![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
What is the M:F ratio of AAA?
|
4:1
|
|
|
Who is at highest risk for AAA?
|
White Males
|
|
|
What is the most common etiology of AAA?
|
Atherosclerotic in 95%
Inflammatory in 5% |
|
|
What is the most common site of AAA?
|
Infra-renal (95%)
|
|
|
What is the incidence of AAA in adults >60?
|
5%
|
|
|
What % of patients with AAA have a peripheral arterial aneurysm?
|
20%
|
|
|
What are the risk factors for AAA?
|
1. Atherosclerosis
2. Smoking 3. FH 4. HTN 5. Male gender 6. Advanced age 7. CT disease (Marfan, Ehlers Danlos) |
|
|
What are the symptoms of AAA?
|
most are ASYMPTOMATIC and discovered during routine abdominal exam by PCP or US/CT done for other reasons
Sx's range from vague epigastric discomfort to back and abdominal pain |
|
|
What are the signs of AAA rupture? (triad)
|
1. Pulsatile mass on abdominal exam
2. Abd pain 3. Hypotension |
|
|
By how much do AAA's grow each year?
|
about 3-4 mm BUT larger AAA's grow faster
|
|
|
Why do larger AAA's rupture more often and grow faster than smaller AAA's?
|
Laplace's law: wall tension = pressure X diameter
|
|
|
What is the risk of rupture per year based on AAA diameter size?
|
< 5 cm = 4%
5 - 7 cm = 7% > 7 cm = 20% |
|
|
Where does the Aorta bifurcate into the Common Iliac Artery?
|
Umbilicus = palpate between the xiphoid process and umbilicus
|
|
|
What is the DDx of AAA?
|
-Acute pancreatitis
-Aortic dissection -Mesenteric ischemia -MI -perforated ulcer |
|
|
What are the diagnostic tests for AAA?
|
use US to follow clinically
Contrast CT and Arteriogram |
|
|
What is the limitation of Arteriogram?
|
AAA's often have large mural thrombi, which result in falsely reduced diameter b/c only the patent lumen is visualized
|
|
|
What are the signs of AAA on AXR?
|
Calcification in the aneurysm wall, best seen on lateral view = "eggshell" calcifications
|
|
|
What are the indications for surgical repair of AAA?
|
1) AAA > 5 cm, if the patient is not an overwhelming high risk for surgery
2) Rupture of AAA 3) Any size of AAA with rapid growth 4) Sx's/embolization of plaque |
|
|
Describe Endovascular AAA repair
When is it used? |
Repair of AAA by a femoral artery catheter placed stents
In poor operative candidates |
|
|
Why is the graft wrapped by the native aorta?
|
This reduces the incidence of Entero-graft fistula formation
-prevents the formation of a fistula between the graft and intestine |
|
|
What type of repair should be performed with AAA and iliacs severely occluded or iliac aneurysms?
|
Aortobi-iliac or aortobifemoral graft replacement
|
|
|
What is the treatment if the patient has abdominal pain, pulsatile abdominal mass, and hypotension?
|
take the patient to the OR for emergent AAA repair
|
|
|
What is the treatment if the patient has known AAA and new onset of abdominal pain or back pain?
|
CT scan
1. Leak -> straight to OR 2. No leak -> repair during next elective slot |
|
|
What is the mortality rate associated with the following types of AAA treatment:
1. Elective? 2. Ruptured? |
1. < 4% operative mortality
2. ~50% operative mortality |
|
|
What is the leading cause of death postoperatively in a patient undergoing elective AAA treatment?
|
MI
|
|
|
What is the mean normal diameter of the aorta?
|
2 cm
|
|
|
What are the possible operative complications?
|
1. MI
2. Atheroembolism 3. Declamping hypotension 4. ARF 5. Ureteral injury 6. Hemorrhage |
|
|
Why is colonic ischemia a concern in the repair of AAA's?
|
Often the IMA is sacrificed during surgery; if collaterals are not adequate, the patient will have colonic ischemia
|
|
|
What are the signs of colonic ischemia?
|
Heme-positive stool
BRBPR Diarrhea Abd pain |
|
|
What is the study of choice to diagnose colonic ischemia?
|
C-scope
|
|
|
When is colonic ischemia seen postoperatively?
|
usually in 1st week
|
|
|
What is the treatment of necrotic sigmoid colon from colonic ischemia?
|
1. resection of necrotic colon
2. Hartmann's pouch or mucus fistula 3. End colostomy |
|
|
What is the possible long-term complication that often presents with both upper and lower GI bleeding?
|
Aorto-enteric fistula
|
|
|
What are other possible post-op complications? (5)
|
ED due to sympathetic plexus injury
Retrograde ejaculation Aortovenous fistula to IVC Graft infection Anterior Spinal Syndrome |
|
|
What is the Anterior Spinal Syndrome? (4)
Which artery is involved? |
1. Paraplegia
2. Loss of bladder/bowel control 3. loss of pain/temp sensation below level of involvement 4. sparing of proprioception Artery of Adamkiewicz = supplies the anterior spinal cord |
|
|
What are the MC bacteria involved in Aortic Graft infections? (2)
|
1. S. aureus
2. S. epidermidis (usually late) |
|
|
How is a graft infection and an Aorto-enteric fistula treated?
|
Extra-anatomic bypass with resection of the graft
-axillofemoral bypass graft (graft not in a normal vascular path): usually the graft goes from the axillary artery to the femoral artery and then from one femoral artery to the other (fem-fem bypass) |
|
|
Which vein crosses the neck of the AAA proximally?
|

Left Renal Vein
|
|
|
What part of the small bowel crosses in from of the AAA?
|
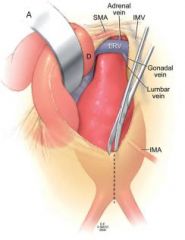
Duodenum
|
|
|
Which large vein runs to the left of the AAA?
|
Inferior Mesenteric Vein
|
|
|
Which artery comes off the middle of the AAA and runs to the left?
|
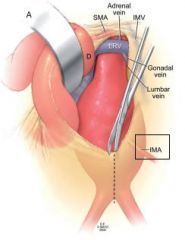
IMA
|
|
|
Which vein runs the RIGHT common iliac artery?
|

LEFT commmon iliac vein
|
|
|
What three things runs anterior to the Common Iliac bifurcation?
|
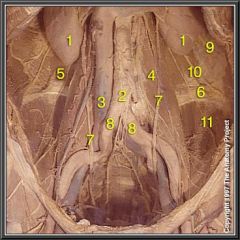
1. Ureter
2. Testicular/Ovarian Artery 3. Testicular/Ovarian Vein |

