![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
69 Cards in this Set
- Front
- Back
|
CHF
|
Heart is unable to pump blood at a rate sufficient ro meet the requirements of metabolizing tissues
Produces a complex of symptoms related to inadequate perfusion of tissues and retention of fluid (dyspnea, fatigues, pulmonary/periphery edema) |
|
|
Primary cause of CHF
|
Impairment of the heart's ability to empty (systolic) and/or fill properly (diastolic dysfunction).
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
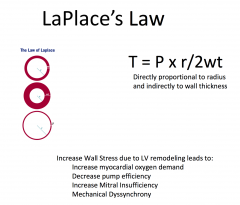
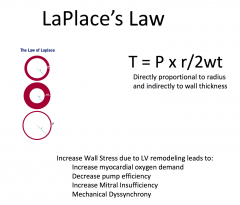
Ventricular Remodeling
|
Fundamental mechanism of myocardial dysfunction in heart failure
Hypertrophy and apoptosis of myocytes Regression to a molecular phenotype that expresses fetal genes and proteins Changes in the nature of the extracellular matrix |
|
|
|
|
|
What is a compensatory mechanism in response to a reduction in left ventricular systolic function?
|
Activation of the sympathetic nervous system
|
|
|
What's the first medication that should be administered in the ER for patients with CHF?
|
Diuretics - for symptom relief
|
|
|
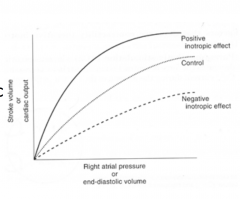
JVP
|
Important marker of the status of intravascular volume
|
|
|
|
|
|
Regulation of Venous Return
|
Affected by two main body pumps:
Respiratory pump: Inspiration leading to decreased intrathoracic pressure resulting in increased venous return to the right atrium and an increase in preload. Skeletal Muscle Pump: Leg muscle contraction leads to increased venous return to right atrium and an increase in preload |
|
|
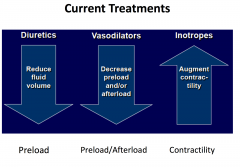
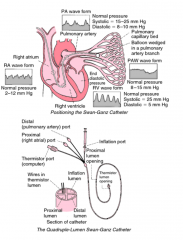
What can be targeted with meds for pts with HF?
|
Afterload, preload, and contractility
|
|
|
Diuretics
|
Mainstay of heart failure management
Reduced fluid volume and preload Reduction in heart size improves efficiency and reduces wall stress Reduce edema |
|
|
|
|
|
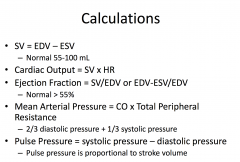
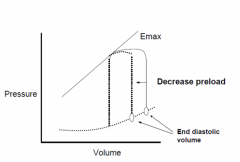
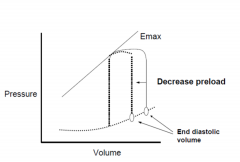
Cardiac performance with systolic heart failure: preload
|
Defined as LV filing
pressure/volume/fiber length Relates to the Frank-Starling mechanism Preload is usually increased because of increased blood volume and venous tone Function of the curve is depressed Reduction of high filling pressure is the goal of: salt restriction, diuretic therapy, and venodilators (nitrates) |
|

|

|
|
|
Preload
|
Degree to which the myocytes are stretched prior to contracting
Related to the End Diastolic Volume Atrial Pressure is a surrogate for preload Affected by venous blood pressure and the rate of venous return |
|
|
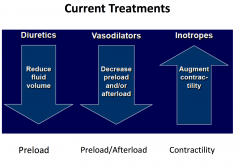
How can you increase your Stroke Volume?
|
By increasing preload up until point when curve plateaus
|
|
|
Diuretic Side Effects
|
Electrolyte abn
Hypokalemia Hypomagnesemia Hyponatremia Hypotension Gout Hearing loss (rare) Increased incidence of digoxin toxicity Renal insufficiency Muscle cramps |
|
|

|
|
|
Pt with CHF has normal kidney function, which medication would you start?
