![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back
|
Case 1:
- 56 yo man presents to ED w/ complaints of progressive SOB, now occurring with walking <50 feet, but not at rest - Lower extremity edema for past 3 months - Woke from sleep w/ SOB, been sleeping in chair for past 3 days - Vitals: 100/60, BP 110, RR 24, 89% on RA, afebrile - Exam: moderate distress, tachypneic when speaking a few words, tachycardic; paradoxically split S2 w/ prominent P2; II/VI holosystolic murmur LLSB, II/VI holosystolic murmur apex - Elevated JVP to angle of jaw at 90 degrees; decreased breath sounds and decreased percussion mid to basal lung fields; pitting edema to mid thighs What’s the clinical diagnosis? a) Congestive heart failure (CHF) b) Pneumonia c) Pulmonary Embolism d) Cirrhosis e) Nephrotic Syndrome |
Congestive Heart Failure (CHF)
|
|
|
What is Congestive Heart Failure?
|
State in which the heart is unable to pump blood at a rate sufficient to meet requirements of metabolizing tissues
|
|
|
What symptoms are present in Congestive Heart Failure?
|
Complex of symptoms related to inadequate perfusion of tissues and retention of fluid:
- Dyspnea, coughing, SOB - Fatigue - Pulmonary / peripheral edema - Pleural effusion (Excess fluid in lungs) - Ascites (swelling in abdomen) |
|
|
What is the primary cause of Congestive Heart Failure?
|
Impairment of heart's ability to empty (systolic dysfunction) and/or fill properly (diastolic dysfunction)
|
|
|
How do you determine which type of Congestive Heart Failure a patient has?
|
- Systolic dysfunction: symptoms with EF < 40%
- Diastolic dysfunction: symptoms with EF > 40% |
|
|
What causes Congestive Heart Failure?
|
End product of several diseases:
- Coronary Artery Disease - Hypertension - Valve disease - Idiopathic / familial cardiomyopathies - Infection - Toxicity |
|
|
What is the 5-year survival rate of Congestive Heart Failure?
|
~50%
|
|
|
How common is Congestive Heart Failure in the general population?
|
2.6% of population (~7 million total)
- 50% have systolic dysfunction - 50% have diastolic cysfunction |
|
|
How do you classify the stages of Congestive Heart Failure?
|
- Stage A: at high risk for HF but without structural heart disease or symptoms of HF
- Stage B: structural heart disease w/o signs or sx of HF - Stage C: structural heart disease w/ prior or current sx of HF - Stage D: refractory HF requiring specialized interventions |
|
|
A patient with hypertension, atherosclerotic disease, diabetes, metabolic syndrome, or that is obese; or patients that are using cardiotoxins or with family history of cardiomyopathy, is probably in what stage of heart failure?
|
Stage A: at high risk for HF but without structural heart disease or symptoms of HF
|
|
|
A patient with a previous MI, LV remodeling including LVH and low EF, or asymptomatic valvular disease, is probably in what stage of heart failure?
|
Stage B: structural heart disease w/o signs or sx of HF
|
|
|
A patient with known structural heart disease AND shortness of breath, fatigue, and reduced exercise tolerance, is probably in what stage of heart failure?
|
Stage C: structural heart disease w/ prior or current sx of HF
|
|
|
A patient with marked symptoms at rest despite maximal medical therapy (eg, those who are recurrently hospitalized or cannot be safely discharged from the hospital w/o specialized interventions), is probably in what stage of heart failure?
|
Stage D: refractory HF requiring specialized interventions
|
|
|
How should you treat a patient in Stage A heart failure (at high risk for HF but without structural heart disease or symptoms of HF)?
|
- Treat HTN
- Encourage smoking cessation - Treat lipid disorders - Encourage regular exercise - Discourage alcohol intake, illicit drug use - Control metabolic syndrome Drugs: - ACE-I or ARB in appropriate patients for vascular disease or diabetes |
|
|
How should you treat a patient in Stage B heart failure (structural heart disease w/o signs or sx of HF)?
|
- All measures under stage A
Drugs: - ACE-I or ARB in appropriate patients - β-blockers in appropriate patients Devices in selected patients: - Implantable defibrillators |
|
|
How should you treat a patient in Stage C heart failure (structural heart disease w/ prior or current sx of HF)?
|
Drugs for routine use:
- Diuretics for fluid retention - ACE-I - β-blockers Drugs for selected patients: - Aldosterone antagonists - ARBs - Digitalis - Hydralazine / nitrates Devices in selected patients: - Biventricular pacing - Implantable defibrillators Other: - All measures for Stage A and B heart failure - Dietary salt restrictions |
|
|
How should you treat a patient in Stage D heart failure (refractory HF requiring specialized interventions)?
