![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
165 Cards in this Set
- Front
- Back
|
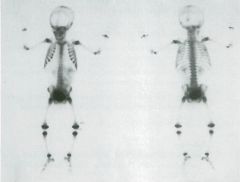
Lower extremity pain in three different patients (A, B, C), all members of the track team.
1. Describe the findings in Patient A. 2. What is the most likely diagnosis? 3. Describe the findings in Patients B and C. 4. Provide the most likely diagnosis for Patients B and C. |
Skeletal System: Stress Fractures
1. Increased activity in a linear pattern along the posterior and medial aspect of both mid-tibias. 2. Shin splints. 3. Patient B: focal ovoid activity posteromedial right tibia at the junction of the proximal two thirds and distal one third. Patient C: focal fusiform activity posteromedially in the right proximal tibia and linear activity along the posteromedial left tibia proximally and more prominently distally. 4. Patient B: stress fracture. Patient C: stress fracture and shin splints. |
|
|
1. Describe the bone scan abnormality.
2. Provide descriptive terms that could be used to describe the pattern in the tibia. 3. Provide the differential diagnosis. 4. The patient may experience clinical symptoms related to another organ system. Discuss the mechanism. |
Skeletal System: Paget's Disease
1. Abnormal highly increased uptake in the entire left femur, which appears bowed and widened, and the distal third of the left tibia, which tapers proximally. 2. A sharp leading edge, referred to as "flame-shaped" or "blade of grass," may be demonstrated on the lytic phase on radiograph and on bone scintigraphy. 3. Paget's disease, fibrous dysplasia, chronic osteomyelitis, primary bone tumors, but principally osteosarcoma. 4. High-output congestive heart failure may occur. Once believed to be the result of arteriovenous shunting within the bone lesion, now hyperemia and increased blood flow through the lesion, and not shunting, are likely causes. |
|

Two patients (A and B) referred with chest wall pain.
1. Describe the bone scan findings. 2. Is there a pattern to the abnormalities? 3. What causes should be considered? 4. Based on the scan findings, provide the most likely diagnoses. |
Skeletal System: Rib Fractures and Sternotomy
1. Patient A: focal increased uptake in multiple ribs posterolaterally and at the costovertebral junctions. Patient B: increased vertical linear uptake in the sternum from the manubrium to the xiphoid. 2. The uptake in adjacent ribs (Patient A) and the vertical uptake in the sternum both have a geometric and characteristic pattern. 3. Trauma or surgery. 4. Patient A: multiple rib fractures. Patient B: median sternotomy for coronary artery bypass grafting (CABG) 6 months ago. |
|
|
A 60-year-old patient with diabetes with cellulitis of the distal foot, referred to rule out osteomyelitis of the left great toe.
1. Describe the physiology of each of the three phases. 2. Describe the scintigraphic findings in this case. 3. Interpret the study. 4. What is the sensitivity and specificity of the three-phase bone scan for osteomyelitis? |
Skeletal System: Pedal Osteomyelitis Three-Phase Positive
1. First phase: arterial blood flow to the bone. Second phase: blood pool or interstitial space distribution immediately following the flow. Third phase: bone uptake phase at 3 hours after injection. All three phases are typically focally increased with osteomyelitis. With cellulitis, only the first two phases are positive. 2. Increased flow, blood pool, and delayed uptake to the left first digit distal phalanx. 3. Consistent with osteomyelitis of the digit. Recent fracture must be excluded with radiography. 4. Sensitivity and specificity of approximately 95% if the radiograph is normal or has only suggestive changes of osteomyelitis. |
|
|
Patient referred for bone scan because of right-sided chest pain.
1. Describe scintigraphic findings. 2. Provide a differential diagnosis. 3. What other examinations may be helpful in this setting? 4. What is the likely reason for ordering the bone scan? |
Skeletal System: Abnormal Breast Uptake
1. Nonuniform abnormal soft tissue uptake exists in the soft tissue overlying the chest, likely in the right breast. 2. Breast cancer, aseptic or septic mastitis, primary skin dis ease, such as psoriasis, vascular or lymphatic obstruction, radiation therapy. 3. Breast examination, mammography, and possible biopsy. 4. To determine whether breast cancer bone metastases are present. |
|
|
Pain in the left shoulder; rule out metastasis.
1. Describe the findings. 2. Name three general processes that could account for the findings. 3. What is the likely primary tumor for which metastases are being excluded? 4. What is the most likely diagnosis? |
Skeletal System: Lymphedema
1. The soft tissues of the left arm are enlarged and show abnormal increased soft tissue activity; the left anterior ribs are uniformly more intense than the right. 2. Venous or lymphatic obstruction, soft tissue neoplasm, soft tissue injury. 3. Breast cancer. 4. Lymphedema secondary to axillary lymph node dissection and left mastectomy. |
|

1. Describe the bone scan findings.
2. Provide the general classification for this finding and the likely diagnosis. 3. Name other conditions that fall into the same spectrum of abnormalities. 4. Are increased risks associated with this condition? |
Skeletal System: Bone Abnormalities of Renal Position
1. The right kidney is not seen in the renal fossa. Nonuniform activity is noted in the right sacroiliac region, which extends beyond the expected superior margin of the bone. 2. Congenital renal anomaly, pelvic kidney. 3. Anomalies of number (supernumerary kidney), position (malrotation), or fusion (horseshoe). 4. Yes. Ureteropelvic junction obstruction, vesicoureteral reflux, decreased function, increased risk of trauma. Urine stasis resulting from distorted anatomy increases the risk of stone formation. |
|
|
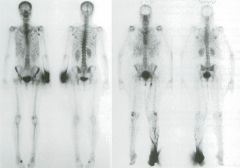
A 67-year-old man has an elevated serum prostate-specific antigen (PSA) level.
1. Describe the findings on this bone scan and interpret the study. 2. What would you predict the serum PSA level to be? 3. Which metastatic cancers have predominantly lytic lesions in bone and thus lower sensitivity for their detection by bone scanning? 4. If a patient with prostate cancer has a significantly elevated serum PSA level postoperatively but negative bone scan findings, what other imaging options are indicated? |
Skeletal System: Metastatic Prostate Cancer
1. Abnormal focal uptake throughout the axial and appendicular skeleton strongly suggestive of metastatic disease. The many distal appendicular lesions usually are seen with latestage disease. 2. Considerably greater than 20 ng/ml. The prevalence of bone scan—evident metastases is less than 1% below this level. 3. Multiple myeloma, followed by thyroid cancer, renal cell carcinoma, lymphoma. 4. CT and MRI have a poor sensitivity for detection of prostate cancer soft tissue/nodal metastases, less than 20%. An In ProstaScint study is indicated. |
|
|
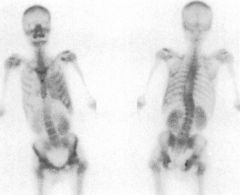
Patient with breast cancer. The serial bone scans are dated as follows: A, 4/97; B, 5/99; C, 8/99; D, 4/00.
1. Describe the bone scan findings and changes over time. The 4/97 scan was completely normal. 2. What is the likelihood of tumor with new focal uptake in a single rib in a patient with known cancer? What is the likelihood with new solitary spine lesions? 3. What are different general scan patterns in metastatic disease? 4. What is the cause of the relatively cold defect in the left hemithorax? |
Skeletal System: Breast Cancer
1. B, New increased uptake at T7 suspicious for tumor; C, multiple new lesions in the thoracic spine, fourth right rib, left sacrum, and single focus in the anterior skull all strongly suspicious for tumor; D, continued progression with new tumor sites in the spine and left sacrum and new focal uptake in left iliac crest, right intertrochanteric femur, and right acetabulum. 2. Less than 20%; greater than 40%. 3. Solitary focal lesion, multiple focal lesions, diffuse involve ment (superscan), cold lesion, soft tissue uptake, flare phenomenon. 4. Breast prosthesis. |
|
|
A 62-year-old patient has right-sided chest discomfort and shortness of breath. A, Posteroanterior chest radiograph;
B, perfusion; C, ventilation. 1. Describe the ventilation-perfusion image findings. 2. Interpret the study. Give your reasoning. 3. What is the likelihood of pulmonary embolus in this patient? 4. What are the most common chest x-ray findings in patients with pulmonary emboli? |
Pulmonary System: High Probability of
Pulmonary Embolus 1. Perfusion is decreased in the right lower lobe except for the superior segment. Ventilation is truncated in the right lower lobe consistent with subpulmonic effusion. 2. High probability for pulmonary embolus. Mismatch between perfusion and ventilation is evident in the basal segments. The perfusion defect is considerably larger than the effusion on the radiograph. 3. Greater than 80%. 4. Most common: normal. Next most common: atelectasis; these also are the most common chest x-ray findings in patients determined by angiography not to have emboli. |
|
|
A chest radiograph (A), posterior 133Xe ventilation (B), and eight-view perfusion study (C) were performed for short
ness of breath. 1. Describe the findings on the ventilation study. 2. Describe the findings on the perfusion study. 3. Provide an interpretation regarding the presence or absence of pulmonary embolism. 4. What term could be applied to this perfusion pattern? |
Pulmonary System: Ventilation-Perfusion—
Stripe Sign, Emphysema 1. Decreased upper lobe ventilation is seen on the single breath with air trapping in both upper lobes and the right lower lobe on washout images. 2. Decreased perfusion to the majority of both lungs, with preserved perfusion in the subpleural lung, most evident at the lung bases and medial aspect of both upper lobes. 3. Low probability. 4. Stripe sign. |
|
|
A young female patient presents at the emergency department with chest pain. Chest radiographs (A, B), perfusion
scan (C), and ventilation study (D) are shown. 1. Describe the findings on the chest radiograph. 2. Describe the perfusion and ventilation scans. 3. Categorize the study regarding the presence or absence of pulmonary embolism using PIOPED criteria. 4. What is the most common finding on chest radiographs with thromboembolism? |
Pulmonary System: Hampton's Hump—
Intermediate Probability 1. Posteroanterior and lateral chest radiographs demonstrate a pleural-based opacity in the lateral right lung base. 2. A single wedged-shaped, pleural-based defect in the same location as the radiographic abnormality, probably the anterobasal segment of the right lower lobe. Normal 133Xe ventilation study. 3. Intermediate probability for pulmonary embolism. 4. Chest x-ray findings in pulmonary embolus without infarction are uncommon. When present, they are usually associated with a large, central embolus. Discoid atelectasis is the next most common finding. |
|
|
A 39-year-old woman had acute upper abdominal pain. Cholescintigraphy was requested.
1. What patient preparation is required before cholescintigraphy? 2. Which hepatobiliary radiopharmaceuticals are available in the United States? 3. What are the radiopharmaceuticals mechanisms of uptake and their differences? 4. Has acute cholecystitis been ruled out? With what degree of certainty? |
Hepatobiliary System: Cholescintigraphy—
Normal Study 1. No oral intake for 3 to 4 hours before radiopharmaceutical injection. 2. 99mTc disofenin (DISIDA), Hepatolite. 99mTc mebrofenin (BrIDA), Choletec. 3. Both are iminodiacetic acid (IDA) analogues, extracted and excreted by hepatocytes into the biliary system. Mebrofenin has higher hepatocyte extraction (98% vs. 88%). 4. Yes. Acute cholecystitis (cystic duct obstruction) is ruled out with a high degree of certainty. The false-negative rate is 1% to 5%. |
|
|
A 35-year-old man has been comatose for 2 weeks since a recent severe head injury. The electroencephalogram (EEG)
is flat and he is being considered as an organ donor. 1. If the EEG is a flat line, why is another study indicated? 2. What are the clinical findings of brain death? 3. List two different types of radiopharmaceuticals with different mechanisms that could be used for this study. 4. What are the scintigraphic findings and the diagnosis? |
Central Nervous System: Brain Death
1. An isoelectric flat EEG can be caused by barbiturates, depressive drugs, or hypothermia. 2. Deep coma, no brain stem reflexes or spontaneous respira tion, exclusion of reversible causes, and the cause of the brain dysfunction must be diagnosed. 3. 99mTc diethylenetriaminepentaacetic acid (DTPA) or 99mTc pertechnetate can be used as a brain flow study (radionuclide angiogram). However, 99mTc HM-PAO and 99mTc ethyl-cysteinate dimer (ECD) have the advantage of irreversible cellular binding on the first pass, allowing for delayed images. 4. No blood flow to the cerebral cortex. Brain blood flow study consistent with brain death. This is a 99mTc DTPA study. 99mTc HM-PAO would show salivary uptake. With normal brain perfusion, cerebral cortical activity would be seen. |
|
|
A 55-year-old man with hypercalcemia has an elevated serum PTH level. Images are taken at 5 minutes and at 1 and
2 hours. 1. Which radiopharmaceutical is being used, and what is the rationale for this technique? 2. What is the diagnosis? 3. What is the accuracy of this study? 4. What is the most common cause for a false-positive study result? |
Endocrine System: Hyperparathyroidism
1. 99mTc sestamibi (MIBI) is taken up by the thyroid and para thyroid tissue, but washes out more rapidly from the thyroid. 2. Parathyroid adenoma in the region of the left lower lobe of the thyroid. 3. Greater than 90% predictive value for preoperative local ization of parathyroid adenoma; lower test accuracy for hyperplasia and small tumors. 4. Thyroid follicular adenoma. |
|
|
A patient has elevated serum calcium and parathyroid hormone levels and normal findings on neck examination.