|
Enalapril (Ace-Inhibitor)
|
|
|
Management after diuresis
|
Afterload reduction
- ACE-I - Hydralazine - Nitroprusside (if severely hypertensive) |
|
|
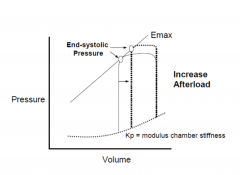
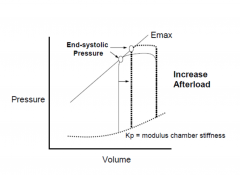
Cardiac Performance with Systolic Heart Failure
|
Resistance against which the heart must
pump (systemic vascular resistance) • Failing heart is very sensitive to changes in afterload • Systemic vascular resistance is increased due to increased sympathetic activity and due to renin-angiotensin system activation • Reduced by: arterial vasodilators (ACE inhibitors, ARBs, hydralazine) |
|
|
Afterload
|
• Load against which the heart contracts to eject blood
• Tension within myocyte ≈ wall stress of the left ventricle during ejection • Systolic aortic pressure is predominant determinant • LV volume is another determinant • Increased by HTN, aortic stenosis, coarctation of the aorta , dilated LV cavity |
|
|
Neuro-hormonal response to CHF
|
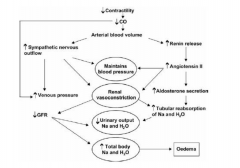
|
|
|
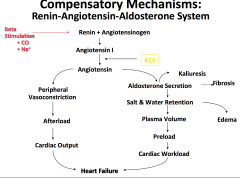
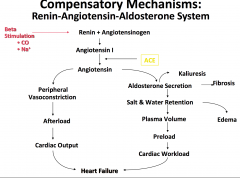
Renin-Angiotensin-Aldosterone System
|
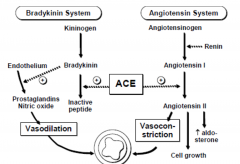
|
|
|
|
|
|
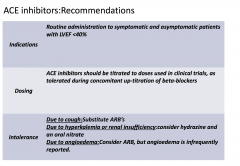
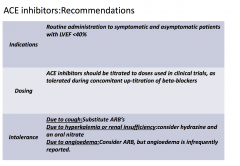
ACE-I primarily cause what change in the kidney?
|
Dilation of the efferent arteriole
|
|
|
|
|
|
Pt is tolerating enalapril with a systolic blood
pressure of 110/75. He continues to diurese on diuretics. He can now lie flat and he is able walk the hallways without any shortness of breath. You decide as his providing doctor to prescribe? |
BBlocker
|
|
|
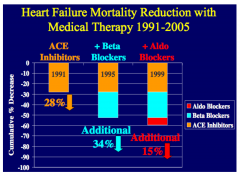
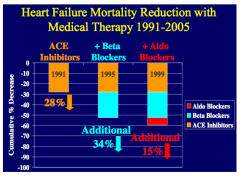
How do beta-blockers improve heart failure?
|
•Upregulation of beta receptors
•Improved coupling of beta receptors to secondary intracellular signals •Alterations in myocardial metabolism •Improved calcium transport •Inhibition of renin-angiotensin system •Inhibition of endothelial and cytokine release |
|
|
|
|
|
Digoxin
|
Glycoside derived plant species from genus digitalis (foxglove)
Only cardiac glycoside available in US Chemically consists of a steroid nucleus linked to a lactone ring and a series of sugars |
|
|
Direct Effects of Digoxin:
|
a. Positive inotropic effect
– Due to a direct effect to increase the contractile state of the myocardium – Increases stroke volume b. Increases vagal tone – Slows heart rate |
|
|
Secondary effects of digoxin
|
a. Decreased heart rate
b. Arterial and venous dilation c. Decreased venous pressure d. Normalized arterial baroreceptors |
|
|
Digoxin: Molecular site of action
|
• Positive inotropic effect due to
inhibition of the Na+,K+-ATPase – results in increased intracellular [Na+] thereby decreasing driving force for Ca2+extrusion by Na+/Ca2+ exchanger – indirectly results in increased intracellular concentration of Ca2+ • K+ competes for binding of digoxin to the Na+,K+ -ATPase |
|
|
Electrophysiological actions of digoxin
|
• At therapeutic concentrations, mainly related to
increased vagal nerve activity – Reduced firing rate of SA node – Decreased conduction velocity in AV node – Heart block can develop • Main observation on the ECG – increased PR interval |
|
|
Pharmacokinetics of Digoxin
|
• t ½ = 36 h (permits daily dosing)
• Orally absorbed (60 – 75% absorbed) • Excreted unchanged by the kidneys (renal elimination) • Max. increase in contractility observed at serum concentration of 1.4 ng/ml • Neurohormonal benefits occur at lower concentrations (0.5 – 0.8 ng/ml) |
|
|
Adverse effects and toxicity of Digoxin
|
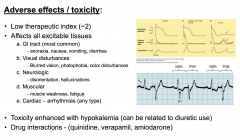
|
|
|
Clinical use of digoxin
|
Not a first-line treatment
• Use limited to heart failure patients with LV systolic dysfunction in atrial fibrillation or in some cases to patients in sinus rhythm who remain symptomatic despite maximal therapy with other therapies • If used, administer a low dose that maintains serum levels between 0.5-0.8 ng/ml |
|
|
HF prognosis correlates most strongly with?