|
Appropriate measures under stages A, B, and C
Options: - Compassionate end-of-life care / hospice - Extraordinary measures: heart transplant, chronic inotropes, permanent mechanical support (LVAD), experimental surgery or drugs) |
|
|
Which of the following is a Class I recommendation for the prevention of chronic HF in patients at high risk of developing HF (Stage A):
a) Angiotensin-converting enzyme inhibitors can be useful to prevent HF in patients at high risk for developing HF due to a history of atherosclerotic vascular disease, diabetes mellitus, or hypertension with associated cardiovascular risk factors b) Angiotensin II receptor blockers can be useful to prevent HF in patients at high risk for developing HF who have a history of atherosclerotic vascular disease, diabetes mellitus, or hypertension with associated cardiovascular risk factors c) Beta-blockers can be useful to prevent HF in patients at high risk for developing HF who have a history of atherosclerotic vascular disease, diabetes mellitus, or hypertension with associated cardiovascular risk factors d) Thyroid disorders should be treated in accordance with contemporary guidelines |
Thyroid disorders should be treated in accordance with contemporary guidelines
A, B, and C are stage B type treatments |
|
|
What is the typical pathologic progression of CV disease?
|
- Myocardial injury (eg, CAD, HTN, diabetes, CM, valvular disease) →
- Pathologic remodeling → - Low ejection fraction → - Death (via sudden death or pump failure) |
|
|
What are the types of pathologic remodeling caused by myocardial injury?
|
- Cellular apoptosis
- Fibrosis - Dilation of LV chamber |
|
|
What system can be activated to compensate for decreased ejection fraction?
|
Renin-Angiotensin-Aldosterone system
- Activated by β-stimulation, CO, Na+ |
|
|
What are the implications of an activated Renin-Angiotensin-Aldosterone system in the context of heart failure?
|
Activation of Angiotensin II → peripheral vasoconstriction → afterload → ↓ cardiac output → heart failure
Activation of AngII → Aldosterone secretion → salt and water retention → ↑ plasma volume → preload → ↑ cardiac workload → heart failure |
|
|
What is LaPlace's Law?
|
T = (P * r) / (2 * wt)
- T = Tension - P = Pressure - r = Radius - wt = wall thickness Wall tension is proportional to radius and indirectly to wall thickness |
|
|
What are the implications of increased wall stress due to LV remodeling?
|
Reduced efficiency of pumping mechanism and decreased CO, due to:
- Increased myocardial O2 demand - Decreased pump efficiency - Increased mitral insufficiency - Mechanical dyssynchrony - all of the walls are not contracting at the same time, typically seen when there are electrical problems (eg, left bundle branch block) |
|
|
What is the fundamental mechanism of myocardial dysfunction in heart failure?
|
Ventricular Remodeling
|
|
|
How does Ventricular Remodeling occur?
|
- Hypertrophy and apoptosis of myocytes
- Regression to a molecular phenotype that expresses fetal genes and proteins - Changes in the nature of the ECM |
|
|
Eccentric Left ventricular remodeling results in:
a) Mitral stenosis b) Increased wall stress c) Decreased myocardial oxygen demand d) Decreased LV mass e) Decreased BNP |
Increased wall stress
Remember eccentric LV remodeling is dilatory change - You would have mitral regurgitation, increased myocardial O2 demand, increased LV mass, and increased BNP (surrogate of stretch in atria that acts as a diuretic) |
|
|
Case 1:
- 56 yo man presents to ED w/ complaints of progressive SOB, now occurring with walking <50 feet, but not at rest - Lower extremity edema for past 3 months - Woke from sleep w/ SOB, been sleeping in chair for past 3 days - Vitals: 100/60, BP 110, RR 24, 89% on RA, afebrile - Exam: moderate distress, tachypneic when speaking a few words, tachycardic; paradoxically split S2 w/ prominent P2; II/VI holosystolic murmur LLSB, II/VI holosystolic murmur apex - Elevated JVP to angle of jaw at 90 degrees; decreased breath sounds and decreased percussion mid to basal lung fields; pitting edema to mid thighs Based on his symptoms what is his NYHA functional class? a) NYHA Class I b) NYHA Class II c) NYHA Class III d) NYHA Class IV |
NYHA Class III
- (Significant) limitation of physical activity - Comfortable at rest, but minimal to ordinary activity causes fatigue, palpitations, or SOB |
|
|
What is the definition of NYHA class 1?
|
- No limitation of physical activity
- Physical activity does not cause fatigue, palpitation, or SOB |
|
|
What is the definition of NYHA class 2?
|
- Slight limitation of physical activity
- Comfortable at rest, but physical activity results in fatigue, palpitations, or SOB |
|
|
What is the definition of NYHA class 3?
|
- (Significant) limitation of physical activity
- Comfortable at rest, but minimal to ordinary activity causes fatigue, palpitations, or SOB |
|
|
What is the definition of NYHA class 4?