1. What other protocol in addition to dual-phase (early and delayed) 99mTc sestamibi imaging can be used to evaluate for parathyroid disease? 2. Describe how that procedure is performed. 3. Describe the findings. Left: 99mTc sestamibi; middle: 123I; right: subtraction. 4. List the differential diagnosis and the most likely diagnosis. |
Endocrine System: Parathyroid Adenoma
1. Dual-isotope imaging with subtraction, in the past using 201Tl and 99mTc pertechnetate, and more recently using 123I and 99raTc sestamibi (MIBI). 2. 123I by mouth. After a delay of 2 to 3 hours, an anterior 123I thyroid scan is obtained. Without moving the patient, an image is obtained after intravenous injection of 99mTc MIBI. The I23I image is computer subtracted from the 99mTc MIBI image. 3. The I23I thyroid scan appears normal, although the left lobe extends more inferiorly (middle). The MIBI image (left) shows an asymmetrical bulbous configuration in the region of the right lower pole of the thyroid. Subtraction demonstrates focal radiotracer compatible with parathy roid adenoma at the lower pole of the right thyroid (right). 4. Parathyroid, thyroid adenoma, parathyroid, thyroid carci noma, metastatic carcinoma. |
|
|
A 13-year-old girl adolescent with sickle cell disease, low-grade fever, arm, leg, and back pain was referred for a bone
scan (A). The scan was repeated 1 year later; the patient now has arm and back pain (B). 1. Describe the scintigraphic bone and soft tissue findings. 2. What is the likely diagnosis? 3. What other nuclear medicine study can detect sickle infarcts? 4. How can osteomyelitis be differentiated from bone infarct? |
Skeletal System: Sickle Cell Disease
1. A, Abnormal increased uptake in the proximal right humerus, left distal femur, multiple sites in the thoracic and lumbar spine. B, Uptake in the right ulna and left pos terior ninth rib. Subtle soft tissue uptake is present in the region of the spleen. 2. Sickle cell crises with infarcts. 3. 99mTc sulfur colloid bone marrow scan. 4. Combined 99mTc bone scan and marrow scan early in the acute crisis. |
|
|
A 65-year-old man had had intermittent rectal bleeding for 2 days.
1. Describe the scintigraphic findings during this 90-minute study. 2. What is the purpose of the oblique/lateral pelvic view (last image) in this case? 3. What is your interpretation of the study? 4. What are the criteria for diagnosing and localizing a bleeding site? |
Gastrointestinal System: Rectal Bleeding
1. Abnormal activity accumulates early in the lower midline pelvis. The appearance is changing over time and seems to decrease and then increase again. 2. To differentiate activity in the rectum from bladder and penis, in this patient the activity is seen in the rectum. 3. Positive for gastrointestinal bleeding is not the answer. Localization is critical. The 90-minute lateral view con firms that this is rectal bleeding. 4. New activity, increases in amount over time, and moves intraluminally. |
|
|
A 53-year-old woman was referred for recent enlargement of the right lower lobe of a known multinodular thyroid
gland and a suppressed TSH level. The patient had radiation therapy for acne as a teenager. 1. Describe the scintigraphic findings of this 99mTc pertechnetate scan {left to right: anterior, left anterior oblique, right anterior oblique). 2. Give the likely diagnosis. 3. What are the therapeutic options? 4. What is the likelihood of thyroid cancer in this patient? |
Endocrine System: Toxic Nodular Goiter and
Thyroid Cancer 1. Multiple hot and cold regions throughout both lobes with apparent suppression of nonnodular gland. 2. Multinodular toxic goiter. 3. Biopsy. If benign, then 131I therapy or surgeiy for multi nodular goiter. 4. The likelihood of thyroid cancer is less than 5% in patients with a multinodular goiter. A dominant nodule increases the suspicion for cancer. A history of radiation therapy to the head and neck significantly increases this patient's risk of thyroid cancer. |
|
|
A 55-year-old woman is referred for a thyroid scan to evaluate a palpable thyroid nodule. Left to right views are ante
rior, right anterior oblique, and left anterior oblique. 1. What are the two radiopharmaceuticals used for thyroid scintigraphy, their photopeaks, and physical half-lives? 2. What is the likelihood of thyroid cancer in this patient? 3. What would you recommend as the next diagnostic or therapeutic procedure? 4. What imaging method is used here? What is its image resolution? |
Endocrine System: Cold Thyroid Nodule
1. Intravenous 99mTc pertechnetate, 140 keV, 6 hours; oral sodium 123I, 159 keV, 8 hours. 2. A single cold nodule has a 15% to 20% chance of malignancy. 3. Aspiration needle biopsy. 4. Pinhole collimator. 4 to 6 mm. |
|
A 2-year-old child has an abdominal mass.
1. Describe the scintigraphic bone scan findings. 2. Name a likely organ of origin. 3. What is the most likely diagnosis? 4. Is the current examination adequate for staging of the patient's illness? |
Skeletal System: Neuroblastoma
1. Large region of nonuniform abnormal soft tissue uptake predominantly in the left side of the abdomen that appears to cross the midline. Its boundaries cannot be distinguished from the two kidneys. 2. Adrenal gland. 3. Neuroblastoma. 4. No. |
|

1. Describe the abnormal bone scan findings in scan A.
2. Provide a differential diagnosis. 3. Describe the findings in scan B, a delayed spot image. 4. Explain the change and provide the most likely diagnosis. |
Skeletal System: Extrarenal Pelvis and Mobile Solitary Right Kidney
1. Solitary right kidney with a prominent renal pelvis. Incidental uptake at antecubital injection site. 2. Ureteropelvic junction obstruction or obstruction secondary to other processes, extrarenal pelvis. 3. The renal pelvis has drained and the kidney is now seen inferomedial to its prior location. 4. Image B was taken with the patient erect, leading to gravity drainage of an extrarenal pelvis. The kidney is mobile (ptotic). |
|
|
Because of a "jaw problem", a bone scan (A) and a bone scan and CT-30 reconstruction (B) were obtained in two children.
1. Describe the bone scan findings. 2. What additional information would be helpful? 3. Provide a short differential diagnosis. 4. The mother says there is no known disease in the child (B) or family. What is the most likely diagnosis? |
Skeletal System: Fibrous Dysplasia
1. A shows increased uptake in the entire mandible. B shows intense increased uptake in the mandible and maxilla, which appear deformed and overgrown. 2. Check the rest of the bone scan for other sites; obtain a history of known underlying or familial disease. 3. Fibrous dysplasia, cherubism. 4. Fibrous dysplasia. |
|
1. Describe the findings in patient A.
2. Describe the findings in patient B. 3. Provide the most likely reason for this appearance. 4. Explain the mechanism for the scan appearance. |
Skeletal System: Radiopharmaceutical
Infiltration, Scatter, and Lymph Node Uptake 1. Intense uniform activity in the soft tissues of the distal left forearm and focal activity in the left axilla, nonuniform activity in the left lateral buttock. 2. Intense activity in the left foot, linear activity indicating lymphatic channels, and left inguinal lymph node. Scatter is seen lateral to the left foot. 3. Partial extravasation of the bone radiotracer at the site of intravenous injection in the left forearm. 4. Demonstration of an axillary lymph node because of lym phatic clearance of the extravasated radiopharmaceutical. Scatter from the arm infiltrate results in apparent (but unreal) increased activity in the buttock. |
|
|
Two patients have low back pain. Patient A has blood pool (left) and delayed images (right) available; for Patient B,
only delayed images are shown. 1. Describe the bone scan abnormalities. 2. Provide the differential diagnoses. 3. List three other sites that are at increased risk for the same process. 4. What is the most likely underlying process in both patients? |
Skeletal System: Sacral Insufficiency Fracture
1. Patient A has increased blood pooling and delayed uptake bilaterally in the region of the sacroiliac joints and across the sacrum (H pattern). The bone scan for Patient B demonstrates abnormal increased radiotracer in a curvilin ear linear pattern across the lower sacrum. 2. Both of these are diagnostic of sacral insufficiency fractures. 3. Proximal femur, wrist, and proximal humerus. 4. Osteoporosis. |
|
|
An elderly woman with a history of prior right hip fracture comes to the emergency department because of pelvic pain and inability to walk. A bone scan was obtained.
1. Describe the scintigraphic findings. 2. What is the differential diagnosis? 3. What is the most likely diagnosis? 4. Name three medical conditions that predispose patients to this underlying disease process. |
Skeletal System: Multiple Insufficiency Fractures
1. Multiple focal areas of increased radiotracer uptake are noted in several ribs, multiple sites in both pubic rami, lower sternum, and multiple vertebra. 2. Multifocal involvement by benign or malignant tumor, multifocal osteomyelitis, fractures. 3. Multiple insufficiency fractures. Degenerative change is present in the right shoulder and postoperative change related to previous right hip orthopedic fixation. 4. Hypercortisolism, hyperparathyroidism, hyperthyroidism. |
|
|
A 55-year-old man with exertional chest pain had a stress single photon emission computed tomography (SPECT)
myocardial perfusion study. 1. Describe the perfusion abnormalities and give your interpretation. 2. Name the culprit vessel or vessels. 3. List any ancillary scan findings. 4. List clinical findings related to the stress test relevant to interpretation of the scan. |
Cardiovascular System: Left Anterior
Descending Artery Ischemia 1. Severe decreased perfusion in the majority of the anterior wall, apex, and septum, which normalizes on the rest image indicating extensive severe ischemia. 2. Left anterior descending (LAD) coronary artery. 3. Transient cavity dilation. 4. Ventricular tachyarrhythmias, angina-related ST-segment abnormalities, decrease in systolic blood pressure, level of exercise achieved. |
|
|
A 60-year-old man with a history of remote myocardial infarct and CABG surgery. Echocardiography results were normal.
1. Describe the SPECT findings. 2. Provide the differential diagnosis. 3. Give the most likely diagnosis. 4. Explain the discrepancy between the cardiac echocardiogram and the SPECT scan. |
Cardiovascular System: Apical Infarct
1. Fixed stress (str) and rest (rst) severe apical lateral perfusion defect of small size. Heart and cavity size appear normal. 2. Myocardial infarction, apical thinning, attenuation. 3. Small apical lateral scar. 4. Technical factors, operator error, interpretation error. |
|
|
Dual-isotope stress SPECT myocardial perfusion study.
1. Describe the various imaging protocols used for 99mTc myocardial perfusion tracers. 2. What radionuclides are used for a dual-isotope study? 3. List the advantages of the dual-isotope technique compared with a single-isotope study. 4. Describe the SPECT findings and interpret the study. |
Cardiovascular System: Dual-Isotope Study—Mild Inferior Ischemia
1. Two-day stress/rest; same-day rest/stress; same-day stress/rest. 2. Tl chloride for rest; Tc sestamibi or tetrofosmin for stress. 3. The dual-isotope technique requires a shorter time to complete the examination. Wall-motion assessment and gated SPECT are available from Tc perfusion study. Tl can be used to assess viability. 4. Mild decreased inferior wall perfusion at stress with mild improvement at rest. Mild inferior wall ischemia (right coronary artery). (Liver activity on the stress images suggests pharmacological stress. Normal biliary clearance is present on projection images). |
|
|
A 50-year-old woman has atypical chest pain. The exercise treadmill test result with adequate exercise was interpreted as negative. SPECT perfusion images (A, gated short-axis; B, vertical long-axis; C, SPECT wall thickening; D, sequential raw data projection acquisition images) are provided.
1. Describe the SPECT myocardial perfusion image findings and gated SPECT. 2. What information is available from the raw data sequential projection images? 3. What is the most likely diagnosis? 4. List the advantages of electrocardiograph-synchronization (gating) to SPECT. |
Cardiovascular System: Breast Attenuation, Wall Thickening
1. Mild fixed anteroseptal hypoperfusion that demonstrates uniform brightening on gated SPECT, indicating normal myocardial wall thickening on gated images. 2. Apparent decreased radiotracer in the upper portions of the heart is most obvious on the left anterior oblique and lateral frames. No obvious patient motion. 3. Normal perfusion study with normal wall thickening and breast attenuation. 4. Assessment of regional wall motion/wall thickening and left ventricular ejection fraction (LVEF). |
|
|
After the rest scan the patient said he could not stay for the stress study but would reschedule. However, the patient
came to the emergency department the next morning with chest pain. 99mTc sestamibi was injected during the pain, and the images were labeled "stress." 1. Describe the SPECT findings. 2. Name the most likely culprit coronary artery or arteries. 3. Which radiopharmaceuticals are preferred in this setting? 4. Provide the reason for your choice of radionuclide. |
Cardiovascular System: Emergency
Department Chest Pain 1. Moderately severe perfusion defect of the entire anterior wall extending to the apex that partially reverses on rest images, severe perfusion defect of the defect involving the lateral and inferolateral wall that partially reverses. 2. LAD and left circumflex coronary arteries or left main coronary artery. 3. 99nlTc sestamibi or 99mTc tetrofosmin. 4. The exact image timing of 99mTc-labeled agents is not cru cial because no significant redistribution occur. In an emergency setting, matters of patient management and logistics may take priority over immediate scanning. |
|
|
Scans for two patients are provided. A, Stress and 4-hour delayed planar thallium scan. B, Poststress SPECT anterior
raw data projection image. Stress/rest SPECT showed single-vessel ischemia. 1. Describe the planar scintigraphic findings in patient A and the abnormal finding in patient B. 2. What other information is necessary for interpretation of these examinations? 3. Name ancillary findings of CAD other than perfusion defects that are relevant in interpreting myocardial perfusion scans. 4. What is the most appropriate diagnosis in patients A and B? |
Cardiovascular: Planar Thallium with
Increased Lung Activity 1. A, Both ventricles are dilated with prominent right ven tricular uptake. No evidence of ischemia or scar. Increased lung activity on the stress images. 2. The level of exercise achieved. At a low level of stress, the scan can provide false-negative indication of CAD. 3. Poststress lung uptake and transient ischemic dilation. 4. A, Dilated cardiomyopathy with right ventricular hyper trophy. B, Multivessel CAD. |
|
|
A 45-year-old man has dyspnea on exertion. Cardiac catheterization found no coronary disease. Images at end-diastole
(left) and end-systole (right) are shown. 1. Name the radiopharmaceutical, the examination being performed, and describe the findings. 2. Which view is shown, and why was it selected to calculate LVEF? Name other views often obtained. 3. List the terms used to describe myocardial wall motion. 4. Provide a classification for cardiomyopathies. |
Cardiovascular System: Cardiomyopathy on
Equilibrium-Gated Blood Pool Ventriculography or Multigated Acquisition 1. 99mTc-labeled erythrocytes. Equilibrium-gated blood pool ventriculography (RVG) or MUGA (multigated acquisi tion). Frames at end-diastole and end-systole show globally decreased wall motion. Visual estimate shows very decreased LVEE 2. The left anterior oblique view provides the best septal sep aration of the two ventricles. Occasionally anterior and left lateral posterior oblique views also are obtained. 3. Global or regional—akinesis, hypokinesis, dyskinesis, tardokinesis. 4. Classification according to the functional status of the ven tricle: restrictive, dilated, or hypertrophic; or according to cause: alcoholic, infectious, metabolic, toxic, druginduced, or ischemia/CAD, idiopathic. |
|
|
A 45-year-old woman was referred for a ventilation-perfusion study. The perfusion scan only is shown.