|
Impaired renal function
|
|
|
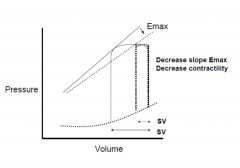
What increases contractility?
|
↑ intracellular Ca2+
– ↓ extracellular Na+ (↓ activity Na+/K+ pump – Catecholamines (↑ Ca2+ pump in SR) – Digoxin (↓ Na+/K+ pump → ↑ intracellular Ca2+) |
|
|
What decreases contractility ?
|
– B1 blockade (↓ cAMP)
– Non-dihydropyridine Ca2+ channel blockers (verapamil and diltiazem) – Acidosis – Hypoxia and hypercapnea |
|
|
|
|
|
|
|
|
|
|
|
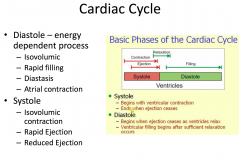
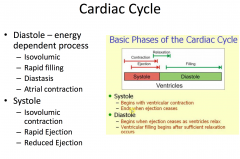
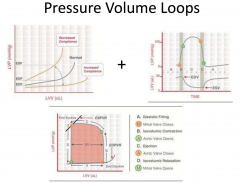
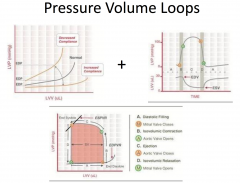
Diastole
|
- Initiated by T-wave on ECG
- Isovolumic relaxation - Mitral and tricuspid valves open - Early rapid filling - Slow filling - Atrial contraction |
|
|
Systole
|
- Initiated by QRS complex on ECG
- Isovolumic contraction - Rapid ejection - Reduced ejection |
|
|
|
|
|
What is true regarding ejection fraction (LVEF) in patients with heart failure?
|
A dilated, thin-walled ventricle usually has a reduced LVEF
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
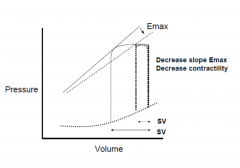
Shifts the curve
|
|
|
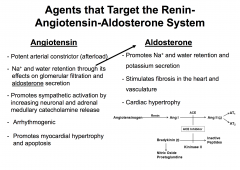
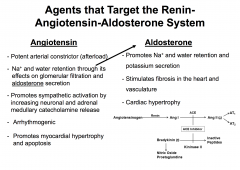
A 56-year-old man presents with a 1-week history
of palpitations and shortness of breath. He has a longstanding history of poorly controlled hypertension. Physical examination reveals an elevated blood pressure of 190/98 mm Hg, elevated jugular venous pressure (JVP), mild hepatomegaly, bilateral pedal edema, and rales at the lung bases. Diagnostic studies reveal concentric left ventricular hypertrophy without significant valvular abnormalities on echocardiogram. What drug is beneficial in the treatment of the patient's condition by virtue of both afterload and preload reduction? |
ACE-I
ACE inhibitors inhibit the conversion of angiotensin I to angiotensin II (AII) through ACE and thus results in favorable modification of the neurohormonal activation in heart failure. They cause favorable hemodynamic effects by causing peripheral vasodilatation, afterload, and blood pressure reduction. They also bring about reduction in the preload through the reduction of aldosterone, which in turn decreases sodium and fluid retention. |
|
|
Loop Diuretics
|
reduce preload by reducing fluid volume
|
|
|
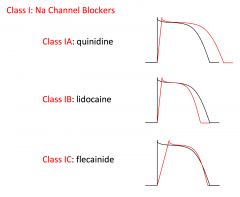
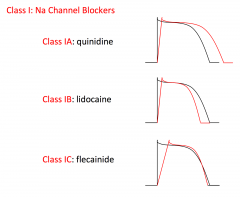
Procainamide
|
class Ia antiarrhythmic agent used in ventricular and
supraventricular arrhythmias. |
|
|
hydralazine
|
used to reduce the afterload by decreasing peripheral vascular resistance and increasing heart rate, stroke
volume, and cardiac output. |
|
|
While performing an in vitro experiment on canine
myocardial cells, you administer an experimental pharmacological agent that acts as a positive inotropic cardiac agent. Administration of this same agent to smooth muscle cells results in smooth muscle relaxation. What medication is the experimental agent most similar to? |
Milrinone
Used short-term in the treatment of decompensated heart failure. Milrinone is a positive inotropic cardiac agent that increases cellular cAMP by inhibiting phosphodiesterase III. On the other hand, this medication results in smooth muscle relaxation, leading to peripheral vasodilatation. Milrinone's vasodilating, inotropic action increases cardiac output and reduces left ventricular pressures without producing significant changes in heart rate and blood pressure. |
|
|
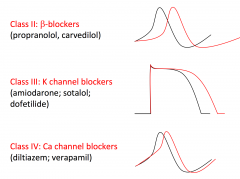
Amiodarone
|
class III cardiac agent that prolongs the action potential duration and the QT interval on ECG by blocking potassium currents in cardiac muscle cells. The medication is used to treat ventricular arrhythmias and is also highly effective in treating supraventricular arrhythmias, such as atrial fibrillation.