|
- Unable to carry on any physical activity without discomfort
- Symptoms of heart failure at rest |
|
|
Which of the following is a compensatory mechanism in response to a reduction in left ventricular systolic function:
a) Activation of the sympathetic nervous system b) Venodilation to augment ventricular preload c) Renal sodium and water excretion d) Reduction in arterial vascular resistance to unload the failing ventricle |
Activation of the sympathetic nervous system
|
|
|
What tips can be used when assessing the JVP?
|
- Start by assessing patient sitting upright to exclude a very high JVP (may be more difficult to detect when at a lower angle)
- Inspect both sides of neck - External jugular vein can be used to estimate JVP; confirm a respirophasic component in external jugular vein before accepting it as a measure of JVP - Assess patient at various angles off horizontal until JVP is visible half-way up neck - If JVP does not appear elevated when supine, press on patient's abdomen or RUQ to see if abdominojugular response is present - To distinguish carotid from JVP, apply pressure 1-2 inches below impulse, if it disappears it was the jugular vein, if it persists it was the carotid artery |
|
|
How should you start an exam of JVP?
|
- Start by assessing patient sitting upright to exclude a very high JVP (may be more difficult to detect when at a lower angle)
- Inspect both sides of neck |
|
|
What can be used to estimate JVP?
|
External jugular vein can be used to estimate JVP; confirm a respirophasic component in external jugular vein before accepting it as a measure of JVP
|
|
|
At what angle should you assess the JVP?
|
- Start by assessing patient sitting upright to exclude a very high JVP (may be more difficult to detect when at a lower angle)
- Assess patient at various angles off horizontal (eg, supine, 30°, or 45° off horizontal, sitting, or standing) until JVP is visible half-way up neck |
|
|
What should you do if the JVP does not appear elevated when supine?
|
Press on patient's abdomen or RUQ to see if abdominojugular response is present
|
|
|
How can you distinguish the carotid from the jugular venous impulse?
|
Apply pressure 1-2 inches below impulse, if it disappears it was the jugular vein, if it persists it was the carotid artery
|
|
|
Case 1:
- 56 yo man presents to ED w/ complaints of progressive SOB, now occurring with walking <50 feet, but not at rest - Lower extremity edema for past 3 months - Woke from sleep w/ SOB, been sleeping in chair for past 3 days - Vitals: 100/60, BP 110, RR 24, 89% on RA, afebrile - Exam: moderate distress, tachypneic when speaking a few words, tachycardic; paradoxically split S2 w/ prominent P2; II/VI holosystolic murmur LLSB, II/VI holosystolic murmur apex - Elevated JVP to angle of jaw at 90 degrees; decreased breath sounds and decreased percussion mid to basal lung fields; pitting edema to mid thighs What’s the first medication that should be administered in the Emergency Department? a) Alpha-blockers b) B-blockers c) Calcium Channel Blockers d) Digoxin e) Diuretics |
Diuretics
- You want to make the patient feel better first before you start giving them therapies that help their HF - Diuretics, decrease preload, decrease pulmonary capillary wedge pressure, also has some vasodilating properties - Diuretics can work very quickly and help you feel better even before you start urinating * Key was that he has volume overload (JVP to angle of jaw and pitting edema); his JVP tells you his RA P was probably >20 (should be <5) |
|
|
What are the benefits of diuretics in a fluid overloaded patient?
|
- Diuretics, decrease preload, decrease pulmonary capillary wedge pressure, also has some vasodilating properties
- Diuretics can work very quickly and help you feel better even before you start urinating |
|
|
What is the most important marker of the status of intravascular volume?
|
Jugular Venous Pressure (JVP)
|
|
|
What is the evidence for congestion (elevated filling pressure)?
|
- Orthopnea
- High JVP - Increasing S3 - Loud P2 - Edema - Ascites - Rales (uncommon) - Abdominojugular reflux - Valsalva square wave |
|
|
What is the evidence for low perfusion?
|
- Narrow pulse pressure
- Pulsus alteration - Cool forearms and legs - May be sleepy, optunes - ACE-I related symptomatic hypotension - Declining serum Na+ level - Worsening renal function |
|
|
What is the purpose of assessing a patient for congestion and perfusion?
|
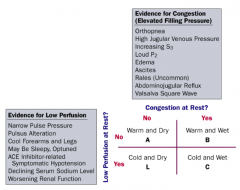
Determine if they are arm warm or cold, and if they are wet or dry
|
|
|
What makes a patient "warm and dry"?
|
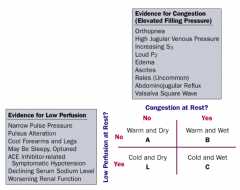
- No congestion at rest
- Normal perfusion at rest |
|
|
What makes a patient "cold and dry"?