1. Describe the abnormal scintigraphic findings. 2. What is the most likely cause for the findings? 3. What is the radiation dose to the patient from a perfusion study? From a 133Xe ventilation study? 4. Given the longer physical half-life and larger administered dose of 133Xe, compared with 99mTc macro-aggregated albumin (MAA), explain the lower resulting radiation dose to the lungs. |
Pulmonary System: "Hot Spots" on Lung Scan
1. Multiple "hot spots" are present in the upper and lower lobes, predominately in the right lung field. 2. Radioactive emboli as a result of poor technique caused by drawing back blood into the syringe containing the 99mTc MAA before injection of the radiotracer, causing clumping. 3. The lungs, the target organs, receive approximately 1 rad/5 mCi from 99mTc MAA. Approximately 0.2 rads to the lung from a 20-mCi xenon study. 4. The biological half-life is brief. The patient breathes 133Xe gas to equilibrium, then expels it into a trap. Only 133Xe absorbed as a result of fat solubility has any appreciable biological half-life. |
|
|
Two patients with the same disease (A and B) had 67Ga scintigraphy.
1. Describe the lung patterns seen on the 67Ga lung scans. 2. What is the finding on the head and neck scan? 3. Match the lung scan with the head and neck scan. 4. What is the disease, and how is 67Ga scintigraphy used in these patients? |
Infection and Inflammation: Sarcoidosis
1. Patient A, "lambda sign" (hilar and paratracheal nodal uptake); patient B, diffuse pulmonary uptake. 2. Classic "panda" sign. 3. Either A or B. The panda sign can be seen at any stage of disease. 4. Sarcoidosis. 67Ga scintigraphy is used to confirm the clini cal diagnosis and to differentiate active alveolitis from inactive fibrosis. |
|
|
A 57-year-old man has had abdominal discomfort and fever for 3 weeks.
1. Describe the findings on this 67Ga study and give a likely diagnosis. 2. What is the mechanism of 67Ga uptake in infection/inflammation? 3. List the photopeaks of 67Ga. List the ones used for imaging. What collimator should be used to acquire the study? 4. What is the recommended administered dose of 67Ga, its half-life, and imaging times? |
Infection and Inflammation: Intraabdominal
Abscess 1. Very increased uptake in the right lower quadrant strongly suggests an intraabdominal abscess. Tumor cannot be excluded. 2. Increased vascular permeability, bacterial uptake, and binding to leukocytes play a role; however, binding to lactoferrin of degranulated neutrophils at the site of infec tion is probably the primary mechanism. 3. Photopeaks occur at 91 to 93, 185, 300, and 394 keV. The lower three photopeaks are used for imaging. A mediumenergy collimator should be used. 4. The recommended adult dose of 67Ga is 5 mCi; the halflife is 78 hours. Imaging at 48 hours is routine. However, if an abscess is suspected, imaging at 6 to 24 hours may provide an early diagnosis. |
|
|
A 9-year-old patient had back pain and fever for 4 weeks. Bone (A), gallium-67 whole-body (B) and abdominal spot
views (C) are shown. 1. Describe the scintigraphic findings on the bone and gallium scans. 2. When both tests are ordered at the same time, which should be performed first? 3. Provide the differential diagnosis and the most likely diagnosis. 4. Based on the available information, characterize the stage of disease. |
Oncology: Bone/Gallium—Stage IV Hodgkin's
Disease 1. The bone scan shows mild increased uptake at L3. The 67Ga scan shows abnormal uptake in the L3 vertebral body, as well as the neck bilaterally (right side greater than the left side), mediastinum, right paratracheal regions, posterior thorax, and right lung base; and multifocal uptake in the liver. The lower-intensity camera setting optimizes liver visualization (C). 2. Bone scan. 3. Hodgkin's disease, tuberculosis, or atypical mycobacteria; Hodgkin's disease is likely. 4. Stage IV. |
|
|
A 32-year-old man has non-Hodgkin's lymphoma. A shows the 67Ga study at initial staging, and B was performed after
a full course of chemotherapy. CT showed a residual chest mass after chemotherapy. 1. What is the adult dose of 67Ga for tumor evaluation? When is imaging performed? 2. Compare the accuracy of 67Ga and CT for initial staging and evaluating response to therapy. 3. Describe the findings of the two studies and interpret them. 4. How can the problem of bowel activity be minimized on 67Ga scans? |
Oncology: 67Ga—Non-Hodgkin's Lymphoma
Before and After Therapy 1. The adult dose is 10 mCi, which is twice the dose used for inflammatory and infectious evaluation. Imaging typically is performed 48 to 72 hours after injection. 2. CT scanning provides better sensitivity for initial staging. 67Ga scanning is superior to CT in evaluation of the effec tiveness of therapy and determination of whether residual masses after therapy represent residual tumor or merely necrosis and fibrosis. 3. A, A large mass in the anterior mediastinum extends to the supraclavicular regions. Considerable colonic/rectal activity is present. Because of the latter activity, tumor cannot be excluded in the mid-pelvis to the lower pelvis. B, Complete response to therapy has occurred. The resid ual chest mass on CT is caused by necrosis and fibrosis, not tumor. 4. Laxatives may be given, and imaging may be delayed as needed at 4 to 7 days after injection. |
|
|
A 67-year-old man has a 2.5-cm left upper lobe lung lesion detected on chest radiographs and confirmed with CT (A).
18F fluorodeoxyglucose positron emission tomography (FDG-PET) scan is shown (B). 1. What percentage of all newly discovered pulmonary nodules are malignant? 2. What percentage of single pulmonary nodules are indeterminate in etiology after chest radiography and CT exami nation? What percentage ultimately are benign? 3. What is the likelihood of lung cancer in this case? 4. What are causes for false-negative/false-positive I8F FDG-PET studies? |
Oncology: FDG-PET—Single Pulmonary Notes
Nodule 1. Only 20% to 30% are malignant overall. However, the incidence is as high as 50% in smokers. 2. By radiographic/CT criteria, 30% to 40% are indetermi nate; 50% percent of these are benign. 3. High. 4. False-negative findings are uncommon and usually are the result of small lesion size (<1.0 cm), bronchoalveolar car cinoma, and carcinoid tumors. False-positive findings can be caused by benign tumor, and inflammatory or infec tious disease, e.g., histoplasmosis, tuberculosis. Typically inflammatory lesions have less uptake than malignant tumors, but overlap exists. |
|
|
A 38-year-old man had a diagnosis of grade I-II astrocytoma and was treated 11 years ago. He has had a recent onset
of seizures. MRI showed no definite change from the many prior studies (B). 1. What FDG-PET scan findings are expected with a low-grade glioma? 2. What is the finding on this FDG-PET scan (A)? 3. Interpret this study. 4. Would 99mTc HM-PAO show a similar appearance? |
Primary Brain Tumor
1. Low-grade gliomas typically have poor or no uptake. 2. Intense uptake in the large temporoparietal mass. 3. Transformation of a low-grade to a high-grade glioma. 4. No. Malignant tumors usually do not have receptors for binding of the radiopharmaceutical, which is necessary before intracellular incorporation. |
|
|
Scintimammography in two different patients; A, a mammographically detected right breast mass; B, a palpable mass
adjacent to a right breast prosthesis. 1. What is the radiopharmaceutical? What is its mechanism of uptake? 2. Describe the imaging findings and give an interpretation. 3. What is the accuracy of conventional mammography and scintimammography for breast cancer? 4. What are causes of false-negative and false-positive findings on scintimammography? |
Oncology: Scintimammography
1. 99mTc sestamibi lipophilicity allows it to enter the cell where it is concentrated in the mitochondrial region related to charge. 2. Patient A has prominent focal uptake in a right breast mass. Patient B has definite focal uptake at the periphery of the breast prosthesis. 3. Accuracy of conventional mammography: sensitivity, 70% to 95%; positive predictive value for cancer, 20% to 30%. Scintimammography multicenter trial: sensitivity/specificity, 75%/83%. Palpable lesion sensitivity, 87%; nonpalpable lesion sensitivity, 71%. 4. Most false-negative findings are in lesions less than 1 cm. False-positive findings occur in fibroadenomas and benign and malignant tumors other than breast cancer. |
|
|
A 53 year-old woman has recent onset of right upper quadrant pain and suspected acute cholecystitis. A, 60-minute
cholescintigraphy. B, 30-minute postmorphine acquisition. 1. Why is morphine used as an alternative to 3- to 4-hour delayed imaging? 2. In a patient with nonvisualization of the gallbladder at 60 minutes, what must be determined before morphine is administered? 3. What is the accuracy of morphine cholescintigraphy? 4. What is the dose of morphine, and how long after injection is the image obtained? |
Hepatobiliary System: Morphine-Augmented
Cholescintigraphy 1. Morphine produces contraction of the sphincter of Odcli, which increases intraluminal common bile duct pressure. Bile and excreted radiotracer then preferentially flow through the cystic duct into the gallbladder if the cystic duct is patent. 2. Exclude drug allergy. Do not give if evidence of common duct obstruction, e.g., delayed filling or clearance of the common duct or delayed biliary-to-bowel transit, exists. 3. The accuracy is at least as good, if not better, than the delayed imaging method. 4. Intravenous administration of 0.04 mg/kg morphine, e.g., 2.4 mg for a 60-kg patient. Images are acquired for an additional 30 minutes. |
|
|
A 53 year-old woman has recent onset of right upper quadrant pain and suspected acute cholecystitis. A, 60-minute
cholescintigraphy. B, 30-minute postmorphine acquisition. 1. Why is morphine used as an alternative to 3- to 4-hour delayed imaging? 2. In a patient with nonvisualization of the gallbladder at 60 minutes, what must be determined before morphine is administered? 3. What is the accuracy of morphine cholescintigraphy? 4. What is the dose of morphine, and how long after injection is the image obtained? |
Hepatobiliary System: Morphine-Augmented
Cholescintigraphy 1. Morphine produces contraction of the sphincter of Odcli, which increases intraluminal common bile duct pressure. Bile and excreted radiotracer then preferentially flow through the cystic duct into the gallbladder if the cystic duct is patent. 2. Exclude drug allergy. Do not give if evidence of common duct obstruction, e.g., delayed filling or clearance of the common duct or delayed biliary-to-bowel transit, exists. 3. The accuracy is at least as good, if not better, than the delayed imaging method. 4. Intravenous administration of 0.04 mg/kg morphine, e.g., 2.4 mg for a 60-kg patient. Images are acquired for an additional 30 minutes. |
|
|
A 43-year-old woman has a low-grade fever and abdominal discomfort 2 days after cholecystectomy.
1. Describe the cholescintigraphic findings. 2. Interpret the study. 3. What are possible causes for this problem? 4. What unique information does cholescintigraphy provide that is not obtainable from other diagnostic imaging procedures? |
Hepatobiliary System: Biliary Leak
1. Rapid bile leakage probably originating from the region of the ligated cystic duct and extending toward the right colonic gutter and with time, over the dome of the liver. 2. Rapid biliary leak. 3. The most common cause is disruption of the cystic duct ligature after cholecystectomy. Other causes for leak include disruption of a surgical anastomosis, blunt or pen etrating trauma, interventional radiographic procedures, tumor, or inflammatory processes. 4. Confirm that fluid collections seen by anatomical imaging modalities are biliary in nature. The rate of leakage also can be estimated. |
|
|
A 59-year-old man is referred with abdominal pain. CT reportedly showed a lesion of uncertain origin in the left lobe of the liver.
1. What is the radiopharmaceutical? What is the study? 2. What are the findings and the likely diagnosis? 3. How large must this lesion be to be seen on planar scintigraphy? 4. What are the advantages/disadvantages and accuracy of the radionuclide study? |
Hepatobiliary System: Cavernous Hemangioma of the Liver
1. Tc-labeled red blood cells (RBCs). RBC liver scintigraphy. 2. Immediate images show no definite abnormality. Delayed images show increased focal uptake in the left lobe consistent with a cavernous hemangioma. 3. At least 2 cm. 4. Very specific (>99%) for hemangioma. Poor sensitivity for small lesions. |
|
|
Two patients undergo studies for gastrointestinal bleeding.
1. What radiopharmaceutical is used? 2. Determine the site of bleeding in study A. 3. Determine the site of bleeding in study B. 4. What is the slowest rate of bleeding that can be detected with scintigraphy and with contrast angiography? |
Gastrointestinal System: 99mTc RBC Colonic
Bleeding 1. 99raTc-labeled RBCs. 2. A, Left colon, rectosigmoid region. 3. B, Right colon, hepatic flexure. It moves rapidly to the left colon. 4. RBC scintigraphy, 0.1 ml/min; contrast angiography (1.0 ml/min). |
|
|
A 5-year-old girl is referred after passage of a bloody stool.