|
|
|
A 78-year-old female who is a known case of
congestive cardiac failure presents to the clinic with complaints of a 2-day history of ulcers on her right foot. Examination reveals bilateral pitting pedal edema with 2 small 2X2 cm venous ulcers at the medial malleolus of her right foot along with increased jugular venous pressure (JVP), hepatomegaly, and S3 gallop on cardiac auscultation. The patient is advised to consider compression stocking for the venous ulcer. Application of compression stocking helps reduction of edema through which of the following hemodynamic mechanism? |
Increasing tissue hydrostatic pressure
|
|
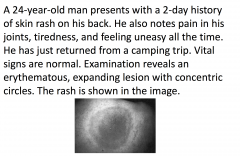
If left untreated, what is a long-term
complication of this patient's condition? |
Myocarditis
This patient's history and clinical picture is suggestive of Lyme disease. Lyme disease is an inflammatory disease characterized by a skin rash, joint inflammation, and flu-like symptoms; it is caused by the bacterium Borrelia burgdorferi and is transmitted by the bite of a deer tick. The figure shows the classic appearance of the rash, erythema chronica migrans. |
|
|
A 60-year-old man you have been treating for
congestive heart failure symptoms has been diagnosed with diabetes mellitus. The endocrinologist who made the diagnosis decided to treat the patient with glipizide 5mg daily since his blood glucose readings are 280mg/dl. You manage the patient's congestive heart failure with enalapril 10 mg daily, and he takes a furosemide 20 mg daily if he needs it. What kind of effect on the patient's hyperglycemia may be expected in these settings? |
Co-administration of ACE inhibitors (captopril,
enalapril) and oral sulfonylurea hypoglycemics results in an increase of the hypoglycemic effect, for which more careful monitoring of blood glucose is advised to avoid pronounced hypoglycemia. Co-administration of thiazide, but not loop diuretics, results in a decrease of hypoglycemic effect. There are no documented interactions of furosemide and sulfonylureas. |
|
|
A 72-year-old man presents with double vision,
weakness, fatigue, nausea, and abdominal discomfort. He describes seeing everything greenish. He suffers from congestive heart failure and is treated for that with digoxin, furosemide, and potassium. He has been taking acetylsalicylic acid since a TIA 2 years ago. He also takes amoxicillin for a urinary tract infection. What medication can cause his symptoms? |
Digoxin
|
|
|
A 55-year-old man presents with dyspnea,
paroxysmal nocturnal dyspnea, nocturia, and anorexia for the past 3 weeks. On examination, he has mild pedal pitting edema. What is the most common cause of his condition? |
Coronary Artery DIsease
|
|
|
A 50-year-old man presents for physical
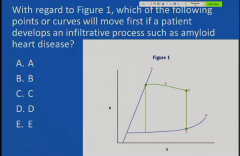
examination, which shows that when lying at an angle, the vertical distance between his sternum and the top pulsation of his jugular vein is 2 cm. On inspiration, it increases to 3.5 cm. On auscultation, his heart has a regular rate and no murmur is heard. His lungs are clear to auscultation. X-ray shows that his heart is a normal size and there is no evidence of pulmonary congestion. Cardiomyopathy is suspected. What is most likely the underlying cause in this patient? |
Amyloidosis is a possible cause of restrictive
cardiomyopathy. This patient presents with signs and symptoms of restrictive cardiomyopathy. An increase in central venous pressure with inspiration is called Kussmaul's sign. Normally, there is a decrease in jugular venous pressure with inspiration. Kussmaul's sign can be seen with restrictive cardiomyopathy. The heart is normal sized with restrictive cardiomyopathy |