|
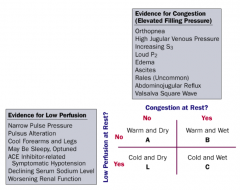
- No congestion at rest
- Low perfusion at rest |
|
|
What makes a patient "warm and wet"?
|
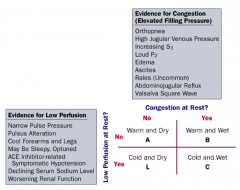
- Congestion at rest
- Normal perfusion at rest |
|
|
What makes a patient "cold and wet"?
|
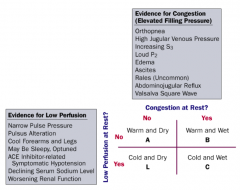
- Congestion at rest
- Low perfusion at rest |
|
|
What regulates venous return?
|
- Respiratory pump
- Skeletal muscle pump |
|
|
How does the respiratory pump affect venous return?
|
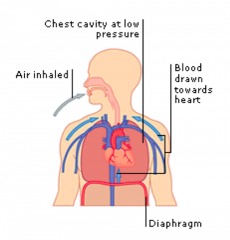
Inspiration → ↓ Intrathoracic pressure → ↑ Venous return to RA = ↑ Preload
|
|
|
How does the skeletal muscle pump affect venous return?
|
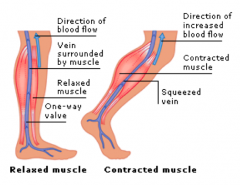
Leg muscle contraction → ↑ Venous return to RA = ↑ Preload
|
|
|
What is the initial management for Congestive Heart Failure patient presenting to the ED?
|
Diuretics
- No mortality benefit - BUT, therapy is directed at symptom relief! |
|
|
What is the effect of diuretics in patients with CHF?
|
- Reduces fluid volume and preload
- Reduces heart size, improves efficiency, and reduces wall stress - Reduces edema (and its symptoms) |
|
|
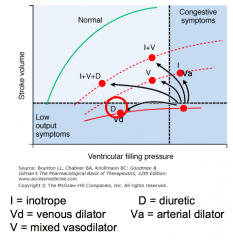
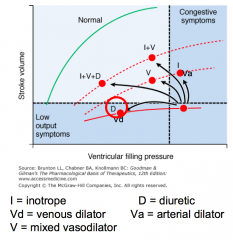
What is the effect of inotropes on stroke volume and ventricular filling pressure?
|
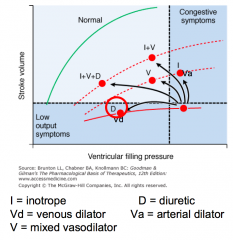
Inotropes: increases stroke volume, with no change in ventricular filling pressure
(the same as an arterial dilator) |
|
|
What is the effect of venous dilators on stroke volume and ventricular filling pressure?
|
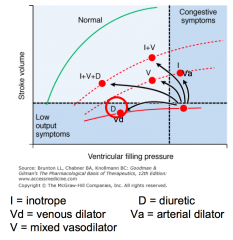
Venous dilators: decreases ventricular filling pressure with no increase in stroke volume
(the same as a diuretic) |
|
|
What is the effect of arterial dilators on stroke volume and ventricular filling pressure?
|
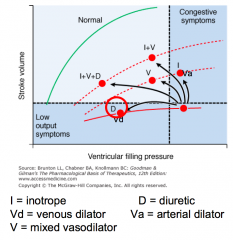
Arterial dilators: increases stroke volume with no change in ventricular filling pressure
(the same as an inotrope) |
|
|
What is the effect of mixed vasodilators on stroke volume and ventricular filling pressure?
|
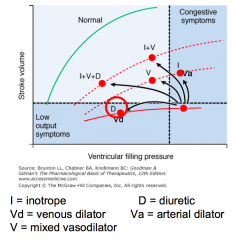
Mixed vasodilators: decreases ventricular filling pressure and increases stroke volume
|
|
|
What is the effect of diuretics on stroke volume and ventricular filling pressure?
|
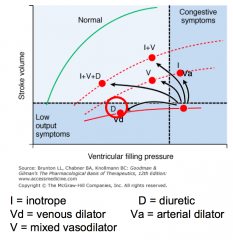
Diuretics: decreases ventricular filling pressure with no change in stroke volume
(the same as a venous dilator) |
|
|
What are the current treatments for CHF? Why?
|
- Diuretics: reduces fluid volume → ↓ preload
- Vasodilators: decreases preload and/or afterload - Inotropes: augments contractility |
|
|
What is Preload? What can increase it?
|
LV filling pressure / volume / fiber length
- Increased because of increased blood volume and venous tone |
|
|
How can you improve the preload in a patient with CHF?
|
Reduce high filling pressure via:
- Salt restriction - Diuretic therapy - Venodilators (nitrates) |
|
|
What is the degree to which the myocytes are stretched prior to contracting? What is it related to?