1. What is the radiopharmaceutical, its mechanism of uptake, and study type? 2. Which pharmacological drugs can be used to enhance detectability? What is their mechanism? 3. Provide an interpretation. 4. Why is bleeding a common complication of this disease entity? |
Gastrointestinal System: Meckel's
Diverticulum 1. 99mTc pertechnetate Meckel's scan. The radiopharmaceutical is taken up and secreted by gastric mucosa. 2. Pentagastrin increases rapidity, intensity, and duration of uptake. It is used with glucagon, which has an antiperistaltic effect that inhibits the rapid dispersion effect of pentagastrin. Cimetidine, a histamine antagonist, increases and prolongs uptake because of inhibition of 99mTc pertechnetate secretion from gastric mucosal cells. It is commonly used because of its lack of side effects. 3. Increasing focal uptake in the mid-abdomen suspicious for Meckel's diverticulum; however, atypical timing of uptake lessens the certainty. The uptake should be coincident with gastric uptake in cases of Meckel's diverticulum. This may be a false-positive scan. 4. Acid and pepsin secretion by the gastric mucosa produces inflammation and ulceration of adjacent bowel mucosa. |
|
|
A patient with insulin-dependent diabetes has chronic symptoms of early satiety, postprandial bloating, and abdominal
discomfort. A gastric emptying study is conduct 90 minutes after a solid meal. 1. What is the diagnosis? 2. What are normal values for solid meal gastric emptying? 3. What is the advantage of a solid radiolabeled meal over a liquid meal? 4. Why is attenuation correction recommended for accurate quantification of gastric emptying? |
Gastrointestinal System: Diabetic Gastroparesis
1. Consistent with severe diabetic gastroparesis. Obstruction cannot be ruled out. 2. Normal values are meal specific and depend on its volume/composition, the method of acquisition, attenua tion correction, processing, and quantification. Normal values must be determined in each clinic or results of a published method should be followed closely. 3. Solid (meat) or semisolid (egg) gastric emptying meals are more sensitive for detection of mild to moderate delay in emptying than studies conducted after a liquid meal. 4. Activity is detected with greatest efficiency close to the cam era. The anterior view alone underestimates emptying, and the posterior view overestimates it because of variable atten uation as the meal moves through the stomach from the posterior gastric fundus to the more anterior gastric antrum. |
|
|
A 3-month-old infant was referred with symptoms of gastroesophageal reflux. A radionuclide gastroesophageal reflux
study (milk study) was performed (posterior view). 1. What are common symptoms and problems in children associated with reflux? 2. What other method is used by pediatricians for detection of reflux? 3. What radiolabel and what meal is used for this study? 4. How frequently should images be acquired to maximize sensitivity of this test? |
Gastrointestinal System: "Milk" Study—
Gastroesophageal Reflux 1. Vomiting, pulmonary symptoms, asthma, pneumonia, sudden death, failure to thrive, anemia. 2. 24-hour pH monitoring. 3. 99mTc sulfur colloid (1 mCi) in the child's usual feeding, formula, or milk. 4. 5 to 10 seconds/frame. |
|
|
A 65-year-old man with recent acute onset of right-sided hemiparesis undergoes 18F FDG-PET scanning.
1. What is the radiopharmaceutical used for metabolic cerebral imaging with PET, and what is the mechanism of uptake? 2. What are the radiopharmaceuticals used for PET cerebral perfusion imaging? 3. Describe this patient's PET imaging findings (above, transverse; middle, sagittal; bottom, transverse)? 4. What is the differential diagnosis? |
Central Nervous System: Cerebral Infarct
1. 18F PET-FDG is dependent on glucose metabolism. 2. SPECT 99mTc HM-PAO and ECD are cerebral perfusion agents that are lipid soluble, distribute according to cerebral blood flow (gray to white matter, 3:1 to 4:1), and fix intracellularly. 3. Wedge-shaped severe decreased metabolism in the left posterior parietal region in a vascular posterial parietal distribution. 4. Cerebral hemorrhage, infarct, and neoplasm. |
|
|
A 45-year-old woman with cervical carcinoma has new bilateral hydronephrosis demonstrated on CT scanning.
1. Describe the scintigraphic findings before and after furosemide administration. 2. Interpret the study before laser administration. 3. Interpret the study after laser administration. 4. List some limitations of diuretic renography. |
Diuretic Renography: Unilateral Obstruction
1. Good symmetrical cortical uptake and prompt excretion into collecting systems bilaterally. Retention of activity in left renal collecting system, apparent cutoff in the upper ureter, and very poor response to furosemide. The right side shows a prominent collecting system but washes out spontaneously before furosemide administration. 2. Hydronephrosis of the left kidney. Rule out obstruction. 3. Consistent with significant obstruction of the left kidney. 4. Dehydration, renal insufficiency, inadequate diuretic dose, full bladder, large collecting system. |
|
|
A 5-year-old girl has had two urinary tract infections in the past 6 months.
1. Which radiopharmaceuticals commonly are used for cystography? 2. What is the advantage of radionuchde cystography over the contrast study? 3. What is the difference between indirect and direct radionuclide cystography? 4. How is reflux graded with radionuclide cystography? |
Radionuclide Cystography
1. 99mTc DTPA and WmTc sulfur colloid are the two most commonly used. 2. Radionuclide cystography is more sensitive in detection of vesicoureteral reflux (VUR) and results in 50 to 200 times less radiation exposure to the gonads compared with the contrast study. 3. The direct method is commonly used and requires urinary catheterization and instillation of radiotracer into the bladder through a catheter. The indirect method is performed after routine renography with 99mTc DTPA/mercaptylacetyltriglycine (MAG3). When the bladder is full, a prevoiding image is obtained, followed by dynamic images during and after voiding. 4. Grading criteria are similar to those used with contrast cys tography; however, the radionuclide study's limited resolu tion does not permit assessment of calyceal morphology. Mild reflux: confined to the ureter. Moderate: reaches the pelvicocalyceal system. Severe: distorted collecting system and dilated tortuous ureter. |
|
|
A 35-year-old renal transplant patient has three renal studies (sequential images over 30 minutes) using 99mTc DTPA
on one day and 99mTc MAG3 and 13II hippuran 1 week later. 1. Which renal radiopharmaceutical is used for each study: A, B, and C? 2. What is the mechanism of uptake of the three radiopharmaceuticals? 3. What are the advantages and disadvantages of each radiopharmaceutical? 4. Can a blood flow (radionuclide angiogram) study be done with all three agents? Why? |
Renal Radiopharmaceuticals
1. A, 99mTc DTPA; 5, 99mTc MAG3; C, I31I hippuran. 2. DTPA: glomerular filtration; MAG3: tubular secretion; hippuran: 20% glomerular, 80% tubular. 3. DTPA is inexpensive, provides a good image quality, but has low extraction efficiency (10% to 20%) and poor quality images with renal insufficiency. MAG3 has a high extraction rate (60%), good target to background, and good-quality images with renal insufficiency. Hippuran has good extrac tion efficiency, high target-to-background, poor image qual ity, poor cortical/collecting system differentiation, and deliv ers a high radiation dose in renal insufficiency. 4. No. The administered dose of 131I hippuran is too low (200 to 300 |xCi), limited by the high radiation absorbed dose. A dose of 5 mCi is needed for good blood flow images. |
|
|
A 31-year-old man with a history of congenital ureteropelvic junction obstruction had surgical correction several years
ago. The most recent diuretic renogram was interpreted as right renal obstruction. This scan was obtained after the second surgical correction. 1. Describe the scintigraphic imaging findings before and after administration of furosemide. 2. What is your interpretation of the study? 3. Can ureteropelvic vs. ureterovesical obstruction be distinguished from this study? 4. What is the Whittaker test? |
Genitourinary System: Diuretic
Renography/Nonobstructed Hydronephrosis 1. Bilateral prompt cortical uptake and excretion into collecting systems. Retention in the right collecting system at 30 min utes with good post-furosemide washout. 2. Good response to surgical correction. Negative for obstruction. 3. Not with certainty. Ureteral nonvisualization is not diagnos tic of ureteropelvic junction obstruction because a standing column of ureteral urine can prevent radiotracer entry. 4. It measures pressure-flow relationships and requires fluoroscopically guided trocar or spinal needle insertion into the renal pelvis. Basal and pressure measurements during infu sion of a contrast solution at a set rate are recorded. Obstruction pressure is defined as greater than 15 cm water, no obstruction as less than 10 to 12 cm water. |
|
|
A 30-year-old kidney transplant recipient has decreasing postoperative urine output, fullness and tenderness around
the graft, and scrotal swelling 24 hours after surgery. 1. Describe the findings on the 25-minute dynamic renal scintigraphy. 2. What is the diagnosis? 3. What are other causes of postoperative fluid collections adjacent to the graft? 4. What are other common complications during the first weeks after transplantation? |
Genitourinary System: Transplant Kidney
Urinary Leak 1. Rapid leakage of urine just inferior to the transplanted lcidney and extravasating into the scrotum. 2. Urinary leak caused by disruption of the surgical anastomosis. 3. Hematomas and abscesses occur in the early postoperative course, whereas lymphoceles generally are noted 4 to 8 weeks after surgery. 4. Acute tubular necrosis, acute rejection, obstruction. Cyclosporin toxicity usually occurs months after transplantation. |
|

Radionuclide blood flow and early dynamic images at 24 hours after transplantation.
1. What are the scintigraphic findings? 2. What is your physiologic interpretation? 3. What is the differential diagnosis? 4. What therapy would be appropriate |
Genitourinary System: Nonviable Kidney After
Transplantation 1. No blood flow to the transplanted kidney. No renal uptake. A photopenic region in the shape of the trans planted kidney. 2. Nonviable kidney. 3. Arterial or venous thrombosis, severe irreversible rejection, acute cortical necrosis. 4. Removal of the nonviable transplanted kidney. |
|
|
A 25-year-old man undergoes imaging 3 days after a renal cadaver transplant.
1. Which postoperative complications occur in the first week of renal transplantation? 2. During which postoperative period does acute rejection typically occur? 3. What are the scintigraphic findings in this case? 4. What is the diagnosis? |
Genitourinary System: Renal Transplant with
Acute Tubular Necrosis 1. Acute tubular necrosis, accelerated acute rejection, urinary leak, urinary obstruction. 2. The second postoperative week. Accelerated rejection may occur during the first week in patients who have had previ ous transplants or received multiple transfusions. 3. Normal blood flow, very poor function, no excretion. Base of penis seen inferiorly. 4. The pattern of normal blood flow but poor function dur ing the first week after transplantation is typical of acute tubular necrosis (ATN). |
|
|
An 8-year-old boy has acute onset of right testicular pain.
1. What is the radiopharmaceutical and mechanism of distribution? 2. What are the most common causes of acute testicular pain? 3. What is the mechanism of testicular torsion? 4. What are the imaging findings, and what is the diagnosis in the case? |
Genitourinary System: Testicular Torsion
1. 99mTc pertechnetate, initial blood flow, and then the radiotracer distributes in the extracellular fluid space (intravascular and interstitial). 2. Actite epididymitis, testicular torsion, torsion of the testic ular appendage. 3. Developmental abnormality of testicular descent and attach ment predisposes to spermatic cord torsion. The most com mon anatomical abnormality is "bell-clapper" testis. 4. Decreased blood flow to the right testicle and a photopenic right testicle consistent with acute testicular torsion. |
|
|
A 48-year-old woman has recent onset of neck tenderness and hyperthyroidism (thyroid-stimulating hormones [TSH]
<0.05 |xU/ml); 123I scan uptake (radioactive iodine uptake [RAIU]) <1%). Right side (R); suprasternal notch (SSN). 1. What is the clinical differential diagnosis of hyperthyroidism? 2. What is the clinical purpose of the thyroid scan and RAIU tests in hyperthyroidism? 3. How is the RAIU calculated? 4. What is the likely diagnosis in this patient? |
Endocrine System: Hyperthyroidism/
Thyroiditis 1. Graves' disease, toxic nodule(s), thyroiditis (subacute, silent, postpartum), iatrogenic thyroid hormone ingestion, iodine-induced (Jod Basedow), trophoblastic tumors (hydatidiform mole and choriocarcinoma), Hashitoxicosis, ectopic hyperfunctioning thyroid tissue (struma ovarii). 2. Aid in the differential diagnosis of hyperthyroidism. 3. A nonimaging gamma probe obtains counts/time from the neck and a phantom-containing activity equal to the orally administered dose (u,Ci) to convert the gamma probe counts to |JiCi. %RAIU = neck (|xCi) divided by the total administered dose (|xCi) after background correction. 4. Subacute thyroiditis based on the history of neck tender ness, laboratory finding, and RAIU. |
|
|
A 35-year-old woman with hyperthyroidism. Radioactive iodine uptake was 94% at 4 hours and 81% at 24 hours.
1. Describe the difference between Graves' disease and euthyroid scan appearance. 2. What is the appropriate therapy for Graves' disease? 3. What are the usual administered doses of radiotracer for "'I uptakes, 123I scans, and Graves' disease therapy? 4. What are the short-term and long-term side effects of 131I therapy for hyperthyroidism? |
Endocrine System: Graves' Disease
1. Scan appearance may be similar. With a large goiter the scan often has a plumper appearance with convex borders. The pyramidal lobe may be seen, as in this case. 2. Surgery is seldom performed because of the high risk. Propylthiouracil (PTU) and methimazole (Tapazole) sometimes are used initially, particularly in patients with severe disease who require "cooling down," young chil dren, and pregnant patients. Most of these are treated with radioactive iodine after 6 to 12 months of antithyroid medication. Many patients are treated initially with 131I. 3. 131I uptake (10 (xCi), 123I scan and uptake (300 |xCi), Graves' disease therapy: 131I (5 to 15 mCi) 4. Short-term: occasional exacerbation of hyperthyroidism, cardiac symptoms in elderly, very rare thyroid storm. Long-term: hypothyroidism. There is no increased inci dence of secondary cancers, reduction in fertility, or con genital defects in offspring. |
|
|
A 39-year-old woman 6 weeks previously underwent total thyroidectomy for thyroid cancer. Scanning was done 7 days
after therapy for thyroid ablation with 75 mCi of 131I. 1. Describe and interpret the scintigraphic images. 2. What is the reason for the star artifact pattern in the neck in scan A? 3. What collimator was used for image B? 4. Why is the liver seen in image A? |
Endocrine System: 131I Star Artifact
1. A, Posttherapy I31I whole-body scan shows intensive uptake in the neck with a "star" artifact, diffuse liver activity, and bladder clearance. The mediastinum is difficult to visualize because of the artifact. B, Pinhole image of the neck with three foci of uptake. 2. Septal penetration of high-energy 131I gamma rays through the collimator septa. 3. Pinhole collimator centered on the thyroid. 4. Radiolabeled thyroid hormone is metabolized in the liver. This usually is seen only on the posttherapy scans. |
|
|
A 12-year-old boy has recent onset of back pain. The report of outside radiographs was equivocal.
