittent asthma (in patients 0-4y)?
|
Short-acting β-agonist (SABA), as needed
|
|
|
What is step 2 in treating patients with persistent asthma (in patients 0-4y)?
|
- Low-dose inhaled corticosteroids (ICS) - used daily
- Short-acting β-agonist (SABA), as needed - Patient education and environmental control at each step |
|
|
What is step 3 in treating patients with persistent asthma (in patients 0-4y)?
|
- Switch to medium-dose inhaled corticosteroids (ICS) - used daily
- Short-acting β-agonist (SABA), as needed - Patient education and environmental control at each step |
|
|
What is step 4 in treating patients with persistent asthma (in patients 0-4y)?
|
- Medium-dose inhaled corticosteroids (ICS) - used daily
* Long-acting β-agonist (LABA) or montelukast - used daily - Short-acting β-agonist (SABA), as needed - Patient education and environmental control at each step |
|
|
What is step 5 in treating patients with persistent asthma (in patients 0-4y)?
|
- Switch to high-dose inhaled corticosteroids (ICS) - used daily
- Long-acting β-agonist (LABA) or montelukast - used daily - Short-acting β-agonist (SABA), as needed - Patient education and environmental control at each step |
|
|
What is step 6 in treating patients with persistent asthma (in patients 0-4y)?
|
- High-dose inhaled corticosteroids (ICS) - used daily
- Long-acting β-agonist (LABA) or montelukast - used daily * Add oral corticosteroids - used daily - Short-acting β-agonist (SABA), as needed - Patient education and environmental control at each step |
|
|
What should you do before stepping up in management of asthma?
|
- Check if using correct inhaler technique
- Ensure adherence to prescription - Consider environmental control - Look for comorbid conditions |
|
|
What does frequent or increasing use of short-acting β-agonists indicate?
|
Inadequate control and the need to step up treatment
|
|
|
What meds are used for treating asthma?
|
- β-agonists
- Anti-cholinergics - Inhaled corticosteroids - Leukotriene modifiers - Oral steroids - Anti-IgE (Omalizumab) - Theophylline - Cromolyn |
|
|
Which medication leads to the synthesis of anti-inflammatory proteins?
a) Beclomethasone b) Ipratropium bromide c) Zileuton d) Theophylline e) Cromolyn sodium Mechanism? |
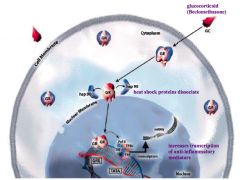
Steroids
- Binds to glucocorticoid receptor - Heat shock proteins dissociate - Enters nucleus and influences transcription of anti-inflammatory mediators |
|
|
What are the cellular effects of corticosteroids?
|
- ↓ numbers of eosinophils (apoptosis)
- ↓ cytokines from Th2 lymphocytes, macrophages, and epithelial cells - ↓ numbers of mast cells and dendritic cells - ↓ leakage between endothelial cells - ↑ β2-receptors on airway smooth muscle - ↓ mucus secretion |
|
|
Which receptor does albuterol bind?
a) Alpha 1 b) Alpha 2 c) Beta 1 d) Beta 2 e) M3 |
Beta-2
|
|
|
What is the mechanism of β2-agonists?
|
- Relaxes airway smooth muscle
- Improves mucociliary function |
|
|
What are the types of β-agonists? When are they used?
|
- Short-acting (Albuterol): as needed, can use before exercise or known trigger exposure
- Long-acting (Salmeterol): used in combination with inhaled steroid, always on a schedule |
|
|
Which medication would be especially beneficial in aspirin exacerbated asthma?
a) Inhaled steroids b) Theophylline c) Leukotriene modifier d) Cromolyn sodium e) Combination inhaled steroid/LABA |
Leukotriene modifier
|
|
|
What are the two leukotriene modifier meds for asthma? Mechanism?
|
- ZilEuton: blocks Enzyme 5-lipoxygenase
- ZafiRlukast: blocks leukotriene Receptor |
|
|
What is the mechanism of Cromolyn Sodium?
|
Stabilizes mast cells so they aren't activated / can't degranulate
|
|
|
Which drug is an anti-IgE antibody? Mechanism?
|
Omalizumab
- Binds IgE and pulls it off of mast cells - When you are exposed to allergens you don't have enough to cross-link and release mediators |
|
|
What in the clinical history makes you think COPD vs asthma?
|
COPD:
- Older age - Tobacco exposure - Diurnal variation not present Asthma: - Younger age - Allergens - Family history - Worse in early morning and at night-time |
|
|
What tests (spirometry/diffusing capacity/CXR) makes you think COPD vs asthma?
|
COPD:
- Spirometry - obstruction not fully reversible - Diffusing capacity - reduced - CXR - hyperinflation and/or bullous changes Asthma: - Spirometry - fully reversible obstruction - Diffusing capacity - normal or INCREASED - CXR - normal to hyperinflated |
|
|
What pathology makes you think COPD vs asthma?
|
COPD:
- Mucous gland METAPLASIA - Loss of alveolar tissue Asthma: - Mucous gland HYPERPLASIA - Intact alveolar structures |
|
|
What type of inflammation makes you think COPD vs asthma?
|
COPD:
- Macrophages and neutrophils ++ - CD8+ lymphocytes Asthma: - Mast cells and eosinophils ++ - CD4+ lymphocytes |
|
|
How does the treatment compare for COPD vs asthma?
|
COPD:
- ICS: for moderate to severe disease - Leukotriene inhibitor: not recommended - Anti-cholinergic: maintenance and in exacerbations Asthma: - ICS: mild to severe persistent disease (used as controller) - Leukotriene inhibitor: may benefit in exacerbations |