|
Preload - related to End Diastolic Volume (EDV)
- Atrial Pressure is a surrogate for preload - Affected by venous BP and rate of Venous Return |
|
|
What are the positive effects of loop diuretics for patients with CHF?
|
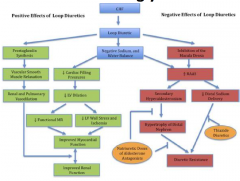
- Prostaglandin synthesis → vascular smooth muscle relaxation → renal and pulmonary vasodilation→ improved renal and myocardial function
- ↓ Cardiac filling pressure → ↓ LV dilation → ↓ functional MR and ↓ LV wall stress and ischemia → improved myocardial function |
|
|
What are the negative effects of loop diuretics for patients with CHF?
|
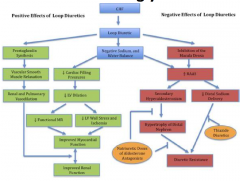
- Inhibition of macula densa → ↑ RAAS → Secondary hyperaldosteronism → hypertrophy of distal nephron → diuretic resistance
- Inhibition of macula densa → ↑ RAAS → ↓ distal sodium delivery → diuretic resistance |
|
|
What are the clinical side effects of diuretics?
|
- Electrolyte abnormalities (hypokalemia, hypomagnesimia, hyponatremia)
- Hypotension - Gout - Hearing loss (rare) - Increased incidence of digoxin toxicity - Renal insufficiency - Muscle cramps |
|
|
What is the purpose of the Swan Ganz Catheter?
|
Measurement of pressures in the:
- Right atrium - Right ventricle - Pulmonary artery - Filling pressure ("wedge" pressure) of the left atrium |
|
|
Case 1:
- 56 yo man presents to ED w/ complaints of progressive SOB, now occurring with walking <50 feet, but not at rest - Lower extremity edema for past 3 months - Woke from sleep w/ SOB, been sleeping in chair for past 3 days - Vitals: 100/60, BP 110, RR 24, 89% on RA, afebrile - Exam: elevated JVP to angle of jaw at 90 degrees - Admitted to hospital, given IV diuretics - good response, making 2L of urine overnight, sx improve - Coronary angiogram is normal - R heart catheterization demonstrates RA pressure of 8 (nl 0-3), PA pressure 55/30/38, PCWP 22 (nl <12), CO 4.5, and CI 2.3 - Echo demonstrates LV EF 25%, mild RV dysfunction, moderate mitral regurgitation, moderate tricuspid regurgitation His kidney function is normal, what is the first medication you would start? a) Enalapril (ACE inhibitor) b) Spironolactone (Aldactone antagnoist) c) Digoxin (cardiac glycoside) d) Isosorbide dinitrate |
Enalapril (ACE inhibitor)
Make sure heart can work as efficiently as possible, without risk of increased resistance; we are dropping afterload with ACE-I This is usually the first drug you use in patient with heart failure UNLESS they have renal failure (look at creatinine) |
|
|
Why would you not use an ACE-I in a patient with heart failure?
|
If they have renal failure (look at creatinine)
|
|
|
What drugs can be used after diuresis to reduce afterload in patients with CHF?
|
- ACE-I and ARBs
- Hydralazine - Nitroprusside (if severely hypertensive) |
|
|
What is Afterload? What can increase it?
|
- Resistance against which the heart must pump (systemic vascular resistance)
- Failing heart is very sensitive to changes in afterload - Systemic Vascular Resistance / Afterload is increased due to increased sympathetic activity and d/t renin-angiotensin system activation |
|
|
What is the tension within the myocyte?
|
T = (P * r) / (2 * wt)
- T = Tension - P = Pressure - r = Radius - wt = wall thickness Wall tension is proportional to radius and indirectly to wall thickness |
|
|
What is the predominant determinant of the afterload / wall tension?
|
Systolic aortic pressure
- LV volume is another determinant |
|
|
What can increase afterload and tension in the myocyte?
|
- Hypertension
- Aortic stenosis - Coarctation of the aorta - Dilated LV cavity |
|
|
How do ACE-I help patient with CHF vs ARBs?
|
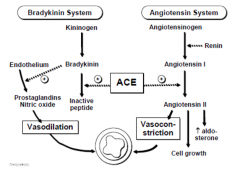
- ACE helps potentiate nitric oxide vasodilation
- ARBs are reserved for patients who can't tolerate ACE-I due to cough |
|
|
What are the actions of Angiotensin?
|
- Potent arterial constrictor (afterload)
- Na+ and water retention through its effects on glomerular filtration and aldosterone secretion - Promotes sympathetic activity by increasing neuronal and adrenal medullary catecholamine release - Arrhythmogenic - Promotes myocardial hypertrophy and apoptosis |
|
|
What are the actions of Aldosterone?