1. Describe the bone scan findings on the planar images (A) and reprojection SPECT (B) images. 2. Describe the findings on the transverse and coronal SPECT slices (Cand D). 3. Provide a differential diagnosis and the most likely diagnosis. 4. This entity may be associated with an abnormality of alignment. Describe it. |
Skeletal System: L5 Pars Interarticularis Defect
1. The bone scan demonstrates focal increased uptake in the lateral aspect of L5 vertebra. 2. The finding is better demonstrated and better localized on the SPECT images, where the abnormal uptake is clearly seen in the region of the left pars interarticularis/facet joint. 3. L5 unilateral pars interarticularis defect, degenerative or posttraumatic facet disease. Pars defect is the most likely diagnosis in this age group. 4. Spondylolisthesis or slippage of the vertebrae out of nor mal alignment can occur if the defect is bilateral. |
|
|
A 5-year-old boy with low-grade fever and pain in the right knee was referred for a three-phase bone scan.
1. Describe the three-phase scintigraphic findings. 2. Provide a differential diagnosis. 3. Do these findings suggest a septic arthritis? 4. What other radionuclide study could confirm or exclude infection? |
Bone: Tibial Osteomyelitis—Three-Phase
Positive Bone Scan 1. Increased blood flow (A), blood pool (B), and uptake on delayed images (C) in the proximal metaphyseal region of the right tibia. 2. Osteomyelitis, bone tumor, fracture/osteotomy. 3. No. A bone scan with septic arthritis shows increased uptake at the end of long bones symmetrically on both sides of the joint. An asymmetrical appearance may be seen if osteomyelitis and septic arthritis coexist; however, this study reveals normal findings on the femoral side. 4. 99mTc HM-PAO-labeled leukocyte study in a child. |
|
|
An 11-month-old infant has a hepatic mass on ultrasound. Bone scan ordered to exclude bone metastases.
1. Describe the scintigraphic findings. 2. Besides a neoplastic process, what other conditions could be associated with the findings? 3. Name another likely origin of the tumor other than the liver. 4. What is the most likely diagnosis? |
Skeletal System: Hepatoblastoma
1. Nonuniform abnormal soft tissue right upper quadrant up take that cannot be clearly separated from the right kidney. 2. Trauma to soft tissue or organs, in this case, the liver, resulting in contusion or hematoma, ischemic injury (although the pattern appears round rather than suggestive of a vascular distribution), chronic abscess. 3. Adrenal: neuroblastoma. 4. Given that it is a hepatic mass, hepatoblastoma is most likely based on the patient's age and uptake of bone radiotracer. |
|
|
Two patients have knee pain, with no fever or calor. Patient A: bone scan and radiograph. Patient B: bone scan.
1. Describe the abnormal three-phase bone scan findings for patients^ and B. 2. What other general information about the patients is evident from the bone scans? 3. Provide a differential diagnosis and the most likely diagnoses for each patient. 4. What term is commonly used to describe the pattern seen on delayed images in B? |
Skeletal System: Osteosarcoma
1. A, Increased blood flow (above) and blood pool (below, left) to the right distal femur and increased uptake on delayed images in the distal femoral metaphysis extending to the joint surface (below, right). Mild increased uptake in die proximal tibia probably the result of hyperemia. B, Radio graph: mixed lytic-sclerotic lesion of die distal femur with cortical destruction and indistinct margins. No periosteal reaction. C, Abnormal increased flow and blood pool to die left distal femur with delayed increased uptake in spiculated pattern extending beyond the femoral contour. 2. The patients are skeletally immature but near the mature stage. Physes are seen faintly on delayed images, indicating that fusion is imminent. These are teenagers. 3. A, Monostotic primary neoplasm, e.g., osteosarcoma, sec ondary neoplasm, or osteomyelitis. B, Characteristic sun burst pattern of osteosarcoma. 4. Sunburst pattern. |
|
|
Two young adults were referred for a bone scan. Patient A has thoracic pain, and patient B has hip pain.
1. Describe the scintigraphic findings in both patients. 2. What is the diagnosis and cause for this pattern of uptake in these patients? 3. What is the mechanism of radiopharmaceutical uptake? 4. What are other causes of uptake in muscle? |
Skeletal System: Muscle Injury
1. A, Uptake in teres major muscles bilaterally. B, Bilateral uptake in the adductor magnus muscles of the thighs. 2. Soft tissue muscle injury caused by repetitive stress; weight lifting in A, and stair climber exertion in B. 3. Soft tissue deposition of 99mTc-labeled diphosphonates is caused by binding to microcalcifications at sites of injury and possibly binding to injured immature collagen. 4. Rhabdomyolysis, iron dextran injection, polymyositis, myositis ossificans, ischemia, electrical injuries, direct trauma. |
|
1. Describe the bone scan findings.
2. Name structures where the tracer could be deposited. 3. Provide the differential diagnosis. 4. What other information would be helpful? |
Skeletal System: Pleural Uptake
1. Abnormal soft tissue uptake in the anterior left hemithorax; scoliosis and mild arthritic changes in both hips. 2. Starting on the inside working outward: in the lung parenchyma, in a primary or secondary tumor in the lung, in the pleural or pleural effusion, in the soft tissue of the chest wall. 3. Extensive pleural calcification, fibrothorax, prior radiation. 4. History, chest radiograph, or SPECT. |
|
|
1. What are possible explanations for the change in the patient's bone scan from A to B?
2. List three questions that would be helpful to limit the differential diagnosis in A/B. 3. Describe the bone scan findings in patient C. Ignore the rectangular region of interest. 4. Provide the most likely diagnosis for the scans A/B and C. |
Skeletal System: Hot Kidneys, Radiation
Nephritis, and Spinal Photopenia 1. Increased radiotracer is present in both renal cortices in a bilateral symmetrical pattern on the follow-up study that was not seen on the initial study. 2. Has the patient been treated with a new medication in the interval since the prior bone scan? Has the patient had recent intravenous contrast media? Has the patient had restricted fluid intake? 3. Increased activity in the upper portions of both kidneys and cold lower thoracic spine. 4. A/B, Chemotherapy-induced interstitial nephritis. C, Prior radiation therapy to the spine with radiation nephritis. |
|
|
1. Describe the advantage of whole body imaging for the technologist compared with spot imaging, which was used
in this case. 2. Describe the advantage of whole body imaging for the physician. 3. Describe the abnormality 4. Provide the differential diagnosis. |
Skeletal System: Splenic Uptake
1. Less camera repositioning and time for the technologist. 2. Easier for the physician to check for quality assurance and for interpretive review. 3. Intense abnormal uptake in a structure that appears to be an enlarged spleen by its location and configuration. 4. Blood dyscrasias, including siclde cell disease, sickle thalassemia, thalassemia major; hemosiderosis; extensive subcapsular splenic hematoma. |
|
|
The bone scan image and radiograph of a paraplegic patient are provided.
1. Describe the bone scan findings. 2. Provide a differential diagnosis. 3. What interventions could be performed if artifact is suspected? 4. Radiograph of the right hip was obtained after the bone scan. What is the most likely diagnosis? |
Skeletal System: Heterotopic Ossification
1. Radiotracer in a full urinary bladder obscures the central portion of the bony pelvis. Intense activity is seen overlying the right acetabulum with a separate area of uptake overlying the proximal right femur. 2. Urinary contamination; fracture with exuberant callus; heterotopic ossification or myositis ossificans; soft tissue injury (contusion). 3. If urinary contamination is suspected: remove clothing and overlying bed sheets; wash the patient's skin in the area of suspected contamination. 4. Heterotopic ossification. |
|

Elevated alkaline phosphatase level.
1. Describe the bone scan findings. 2. Name two other nonosseous systems that should be evaluated on the bone scan. 3. Describe any other findings. 4. What term can be applied to this case? |
Skeletal System: Superscan Secondary to
Metastatic Prostate Cancer 1. Increased radiotracer in the large majority of the visualized bones, with nonuniform involvement particularly evident in both femurs, both humeri, and skull. 2. Soft tissues and genitourinary tract. 3. The kidneys are not visualized, but faint activity is seen in the urinary bladder. Little soft tissue activity is seen. 4. Superscan. |
|
|
A 56-year-old was admitted after a seizure and fall. Brain CT demonstrates multiple cerebral masses. Whole body bone
scan (A) and multiple transverse SPECT images of the chest (B) are shown. 1. Describe the skeletal abnormalities. 2. Describe any other abnormalities. 3. What is the most likely diagnosis? 4. Name 3 liver primary or metastatic tumors that have increased bone tracer uptake. |
Skeletal System: Soft Tissue Uptake
in Lung Mass 1. Focal abnormal uptake in the right and left anterior ribs, right upper posterior rib, and sternum. 2. Abnormal diffuse radiotracer uptake in the right upperchest on the anterior and posterior views, which does not conform to normal bone configuration. Selected SPECT images demonstrate the uptake to be in a large ovoid mass within the right lung. 3. Lung cancer with brain metastases. The bone scan abnor malities are likely traumatic because of the distribution and history of a fall. 4. A high percentage of neuroblastomas involving the liver have bone tracer uptake, and a much smaller percent of metastases from lung, breast, and colon cancer, especially mucinous cancers. |
|
|
A 55-year-old man has low back pain and no prior history. Bone scan images, anterior and posterior views.
1. Provide a general distribution for the bone abnormalities. 2. Describe the findings. 3. List three factors that help limit the differential diagnosis. 4. What is the most likely diagnosis? |
Skeletal System: Prostate Cancer Bone
Metastases, Axial Distribution 1. Spine and pelvis. 2. Abnormal focal and regional activity is seen in multiple sites in the sacrum, both ilium, both inferior pubic rami, right superior pubic ramus, mid-thoracic and lower thoracic spine. Note the incidental calcification of costochondral cartilage. 3. Multiple lesions, axial predominance, older adult man. 4. Multiple skeletal metastases from prostate cancer. |
|
|
A 53-year-old woman with hypercalcemia was referred to rule out metastatic bone disease.
1. Describe the bone scan findings. 2. Give a differential diagnosis. 3. Provide the most likely diagnosis. 4. Could this pattern be caused by free 99mTc pertechnetate? Why? |
Skeletal System: Hyperparathyroidism
1. Abnormal diffuse uptake in the lungs and stomach. Poor visualization of small kidneys and bladder, increased uptake in the shoulders, hips, knees, and ankles. 2. Hyperparathyroidism, metastatic calcification caused by hypercalcemia, renal failure or both, metabolic bone disease. 3. This particular pattern of metastatic calcification is charac teristic of long-standing hyperparathyroidism. Although other causes of metabolic bone disease, e.g., osteomalacia and renal osteodystrophy, result in abnormal bone scans, they do not have this characteristic pattern. This scan pattern is seen in hyperparathyroidism. 4. Free 99mTc pertechnetate has gastric, thyroid, and salivaty gland uptake. The latter two are not seen in this patient, who also shows large uptake. |
|
|
An initial bone scan (A) and repeat study 2 years later (B).
1. Describe the bone scan abnormalities on the initial study (A). 2. Describe the skeletal abnormalities on the follow-up study (B). 3. List the differential diagnoses. 4. Provide the most likely diagnosis. |
Bone: Osteosarcoma Metastatic to Lung
1. A, Abnormal decreased and increased uptake in the left humerus (proximal and mid, respectively). 2. B, Irregular uptake in the chest anterior and posterior views indicates location midway between in the lung parenchyma. Uptake is nodular and masslike. Rib abnor malities cannot be excluded, but the pathological condi tion extends across the rib spaces. Left shoulder arthroplasty is shown by photopenia. 3. The differential diagnosis for abnormal lung activity in a focal pattern includes primary lung tumors and metastases, especially for tumors with calcific or ossific components. For abnormal lung activity in a regional pattern, not evi dent in this case, the differential diagnosis includes malig nant pleural effusion, fibrothorax, or radiation therapyinduced pneumonitis. 4. Osteosarcoma of the left proximal humerus, status/ post-arthroplasty, with lung metastases. |
|
|
Diffuse upper extremity pain was noted 3 months after thoracotomy. Hand radiographs show normal findings. The remainder of the bone scan is normal.
1. Describe the scintigraphic bone scan findings in this case (palms down on the camera). 2. Provide the differential diagnosis. 3. What is the likely diagnosis in this case? 4. Discuss the pathogenesis. |
Skeletal System: Reflex Sympathetic
Dystrophy 1. Three-phase study demonstrates abnormal increased blood flow and blood pool of the distal right upper extremity. The delayed bone phase shows increased activity in the bones in the same distribution, with a striking increase in periarticular activity causing the joints to stand out. 2. Reflex sympathetic dystrophy syndrome (RSDS), disuse of a limb of new onset, e.g., recent stroke or immobilization by orthopedic cast or splint. 3. Shoulder-hand syndrome, a frequently encountered form of RSDS. 4. Neurogenic origin with loss of sympathetic autonomic tone is the generally accepted explanation, although not firmly established. |
|
|
An elderly patient has had right knee pain for 3 months. Radiographs at onset were reported as normal.