|
- Promotes Na+ and water retention and K+ secretion
- Stimulates fibrosis in the heart and vasculature - Cardiac hypertrophy |
|
|
ACE Inhibitors primarily cause the following change in the kidney:
a) Dilation of the Efferent arteriole b) Constriction of the Efferent arteriole c) Dilation of the Afferent Arteriole d) Constriction of the Afferent Arteriole e) Causes an increase in glomerular pressure |
Dilation of the efferent arteriole (falsely lower GFR)
- Remember that AngII constricts the efferent arteriole because it is trying to increase Renal Blood Flow, so ACE-I does the opposite by dilating efferent arteriole |
|
|
What is the effect of ACE-I compared to placebo in patients with CHF?
|
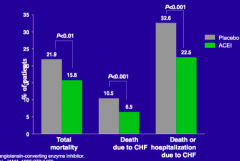
- Decreases total mortality
- Decreases death due to CHF - Decreases hospitalization due to CHF |
|
|
What are the indications for ACE-I in CHF?
|
Routine administration to symptomatic and asymptomatic patients with LV EF < 40%
|
|
|
What limits the tolerance of ACE-I use in CHF? What should you do if these patients have intolerance?
|
- Chronic cough → substitute with ARBs
- Hyperkalemia or renal insufficiency → consider hydralazine and an oral nitrate - Angioedema → consider ARB, but angioedema is infrequently reported |
|
|
Case 1:
He is tolerating enalapril with a systolic blood pressure of 110/75. He continues to diurese on diuretics. He can now lie flat and he is able walk the hallways without any shortness of breath. You decide as his providing doctor to prescribe? a) β-Blocker b) Digoxin c) Warfarin d) A second diuretic |
β-blocker
|
|
|
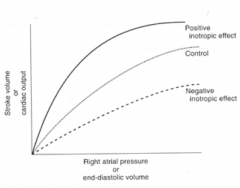
How do β-blockers improve heart failure?
|
- Upregulation of β receptors
- Improved coupling of β receptors to secondary intracellular signals - Alterations in myocardial metabolism - Improves Ca2+ transport - Inhibits renin-angiotensin system - Inhibits endothelial and cytokine release |
|
|
What is the effect of β-blockers on mortality in CHF?
|
β-blockers decrease risk of mortality relative to placebo
- Improves EF after 3 months |
|
|
What is the third drug to use after ACE-I/ARB and β-blockers for heart failure treatment?
|
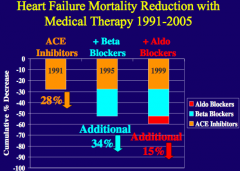
Spironolactone (aldosterone antagonist)
|
|
|
Case 1:
- You see the patient in clinic and he reports he will get SOB after walking a couple hundred of yards, and he can climb 1-2 flights of stairs - No longer wakes up w/ SOB in the middle of the night - His BP is 115/82 and heart sounds are noted to be regularly irregular, so ECG is obtained, demonstrating A. Fib w/ HR of 115 bpm - Offer to perform transesophageal echo to assess for clot and cardiovert patient to sinus rhythm, but refuses and wishes only to take coumadin for stroke prevention In addition to β-blocker’s what other medication may be indicated? a) Calcium channel blockers b) Nitrates c) Coumadin d) Digoxin e) Hydralazine and isosorbide mononitrate |
Digoxin
|
|
|
What kind of medication is Digoxin? Source?
|
- Glycoside derived from plant species from the genus "Digitalis"
- Only cardiac glycoside available in US - Steroid nucleus linked to lactone ring and series of sugars |
|
|
What are the direct effects of Digoxin?
|
- Positive inotropic effect: d/t direct effect to increase contractile state of myocardium, increases stroke volume
- Increases vagal tone: slows HR |
|
|
What are the secondary effects of Digoxin?
|
- Decreased HR
- Arterial and venous dilation - Decreased venous pressure - Normalized arterial baroreceptors |
|
|
What is the molecular mechanism of Digoxin?
|
![Positive inotropic effect d/t INHIBITION OF Na+/K+ ATPase
- Results in ↑ intracellular [Na+], which ↓ driving force for Ca2+ extrusion by Na+/Ca2+ exchanger
- Indirectly results in ↑ intracellular [Ca2+], which increases contractility of h...](https://images.cram.com/images/upload-flashcards/91/84/65/4918465_m.png)
Positive inotropic effect d/t INHIBITION OF Na+/K+ ATPase
- Results in ↑ intracellular [Na+], which ↓ driving force for Ca2+ extrusion by Na+/Ca2+ exchanger - Indirectly results in ↑ intracellular [Ca2+], which increases contractility of heart K+ competes for binding of Digoxin to Na+/K+ ATPase |
|
|
What are the electrophysiological actions of Digoxin?