1. Describe the bone scan findings. A, above: flow; A, below: blood pool and delayed images. 2. Based on the scan findings, provide a differential diagnosis. 3. A radiograph then was obtained (B). Given all available information, what is the most likely diagnosis? 4. What are common causes for this condition in the femoral head? |
Skeletal System: Spontaneous Osteonecrosis
of Distal Femur 1. Increased activity in the medial femoral condyle on all three phases of the bone scan. 2. Osteonecrosis, fracture, osteoarthritis, primary bone neo plasm (unlikely with prior normal radiograph). 3. Spontaneous osteonecrosis of the medial femoral condyle. 4. Trauma, steroid therapy, vasculitis, infarction (siclde cell, Gaucher's disease), alcoholic, caisson disease. |
|
|
A patient has back pain and elevated serum alkaline phosphatase concentration.
1. What is the mechanism of uptake of bone scan agents? 2. Describe the bone findings. Describe any other soft tissue findings. 3. What is the most likely diagnosis? 4. List three possible primary neoplasms. |
Skeletal System: Metastases to Bone and Liver
1. Uptake is dependent on blood flow and adsorption to the hydroxyapatite crystal. 2. Abnormal focal uptake in the skull, scapulae, ribs, spine, pelvis, and left femur. Diffuse uptake in the majority or entire liver. 3. Malignant metastases to bone and liver. 4. Breast, colon, lung. |
|
|
A bone scan was ordered because an elderly man "hurts all over." The remaining bone scan (not shown) was otherwise
normal. 1. Describe the 99mTc disphosphonate bone scan findings. 2. In terms of anatomical location, where is the abnormal radiotracer uptake? 3. What other radiopharmaceutical would give a similar appearance? 4. What is the differential diagnosis? |
Skeletal System: Myocardial Uptake
1. Curvilinear "horseshoe" pattern of uptake in the anterior chest that does not correspond to normal bony anatomy and therefore is most likely abnormal soft tissue uptake. 2. Cardiac uptake, either the myocardium or pericardium. 3. 99mTc pyrophosphate. 4. Idiopathic or secondary cardiomyopathy, e.g., due to cardiotoxic drugs, myocarditis, cardioversion injury, myocar dial contusion, ventricular aneurysm, infarction, severe unstable angina, pericarditis with or without calcification, amyloidosis. |
|
|
Patient has known breast cancer metastatic to bone. Initial bone scan (A) and scan 6 months later (B and C) are submitted.
1. Describe any interval change. 2. Describe the findings in C. 3. Where is the skull abnormality most likely located? 4. What is the most likely explanation? |
Skeletal Metastases: Metastasis to Clivus
1. Increased intensity of activity is seen in the nasal region on the anterior view and midline occiput on the posterior view and left sixth and seventh costochondral junctions and left radial head uptake (not injection site). 2. The skull abnormally increased activity projects over the temporomandibular joint region on the right and left lateral skull images. 3. Skull base in the midline. 4. Metastasis to clivus; other skeletal metastases appear stable. |
|
|
Two patients are shown. ^4, A 10-year-old boy was referred for a bone scan because of back pain. B, A 60-year-old man
with new lung cancer. Bone scan and CT scan are provided. 1. Describe the bone scan findings in both patients. 2. Give a differential diagnosis for these abnormalities. 3. Describe the extraosseous soft tissue abnormality in B. 4. What are the two most likely causes for the soft tissue abnormality? |
Skeletal System: Cold Spine Defects
1. A, Cold defect in Tl 1. B, Decreased activity at approxi mately T6. 2. Benign or malignant tumor, osteomyelitis, avascular necro sis, congenital or surgical defect, artifact, radiation therapy. 3. Intense renal cortical uptake (cortical staining). 4. Nephrotoxic antibiotics or chemotherapeutic agents asso ciated with interstitial nephritis. |
|
|
A patient has abnormal blood chemistry test results. Selected images from a bone scan are submitted printed in normal
and dark modes. 1. Describe the findings. 2. Name two features that help to narrow the diagnosis. 3. List other findings outside the chest that can help to narrow the differential diagnosis. 4. Provide the most likely diagnosis. |
Skeletal System: Metastatic Calcification in
Lungs and Kidneys 1. Abnormal bilateral lung activity; increased activity in the renal parenchyma; kidneys appear enlarged. 2. The findings are bilateral and uniform. Two different organs are involved. 3. Tracer uptake in the stomach would suggest hyperparathyroidism. 4. Metastatic calcification caused by hypercalcemia associated with renal insufficiency. |
|
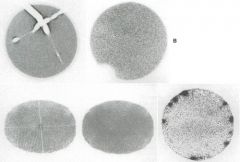
Provide the probable cause and give your recommendations for the abnormal gamma camera quality control floods.
1. A. 2. B. 3. C. Overnight change. 4. D. Change since prior patient that day. |
Quality Control: Gamma Camera Floods
1. Cracked crystal (buy a new crystal). 2. Nonfunctioning photomultiplier tube (call service). 3. Distorted (not circular) and nonuniform image. Electronic tuning required. The power went off overnight. Call the service representative. 4. Contamination of crystal with radiopharmaceutical. (Clean camera or allow radiotracer to decay 10 half-lives.) |
|
|
A 50-year-old patient with diabetes achieved 4.0 METS (metabolic equivalent) and 60% of maximum age-predicted
heart rate (MPHR) on the exercise treadmill stress test. 1. When should the exercise treadmill stress test be discontinued? 2. Describe the myocardial stress and rest perfusion SPECT image findings. 3. Provide the differential diagnosis and likely involved vessel(s). 4. Discuss any other factor important to the interpretation of the scan. |
Cardiovascular System: Inferior Lateral
Wall Infarction 1. If the patient develops severe anginal chest pain, a decrease in blood pressure, frequent premature ventricular contrac tions (PVCs), or ST-T wave elevation suggestive of acute infarct. Also if the patient can walk no further on the treadmill because of general fatigue, leg pain, or dyspnea. 2. Severe stress and rest fixed defect in the basal lateral, inferior, and inferolateral walls, sparing the apex. 3. Myocardial infarction or possibly hibernation. Circumflex artery. 4. The exercise stress level. |
|
|
A 53-year-old man who had a recent myocardial infarction had a dipyridamole stress myocardial SPECT study before hospital discharge. SPECT short-axis (A) and vertical long-axis (B) images are shown.
1. Describe the SPECT findings. 2. Name the likely coronary artery or arteries involved. 3. Provide the differential diagnosis. 4. What prognostic information does the scan provide? |
Cardiovascular System: Dipyridamole-lnduced Reversible Inferior Wall Ischemia
1. A perfusion defect involving the entire inferior wall extending to the apex shows partial reversibility. 2. Right coronary artery. 3. Inferior wall ischemia with incomplete reversibility. The latter may represent scar (infarct) or hibernating myocardium. 4. The patient is at risk for a further cardiac event, either myocardial infarct or death. |
|
|
SPECT adenosine stress/rest myocardial perfusion images. SPECT short-axis (A), vertical long-axis (B), and horizontal long-axis (C) images are shown.
1. Describe the procedure for adenosine stress (a), adenosine's duration of action (b), and the procedure to deal with side effects of adenosine (c). 2. List contraindications to the use of intravenous adenosine. 3. Describe the SPECT findings and the diagnosis. 4. What are clinical indications for adenosine stress? |
Cardiovascular System: Adenosine Stress/
Apical Infarct, Anterior-Lateral Ischemia 1. (a) Adenosine is infused intravenously for 6 minutes (140 |xg/kg/min). After 3 minutes the radiotracer is injected and adenosine is continued for 3 more minutes, (b) Adenosine is cleared rapidly from the circulation (tj, <10 seconds). Return to baseline blood flow levels occurs in 2 to 3 minutes after stopping the infusion, (c) Stop the infusion. 2. Sinus node disease, second- or third-degree atrioventricular (AV) block, bronchospastic lung disease, adenosine allergy. 3. Small to moderately severe fixed defect at the apex on both stress and rest images consistent with infarct. Mildly improved perfusion of the anterior and lateral walls at rest compared with stress consistent with mild anterolateral ischemia. 4. Whenever adequate exercise stress is not possible. |
|
|
A 55-year-old man with CAD but no history or ECG evidence of myocardial infarction. SPECT short-axis (A), vertical long-axis (B), and horizontal long-axis (C) are shown.
1. Describe the findings on the SPECT. 2. Provide the differential diagnosis. 3. Describe the blood flow and functional state of hibernating myocardium. 4. Describe the blood flow and functional state of stunned myocardium. |
Cardiovascular System: Viability,
Fixed LAD Defect 1. Extensive fixed defects involving the anterior wall, apex, septum, extending to the lateral wall. 2. Myocardial infarction versus hibernating myocardium 3. In hibernating myocardium, blood flow and function, e.g., contractility, are chronically reduced. 4. Blood flow is normal, recently restored after an acute occlusive state; function is reduced. |
|
|
1. Describe the bull's-eye format for SPECT myocardial perfusion studies.
2. List possible errors that may occur when applying a bull's-eye quantitative analysis technique to myocardial perfu sion SPECT. 3. Describe the findings and the likely culprit coronary artery or arteries. Does the bull's-eye plot confirm the image findings? 4. List the characteristics of perfusion scan abnormalities that should be included in any report. |
Cardiovascular System: Bull's-Eye,
Reporting Results 1. A polar plot is constructed by layering short-axis slices one on top of the other, with the apex forming the center and the base of the heart being the outermost portion. 2. Misregistration/misalignment, use of inappropriate refer ence database. 3. Stress: hypoperfusion of the anterior, lateral, and inferior walls. Rest, normalized perfusion of the anterior and lateral walls and incomplete normalization of the inferior wall. Most consistent with ischemia of the left circumflex and infarct of the right coronary artery. The bull's-eye confirms the image findings. 4. Include location and extent, severity, and reversibility for each perfusion abnormality. If gated SPECT is performed, include LVEF, wall motion, with or without wall thicken ing fractions. Note ancillary signs of significant CAD, e.g., increased 201Tl lung activity, or stress-induced dilation of the left ventricle, if present. |
|
|
A patient had atrial fibrillation and high baseline resting heart rate. The patient exercised for only 3.5 minutes,
achieved only 3.0 METS, but reached 100% of age-predicted maximum heart rate. SPECT short-axis (A) and hori zontal long-axis perfusion images (B). 1. Describe any perfusion abnormalities. 2. Describe any other findings. 3. What is the most likely culprit coronary artery? 4. Discuss the significance of failure to achieve adequate exercise. |
Cardiovascular System: Inadequate Stress
1. Severe fixed defect involving the entire lateral wall. 2. Dilated left ventricular cavity at both stress and rest. 3. Left circumflex coronary artery. 4. False-negative studies for ischemia may result. |
|
|
A 60-year-old patient with diabetes has severe chronic obstructive pulmonary disease (COPD) and uses a walker; he
denies chest pain. Short-axis (A) and horizontal long-axis (B) SPECT myocardial perfusion images are presented. 1. What form of stress is indicated for this patient and why? 2. Describe the perfusion abnormalities. 3. What is the likely culprit coronary artery? 4. Explain the discrepancy between the findings and patient's lack of symptoms. |
Cardiac: Silent Lateral Wall Ischemia
1. Dobutamine. The need of a walker precludes adequate exercise stress, and COPD is a contraindication to adeno sine or dipyridamole use. 2. Moderately severe perfusion defect involving the entire lat eral wall extending to the anterolateral, inferolateral regions, and apex on the stress images that nearly normal izes on the rest images. Incomplete reversibility of small portion of inferior wall. 3. Left circumflex coronary artery. 4. Silent myocardial ischemia. |
|
|
A 55-year-old woman with abnormal baseline ECG and left bundle branch block (LBBB) is sent for a stress dualisotope
SPECT study. LVEF and wall thickening by gated SPECT are normal. 1. Name the appropriate stress technique. 2. List stress methods that would be disadvantageous in this patient and state the reason. 3. Discuss the physiological advantage of adenosine or dipyridamole compared with other stress methods. 4. Describe the scintigraphic findings. |
Cardiovascular System: LBBB
1. Dipyridamole or adenosine. 2. Exercise or dobutamine. Methods of stress that result in increased heart rate can be associated with false-positive findings of septal reversibility (identical to isolated septal ischemia) in patients with LBBB. 3. These agents do not result in an increase in heart rate. 4. The mild decreased activity in the anterior wall appears fixed and likely is caused by breast attenuation in light of the reported normal wall motion. |
|
|
Gated radionuclide ventriculogram (RVG or MUGA) was performed.
1. Name the radiopharmaceutical used. 2. List methods for preparation of this radiopharmaceutical. 3. Describe the methodologies of radiolabeling. 4. List the advantages and disadvantages of the different labeling methods. |
Cardiovascular System: RBC Labeling
for RVG/MUGA 1. 99mTc-labeled RBCs. 2. In vivo, modified in vivo, and in vitro methods. 3. In vivo: stannous pyrophosphate is administered intra venously, followed in 15 to 30 minutes by 99mTc pertechnetate. Modified in vitro: stannous pyrophosphate is adminis tered intravenously and 15 to 30 minutes later, 3 to 5 ml of blood is withdrawn into an attached shielded syringe containing 99mTc pertechnetate and an anticoagulant, either acid-citrate-dextrose (ACD) or heparin. The blood is incu bated for 10 minutes and periodically agitated, then infused. The syringe is left attached to the indwelling intravenous line during the procedure so that the entire system is closed. In vitro: blood is withdrawn and placed in a closed vial containing stannous chloride and sodium hypochlorite to oxidize excess extracellular stannous ion and prevent extra cellular reduction of 99mTc pertechnetate. Labeling occurs when 99mTc pertechnetate is added, followed by a 20-minute incubation before reinjection of labeled cells. 4. The in vivo method is simplest and least costly, but has the lowest labeling efficiency. The in vitro kit method (UltraTag) has the highest labeling efficiency but requires more time, technologist effort, and cost. |
|
|
1. Describe and explain the processing performed on this equilibrium gated RVG or MUGA study.
2. How are the regions of interest (ROIs) selected? 3. List the nuclear medicine techniques by which left ventricular function can be assessed. 4. Provide the equation for determination of LVEF. |
Cardiac: Calculation of LVEF for RVG (MUGA)
1. Left anterior oblique end-diastolic and end-systolic images show left ventricular and background (bkg) ROIs drawn on computer for calculation of the LVEF. 2. Acquisition in the left anterior oblique (LAO) view with greatest separation of the left and right ventricle. ROI for the left ventricle at end-systole, at end-diastole, and for adjacent background. 3. Equilibrium gated blood pool (RVG); first-pass radionuclide ventriculography; gated perfusion SPECT. 4. LVEF = end-diastolic counts — end-systolic counts/ end-diastolic counts (corrected for bkg counts). |
|
|
Radionuclide planar gated blood pool study. Sequential gated image frames are shown.
1. Estimate the left ventricular ejection fraction (LVEF) based on the submitted images and explain the decreased intensity of image No. 16. 2. Discuss the importance of patient positioning on calculation of the LVEF. 3. List factors that may result in reduced accuracy of the LVEF calculation. 4. Describe the effect on the LVEF if (A) no background is subtracted; (B) a background region is used that includes the spleen. |
Cardiovascular System: RVG/MUGA
Technique 1. LVEF appears normal (>55%). End-systolic at Frame 8. Frame 16 shows decreased intensity compared with other frames, resulting from variability in the patient's heart rate, e.g., frequent PVCs. 2. The left anterior oblique (LAO) position selected is that which provides the best separation of the left and right ventricles, approximately a 45-degree LAO view, but varies depending on the patient's anatomy (best septal view). 3. Patient-related factors: arrhythmia, inability to gait, suboptimal RBC labeling, e.g., concomitant drugs. Techniquerelated: poor LAO positioning, suboptimal RBC labeling; incorrect ROI for left ventricle or background. 4. A, Falsely low; B, falsely high. |
|
|
A 35-year-old man with increasing dyspnea was referred for ventilation-perfusion (V/Q) study. The chest film was
clear of infiltrate, mass, or pleural disease. 1. Name the three phases of a 133Xe ventilation scan. 2. Describe the phases. 3. Describe the findings on the ventilation and perfusion scans. 4. Provide an interpretation and offer a diagnosis for the underlying disease. |
Pulmonary System: Emphysema Caused
by o^-Antitrypsin Deficiency 1. Single breath or wash-in, equilibrium, and washout phases. 2. Single breath: patient breathes in and holds a single maxi mum deep inspiration while a 100,000-count image is acquired. Equilibrium: patient breathes a mixture of air and xenon while serial images are obtained every 60 to 90 seconds for 3 minutes. Washout: patient breathes room air and exhales xenon while serial images are obtained. 3. Ventilation: nonuniform in the upper lung zones bilater ally. Initially near absent at the bases. As upper lobes wash out, xenon fills and is retained in both bases indicating severe air trapping. Perfusion: heterogeneous to both upper lung zones that match the early ventilation images. The extensive perfusion abnormalities in both lower lung zones are matched with areas of washout air trapping. 4. Low probability for pulmonary embolism, arantitrypsin deficiency. |
|
|
A 64-year-old man has recent onset of shortness of breath. The chest x-ray was clear.
1. Describe the image findings (A, perfusion; B, ventilation) and give an interpretation. 2. What is the ventilation study radiopharmaceutical, and what is its mechanism of distribution? What are the likely reasons for their appearance on this study? 3. Is the ventilation or perfusion study usually performed first and why? 4. What is another commonly used ventilation radiopharmaceutical that could be used, and what are the advantages and disadvantages? |
Pulmonary System: 99mTc DTPA Ventilation
Study with Aerosol Clumping 1. Multiple perfusion defects in upper and lower lung fields. Many appear segmental, e.g., the lateral basal of the right lower lobe, superior segment of the left lower lobe. Venti lation study shows extensive diffuse "clumping" within the airways throughout both lung fields making determination of matching or mismatching difficult. The study was inter preted as intermediate probability since the ventilation study could not be interpreted; however, the segmental perfusion defect pattern is suspicious for embolus. 2. 99mTc DTPA aerosol particles (0.1 to 0.5 \x,m in size) nor mally distribute on first impact within the alveoli. With airway turbulence, e.g., asthma or COPD, particles impact proximally within bronchi and appear as focal hot spots. 3. 99mTc DTPA aerosol ventilation study usually is performed first. The patient breathes in less than 1 mCi at tidal vol ume until an adequate count rate is obtained (3,000 counts/sec). The sixfold larger 99mTc MAA perfusion dose (5-mCi) overwhelms the retained ventilation dose, allow ing for two consecutive 99mTc studies. 4. 133Xe, an inert gas, is advantageous for patients with COPD and asthma. Delayed filling and clearance (air trapping) in regions of obstructive disease can be seen. Disadvantage: only posterior views are possible because of rapid exhalation. |
|
|
A 54-year-old man with known cardiopulmonary disease complains of increasing dyspnea. A, Chest radiograph;
B, perfusion scan; C, ventilation scan. 1. What are the scintigraphic findings and interpretation? 2. What is the likelihood of pulmonary embolus in this patient? 3. What is the likelihood of pulmonary embolus in a patient with a normal scan? 4. How are perfusion defects classified as to size? |
Pulmonary System: Low-Probability
Ventilation-Perfusion Scan 1. Bilateral inhomogeneous distribution. Matched perfusion and ventilation abnormalities throughout the upper and lower lobes, especially in the right lower lobe basal seg ments. Minimal atelectasis in the lower lobes on chest x-ray. Low probability for pulmonary embolus. 2. Less than 20%. 3. Less than 1%. 4. Large (segmental): greater than 75% of a segment. Moderate (subsegmental): 25% to 75% of a segment. Small (small subsegmental): less than 25% of a segment. |
|
|
A 29-year-old pregnant woman has a history of asthma and recent onset of dyspnea.
1. Is any patient preparation indicated? 2. Would the patient's pregnancy change the V/Q protocol? 3. Describe the perfusion (A) and ventilation (B) images and radiograph findings (C). 4. Give your interpretation of the study. |
Pulmonary System: Intermediate Probability and Pregnancy
1. Bronchodilator therapy before V/Q study as an asthmatic therapeutic trial. 2. Pulmonary emboli are life threatening to the patient and fetus. The radiation dose to the patient and fetus is low (less than 2 rads). The benefit/risk ratio is high. No change in procedure is required. In young, nonsmoking patients without cardiopulmonary disease, one might reduce the dose, conduct only a perfusion study, or both. 3. Hypoperfusion of the left lower lobe, except the superior segment. Better ventilation than perfusion with mismatch ing, in the anterior basal and part of the lateral basal segments. No ventilation in the posterior basal and part of the lateral basal. Costophrenic angle loss seen in left lateral and LPO views. Radiograph: atelectasis/infiltrate with elevation of the left diaphragm. 4. Intermediate probability for pulmonary embolus. One large/one moderate segmental mismatch and one large and one moderate segmental match corresponding to the x-ray atelectasis/infiltrate. |
|
|
Two patients (A and B) with similar histories of a soft tissue infection overlying the tibia. 99mTc HM-PAO leukocyte
studies were ordered to confirm or exclude underlying osteomyelitis. 1. Would a bone scan be useful as the initial study in these cases? 2. When would a bone marrow study with 99mTc sulfur colloid be useful in this clinical setting? 3. Would an ' "In oxine leukocyte study or 67Ga study be preferable? 4. Describe the findings. What are the diagnoses? |
Infection and Inflammation: 99mTc HM-PAO
Leukocytes and Osteomyelitis 1. A negative bone scan rules out osteomyelitis with a high degree of certainty. 2. A bone marrow study can improve the specificity of a leukocyte study if there is displaced normal marrow (orthopedic hardware). This is most helpful in the hips and knees. 3. ' "In leukocytes can make the same diagnosis. The superior imaging resolution of 99mTc HM-PAO often better differ entiates soft tissue and bone infection. 67Ga is less specific because increased uptake occurs with bone remodeling from any cause. 4. Patient A: soft tissue uptake. No bone uptake rules out osteomyelitis; consistent with cellulitis. Patient B: soft tis sue and bone localization consistent with osteomyelitis. |
|
|
A 49-year-old man was referred for 99mTc HM-PAO leukocyte study to locate the source of Staphylococcus aureus sepsis.
1. What are the scintigraphic findings? 2. What is your interpretation of the study? 3. What are the most common causes for false-positive radiolabeled leukocyte studies? 4. What is the optimal imaging period for 67Ga, ulIn oxine leukocytes, 99mTc HM-PAO leukocytes for infection imaging? |
Infection and Inflammation: 99mTc HM-PAO Leukocytes-free 99mTc pertechnetate
1. Activity in the salivary glands, thyroid, stomach, bowel, and bladder. 2. Free 99raTc pertechnetate. Nondiagnostic study. 3. Gastrointestinal bleeding, swallowed leukocytes from oropharyngeal, esophageal, or lung inflammation/ infection, accessory spleen, uninfected postoperative surgical wounds, intestinal stomas, and catheter sites. 3. 67Ga, 48 hours; nlIn oxine leukocytes, 24 hours; 99mTc HM-PAO leukocytes, 1 to 4 hours. |
|
|
A 25-year-old man has fever and abdominal pain. 99mTc HM-PAO-labeled leukocyte images.
1. Which leukocytes are labeled with the two radiopharmaceuticals used for leukocyte scans? 2. What is the explanation for the prominent skeletal uptake? 3. What is the optimal imaging time for ' "In oxine-labeled leukocytes and 99mTc HM-PAO leukocytes? 4. Give an image interpretation and diagnosis in this case. |
Infection and Inflammation: Intraabdominal Abscess
1. 99mTc HM-PAO binds only to neutrophils. nlIn oxine binds to mixed leukocytes. 2. Normal bone marrow distribution of the radiolabeled leukocytes. 3. Abdominal imaging: 99mTc HM-PAO images are acquired at 1 to 2 hours because hepatobiliary, intestinal, and renal clearance occurs subsequently, complicating interpretation. Extremity imaging: 2 to 6 hours. nlIn leukocytes: 24 hours. Four-hour imaging for inflammatory bowel disease because sloughing of intestinal mucosa leukocytes may occur and 24-hour may be misleading. 4. Infection in the right lower quadrant overlying the sacroiliac joint in the anterior view and lateral right of the spine. The patient had a perforated appendix. |
|
|
An 8-year-old girl with juvenile rheumatoid arthritis and persistent fever after resolution of recent pneumonia. She has
no current symptoms of arthritis. 1. Describe the findings on 67Ga sequential coronal SPECT chest images (A) and a selected enlarged image (B). Image intensity is high. What is the differential diagnosis? 2. What is the advantage of 67Ga over indium- or technetium-labeled leukocytes for fever of unknown origin? 3. What is the target organ (highest radiation absorbed dose) for 67Ga? 4. Which pulmonary infections or inflammatory diseases show increased 67Ga uptake? |
Infection and Inflammation: Pericarditis—67Ga
1. Abnormal uptake in myocardium, pericardium, or bothconsistent with pericarditis or myocarditis. The patient developed a pericardial friction rub the day after the 67Ga scan. Incidental note of normal liver uptake and transverse and left colon clearance. 2. 67Ga shows uptake not only with inflammation and infec tion, but also in tumors that can sometimes be the cause of persistent fever, e.g., lymphoma. 3. Large bowel, approximately 4.5 rads. 4. Most pulmonary inflammatory and infectious diseases. Uptake is nonspecific, although the pattern of uptake and the clinical setting, e.g., AIDS, may be helpful in deter mining the differential diagnosis. |
|
|
A, 70-year-old man with recent onset of flushing, diarrhea, elevated 5-hydroxyindoleacetic acid (5-HIAA), and a diag
nosis of carcinoid syndrome. B, 56-year-old patient with past history of medullary carcinoma of the thyroid and recent increase in serum calcitonin levels. 1. Provide the mechanism of uptake of" In pentetreotide (OctreoScan). 2. List the category of tumors for which this radiopharmaceutical is particularly useful. 3. Describe the image findings on these two studies: A (abdominal/pelvis view) and B (chest views), and give your interpretation. 4. Name the organs that normally have greatest uptake of the radiopharmaceutical. |
Oncology: Neuroectodermal Tumors
1. Peptide analogue of somatostatin and octreotide. Binds to tumors with somatostatin receptors. 2. Neuroendocrine tumors. 3. A, Multiple metastases to both lobes of the liver. Two large foci and one small focus of uptake consistent with paraaortic tumor adenopathy. Possible small tumor in right hilum (confirmed by later CT). B, Prominent irregular uptake in the anterior mediastinum and focal uptake in the left lower lung posteriorly. 4. Kidneys and spleen. |
|
|
Three patients in images A, B, and Chave whole body 67Ga scans.
1. What is the normal distribution of 67Ga? 2. Which studies show postchemotherapy changes? What are the findings? 3. What are other causes of 67Ga lung uptake? 4. Which study shows an altered distribution of the radiopharmaceutical? Causes? |
Oncology: Postchemotherapy 67Ga Findings
1. Greatest to least uptake: liver, bone/bone marrow, spleen, kidney (excretion pathway), salivary and lacrimal glands. 2. B, Thymus uptake is not an uncommon nonpathological finding after chemotherapy. C, Diffuse pulmonary uptake is consistent with pulmonary toxicity, e.g., bleomycininduced lung disease. 3. Gallium-avid tumor, inflammation, and infection. 4. A, Decreased hepatic and marrow uptake. Causes: recent MRI gadolinium contrast study, very recent chemotherapy, or iron saturation, e.g., multiple transfusions. |
|
|
A patient with malignant B-cell lymphoma. Initial FDG-PET study (A) shows tumor above and below the diaphragm.