|
Increased vagal nerve activity
- ↓ firing rate of SA node - ↓ conduction velocity in AV node - Heart block can develop |
|
|
What ECG finding is associated with Digoxin use?
|
Increased PR interval
|
|
|
How often must Digoxin be dosed? Why? How is it administered?
|
- Daily dosing, t1/2 = 36 hours
- Oral administration (60-75% absorbed) |
|
|
What happens to Digoxin to excrete it?
|
Excreted unchanged by kidneys (renal elimination)
|
|
|
When is the ideal dosing of Digoxin based on desired effect?
|
- Max increase in contractility: serum concentration of 1.4 ng/mL
- Neurohormonal benefits occur at lower concentrations (0.5-0.8 ng/mL) |
|
|
What are the adverse effects of Digoxin?
|
- Low therapeutic index (~2)
- Affects all excitable tissues: a) GI tract (most common) - anorexia, nausea, vomiting, diarrhea b) Visual disturbances - blurred vision, photophobia, color disturbances c) Neurologic - disorientation, hallucinations d) Muscular - muscle weakness, fatigue e) Cardiac - arrhythmias (any type) Toxicity enhanced w/ hypokalemia (can be related to diuretic use) Drug interactions: quinidine, verapamil, amiodarone |
|
|
What drugs do you need to be wary of using in a patient taking Digoxin?
|
- Toxicity enhanced w/ hypokalemia (can be related to diuretic use)
- Drug interactions: quinidine, verapamil, amiodarone |
|
|
When should you use Digoxin?
|
- Not a first-line treatment
- Use limited to HF patients w/ LV systolic dysfunction in A. Fib. or in some cases to patients in sinus rhythm who remain symptomatic despite maximal therapy with other therapies - If used, administer a low dose to maintain serum levels between 0.5-0.8 ng/mL |
|
|
How can you increase contractility?
|
- ↑ Intracellular Ca2+
- ↓ Extracellular Na+ (↓ activity of Na+/K+ pump) - Catecholamines (↑ Ca2+ pump in SR) - Digoxin (↓ Na+/K+ pump → ↑ intracellular Ca2+) |
|
|
How can you decrease contractility?
|
- β1-blockade (↓ cAMP)
- Non-dihydropyridine Ca2+ Channel Blockers (verapamil and diltiazem) - Acidosis - Hypoxia and hypercapnea |
|
|
What are the class I anti-arrhythmics? Mechanism?
|
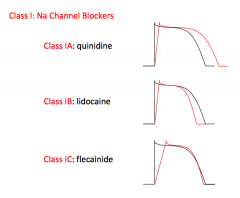
Na+ Channel Blockers
- Class IA: quinidine - Class IB: lidocaine - Class IC: flecainide |
|
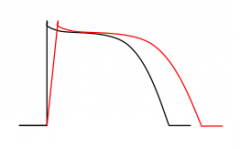
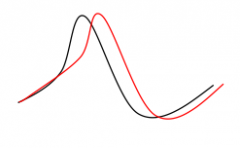
Which type of Class I anti-arrhythmics prolong the AP?
|
Class IA: Quinidine
|
|
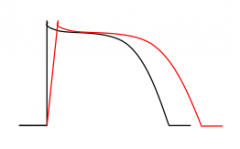
Which type of Class I anti-arrhythmics shorten the AP?
|
Class IB: Lidocaine
|
|
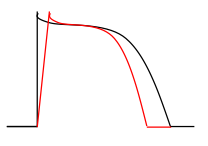
Which type of Class I anti-arrhythmics maintains the length of the AP?
|
Class IC: Flecainide
|
|
|
What are the types of Class II anti-arrhythmics? Mechanism?
|
β-blockers: propranolol and carvedilol
|
|
|
What are the types of Class III anti-arrhythmics? Mechanism?
|
K+ Channel Blockers (prolongs AP)
- Amiodarone - Sotalol - Dofetilide |
|
|
What are the types of Class IV anti-arrhythmics? Mechanism?
|
Ca2+ Channel Blockers:
- Diltiazem - Verapamil |
|
|
What are the basic phases of the cardiac cycle?
|
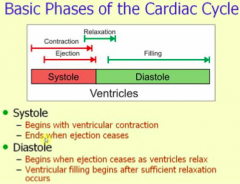
- Systole: begins with ventricular contraction, ends when ejection ceases
- Diastole: begins when ejection ceases as ventricles relax, ventricular filling begins after sufficient relaxation occurs |
|
|
What happens during diastole?
|
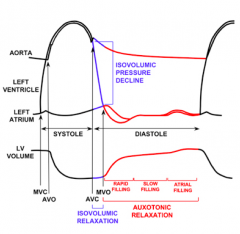
- Initiated by T wave on ECG
- Isovolumic relaxation - Mitral and tricuspid valves open - Early rapid filling, followed by slowed filling - Atrial contraction |
|
|
What happens during systole?
|
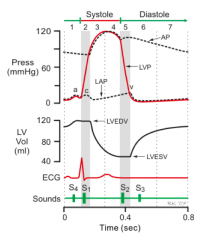
- Initiated by QRS complex on ECG
- Isovolumic contraction - Rapid ejection, followed by reduced ejection |
|
|
How do you calculate Stroke Volume? Normal?
|
SV = EDV - ESV
Normal = 55 - 100 mL |
|
|
How do you calculate Cardiac Output?
|
CO = SV * HR
SV = EDV - ESV |
|
|
How do you calculate Ejection Fraction? Normal?
|
EF = SV / EDV
or EF = (EDV-ESV) / EDV Normal >55% |
|
|
How do you calculate Mean Arterial Pressure?
|
MAP = CO * TPR
MAP = (2/3) * Diastolic Pressure + (1/3) * Systolic Pressure |
|
|
How do you calculate the Pulse Pressure?
|
Pulse Pressure = Systolic Pressure - Diastolic Pressure
Proportional to Stroke Volume |
|
|
What is the location of α1-receptors? Effect of stimulation?
|
- Vascular walls → vasoconstriction
- Heart (effect significantly less) → increases duration of contraction |
|
|
What is the location of β1-receptors? Effect of stimulation?
|
Heart → inotropy (↑ force of contraction) and chronotropy (↑ rate)
|
|
|
What is the location of β2-receptors? Effect of stimulation?
|
Vascular walls → vasodilation
|
|
|
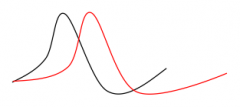
What happens to the compliance curve as it decreases or increases?
|
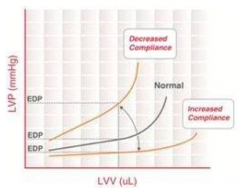
- Normally, as LV volume increases, so does pressure
- Increased compliance curve: less increase in pressure per changes in volume - Decreased compliance curve: greater increase in pressure per changes in volume |
|
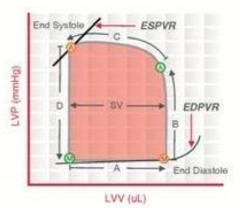
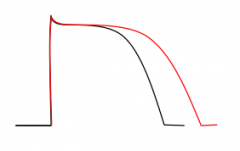
What is happening during "A"?
|
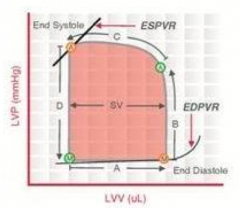
- Mitral valve opens
- Diastolic filling - Mitral valve closes |
|
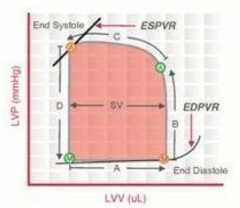
What is happening during "B"?
|
- Mitral valve closes
- Isovolumetric contraction - Aortic valve opens |
|
What is happening during "C"?
|
- Aortic valve opens
- Ejection - Aortic valve closes |
|
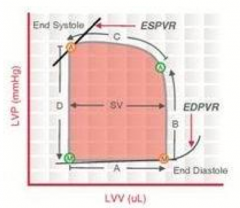
What is happening during "D"?
|
- Aortic valve closes
- Isovolumetric relaxation - Mitral valve opens |
|
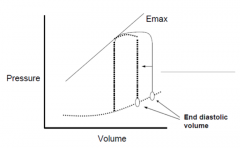
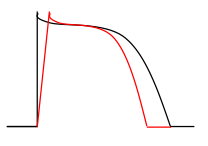
What could cause this change? What change is happening?
|
Decrease in preload
- Decreased EDV |
|
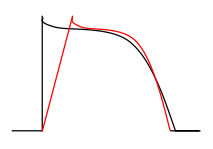
What could cause this change? What change is happening?
|
Increase in afterload
- Increased end-systolic pressure |
|
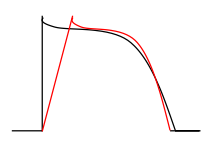
What could cause this change? What change is happening?
|
- Decreased slope of Emax
- Decreased contractility - Decrease in stroke volume |
|
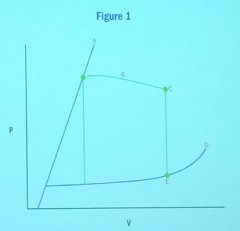
With regard to the Figure, which of the following points or curves will move first if a patient develops an infiltrative process such as amyloid heart disease?
a) A b) B c) C d) D e) E |
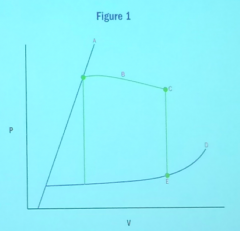
D
|