Postchemotherapy CT shows a residual abdominal mass. Posttherapy FDG-PET (B). 1. Is remission complete or partial based on the CT and subsequent PET study? 2. What are the limitations of CT for staging and restaging of disease in patients with lymphoma? 3. List imaging limitations of 67Ga. 4. What are the advantages of 18F FDG-PET compared with 67Ga? |
Oncology: 18F FDG-PET—Lymphoma
1. The CT scan is indeterminate, but FDG-PET demonstrates a complete response. 2. CT assessment of tumor response is based on a decrease in the size of the mass or complete resolution. However, posttherapy residual masses are common and CT cannot dif ferentiate residual tumor from posttherapy fibrosis and necrosis. 3. Multiple high-energy photopeaks: 185, 300, 394 resulting in poor image resolution; frequent need for delayed imag ing (48 to 72 hours and sometimes 5 to 7 days) to allow for bowel clearance. 4. Study completed 2 hours after injection. FDG-PET targetto- background ratio is higher and image quality superior to 67Ga. Usually little bowel activity with FDG. Data are limited, but consensus is that FDG is superior to 67Ga. |
|
|
A 33-year-old male smoker has a poorly defined right mid-lung density on chest x-ray (A, marked). CT reported a
1.5-cm lesion with infiltrative margins in the superior segment of the RLL (B) but no other abnormality. 1. Describe the ' 8F FDG-PET scan findings (C). Sequential coronal slices are shown. 2. How has this PET scan affected the patient's preoperative staging? 3. What is the overall accuracy of CT and MR for preoperative staging of lung cancer? 4. What is the overall accuracy of 18F FDG-PET for preoperative lung cancer staging? |
Oncology: 18F FDG-PET—Lung Cancer Staging
1. Focal increased uptake corresponding to the nodule on CT (frames 358-370). In addition, abnormal uptake is seen in the right and left paratracheal regions, the right and left hilum, and the mediastinum, all consistent with tumor adenopathy. 2. 18F FDG-PET has preoperatively upstaged the patient, who is no longer a surgical candidate. 3. Approximately 65%. 4. Approximately 85%. |
|
|
A 69-year-old man has a history of colorectal carcinoma and surgical resection. The carcinoembryonic antigen (CEA)
level is increasing and the CT scan shows a new 2.3-cm lesion in the right lobe of the liver. 1. FDG-PET scan (A) was then obtained. What are the findings? 2. Why was the FDG-PET scan ordered? 3. What are clinical indications for FDG-PET in colorectal carcinoma? 4. FDG-PET scan (B) was performed 6 months after resection of the liver lesion. Describe the findings. |
Oncology: 18F FDG-PET—Colorectal Cancer Metastatic to Liver
1. Increased uptake consistent with tumor in the liver corre sponding to the reported CT mass. No other liver lesions or metastases are seen elsewhere in the whole body scan. 2. Surgical resection is planned. The preoperative FDG-PET scan is used to determine the presence of any other metas tases in the liver or elsewhere in the body that might change the surgical approach or make the patient inoperable. 3. (1) Increasing serum CEA levels with normal conventional imaging, (2) equivocal lesion with conventional imaging, and (3) preoperative staging before curative resection. 4. Negative scan. No evidence of tumor. |
|
|
A 54-year-old woman with bronchogenic carcinoma metastatic to the brain recently underwent stereotactic radiosurgery
for a lesion in the left temporoparietal region. MRI could not differentiate posttherapy changes from viable tumor (A). 1. Give the relative accuracy of FDG-PET versus CT or MRI for diagnosing malignant tumor in the brain. 2. What is the relative accuracy of FDG-PET versus CT/MRI for differentiating recurrent or persistent tumor from postradiation necrosis? 3. Describe the image findings and interpret the transaxial images (B) of FDG-PET of the brain. 4. List single photon radiotracers used for brain imaging and describe the expected findings. |
Oncology: 18F FDG-PET—Bronchogenic Cancer
Metastatic to Brain 1. CT and MRI are more sensitive for tumor detection. Normal brain uses only glucose for metabolism and has higher uptake than any other organ. This results in high background that can make tumor detection difficult. 2. FDG-PET is more accurate than CT or MRI for deter mining whether posttherapy changes are the result of residual/recurrent tumor or radiation necrosis. 3. Focal increased uptake in the left temporoparietal region that correlates with the lesion on MRI. This is consistent with viable residual or recurrent tumor. 4. 2O1T1 and 99mTc sestamibi have increased uptake in tumors. Tumors usually are cold on 99mTc HM-PAO and ECD. |
|
|
A 35-year-old-man with AIDS has a new intracranial abnormality on MRI (A and B) of uncertain origin. A SPECT
study (Cl, coronal; C2, sagittal; C3, transverse) was ordered to assist in the differential diagnosis. 1. What is the radiopharmaceutical? 2. What is the differential diagnosis before the SPECT study? 3. What is the likely diagnosis after the radionuclide study? 4. What is the accuracy of the radionuclide method? |
Oncology: 201TI—Intracranial Lymphoma
1. 201Tl was used. 99mTc sestamibi also can be used; however, it is taken up by the choroid plexus and could pose diag nostic problems in some cases. 2. Tumor, particularly lymphoma, versus infection, usually toxoplasmosis, or other opportunistic infections, e.g., cytomegalic inclusion virus, herpes simplex, Cryptococcus. 3. Malignant lymphoma. 4. Approximately 90% sensitivity for tumor. False-positive rate of less than 10%. |
|
|
A 49-year-old woman was referred for breast lymphoscintigraphy after recent biopsy of a right breast mass and the di
agnosis of breast cancer. 1. What is the implication of axillary node involvement in breast cancer? 2. What is a sentinel node? 3. What is the purpose of sentinel node biopsy? 4. What is the radiopharmaceutical used, and how is the study performed? |
Oncology: Breast Cancer Lymphoscintigraphy
1. The 5-year survival rate for breast cancer decreases with axil lary node involvement. Adjuvant chemotherapy is indicated. 2. A sentinel node is the first node drained by the lymphatics in a nodal basin. 3. If the sentinel node biopsy is tumor negative, no axillary dissection is needed. If positive, axillary dissection is performed. 4. The pharmaceutical often used is filtered 99mTc sulfur col loid. It is injected around the lesion or biopsy site. Imag ing usually is performed. At surgery a gamma probe is used to help locate the sentinel node. |
|
|
Sentinel node lymphoscintigraphy was performed for malignant melanoma in the mid-left posterior thorax. Oneminute
posterior images (A) are followed by anterior and posterior static images with a cobalt transmission source placed behind the patient for body contour (B). A lead shield was placed over the injection site on the static posterior images (appears cold). 1. What is the radiopharmaceutical commonly used and what is the rationale for its use? 2. Describe the study findings. 3. What is the normal drainage of a mid posterior chest or flank lesion? 4. How are patients with melanoma selected for lymphoscintigraphy? |
Oncology: Melanoma Lymphoscintigraphy
1. Filtered 99mTc sulfur colloid particles, 0.1 to 0.22 |xm in size, are injected intradermally, taken up by the lymphat ics, and demonstrate lymphatic channels and nodes. 2. One-minute dynamic images: drainage to the right axilla through two separate lymphatic channels, also drains to the left axilla. Nodal uptake in the right axilla is seen on the static posterior view. The anterior view shows two right sentinel nodes and one on the left. 3. Drainage is unpredictable, and may drain to either axillary or to inguinal regions. 4. Prognosis is determined by lesion depth. Those less than 0.76 mm are low risk and rarely metastasize; those deeper than 4 mm often metastasize. Patients with intermediate thickness lesions are referred for lymphoscintigraphy and sentinel node biopsy. |
|
|
A 43-year-old woman was hospitalized with abdominal pain, nausea, and vomiting that started 24 hours before
cholescintigraphy. 1. What are the cholescintigraphic findings? 2. What clinical information would be helpful to correctly interpret the study? 3. What is the differential diagnosis? 4. What would you do next? |
Hepatobiliary System: Delayed Biliary-to- Bowel Transit
1. Normal gallbladder filling and secretion into biliary ducts; however, no clearance of radiotracer from the common duct or biliary-to-bowel transit by 60 minutes. 2. Is the patient receiving narcotics? Was sincalide (CCK) given before the study? 3. Partial common duct obstruction, functional obstruction caused by sincalide administered before the study, recent narcotic administration, or normal variation. 4. Obtain delayed images or give CCK. The latter would give the answer more promptly. |
|
|
A 63-year-old woman has been hospitalized for 9 days with multiple serious medical problems and is receiving hyperalimentation.
Now acute abdominal pain has developed. She has been referred for cholescintigraphy to rule out acute cholecystitis. A, 60-minute cholescintigraphy. B, Additional 30-minute images after administration of morphine. 1. What is the relative accuracy of cholescintigraphy in this patient's clinical setting? 2. Describe the cholescintigraphic findings. 3. What is the clinical significance of these findings? 4. What pathological condition is likely? |
Hepatobiliary System: RIM Sign
1. Increased incidence of false-positive study results in patients who have been fasting more than 24 hours, those receiving hyperalimentation, or those with concomitant serious illness. 2. Nonvisualization of the gallbladder after 60 minutes. After morphine administration no filling of the gallbladder occurs. Increased uptake is seen in the region of the gall bladder fossa, which persists after most of the liver has washed out (RIM sign). 3. Nonvisualization of the gallbladder after morphine admin istration is consistent with acute cholecystitis, but the specificity is reduced somewhat in this clinical setting (hyperalimentation). The RIM sign is very specific for acute cholecystitis and confirms the diagnosis. 4. The RIM sign indicates severe acute cholecystitis, which is associated with an increased incidence of gallbladder gan grene and perforation. |
|
|
A 50-year-old woman has acute onset of abdominal pain of 4 hours' duration. Ultrasonography results are normal.
1. What are the cholescintigraphic findings and the diagnosis? 2. Differentiate the terms surgicaljaundice, biliary obstruction, and bile duct dilation. 3. Differentiate the 99mTc IDA findings of high- and low-grade biliary obstruction. 4. How do the cholescintigraphic findings of hepatic insufficiency differ from this case? |
Hepatobiliary System: High-Grade Biliary
Obstruction 1. Prompt hepatic uptake, no excretion into the biliary tract, consistent with high-grade common duct obstruction. Cholestatic jaundice, e.g., drug reaction, may look similar. 2. Obstruction may occur without jaundice. Jaundice is a late manifestation. Obstruction does not always result in ductal dilation. Dilation can be present without obstruction. 3. High-grade: hepatic uptake, no biliary clearance. Lowgrade: secretion into biliary ducts, delayed clearance from the biliary ducts, and delayed biliary-to-bowel transit. 4. Hepatic insufficiency: delayed liver uptake and delayed hepatic and background clearance, often delayed biliaryto- bowel transit. |
|
|
A 50-year-old man with several months of abdominal discomfort and jaundice.
1. Describe the cholescintigraphic findings. 2. What is the differential diagnosis at 60 minutes? 3. How have delayed images helped make the diagnosis? 4. What are the possible FDA-approved radiopharmaceuticals and their alternative route of excretion? |
Hepatobiliary System: Hepatic Insufficiency
1. Poor hepatic function: delayed blood pool (heart and great vessels) and background clearance, no secretion into biliary ducts at 60 minutes. Delayed images show very late filling of the gallbladder and biliary-to-bowel transit by 24 hours. 2. Hepatic insufficiency, biliary obstruction with secondary hepatic insufficiency. 3. Delayed images show no radiotracer retention within the biliary ducts and biliary-to-bowel transit, ruling out obstruction. 4. 99roTc mebrofenin or bromotriethyl minodiacetic acid (IDA; Choletec) or 99mTc disofenin or DISIDA (Hepatolite). Renal excretion. |
|
|
A 39-year-old woman with abdominal pain; history of cholecystectomy. Results of real-time ultrasonography are normal.
1. Describe the cholescintigraphic findings. 2. Give the differential diagnosis at 60 minutes. 3. Give the diagnosis at 120 minutes. 4. What is an alternative method for making the diagnosis? |
Hepatobiliary System: Acute Cholecystitis
and Biliary Obstruction 1. Nonfilling of the gallbladder, prominent retained activity in the common duct at 60 minutes, with definite biliaryto- bowel clearance. Continuing biliary-to-bowel transit at 120 minutes, however, increased retention in the commonduct. Minor enterogastric reflux. 2. Partial biliary obstruction, hyptonic sphincter of Oddi (normal variation, CCK given before the study, chronic cholecystitis. 3. Very suspicious for partial common duct obstruction. 4. Administer CCK. |
|
|
Both patients are 4 weeks old (A and 5). They have hyperbilirubinemia and were referred to rule out biliary atresia.
1. What patient preparation is required before the cholescintigraphic study? 2. What is the differential diagnosis of hyperbilirubinemia in this age group? 3. What are the scintigraphic findings on these studies and your interpretations? 4. What is the accuracy of cholescintigraphy to diagnose biliary atresia? |
Hepatobiliary System: Biliary Atresia
1. Phenobarbital, 5 mg/kg/day for 3 to 5 days before the study. 2. Inflammatory, infectious, and metabolic causes for neona tal hepatitis and biliary atresia. 3. A, Delayed blood pool clearance (note heart) as a result of hepatic insufficiency. Biliary clearance at 50 minutes and increasing through 120 minutes. Note the medial edge of the gallbladder (image intensity set high to see bowel activity). B, Good liver function. No secretion into biliary ducts during the initial 120 minutes or at 5 and 24 hours. Case B is consistent with biliary atresia, case A with neona tal hepatitis. 4. Sensitivity 97%, specificity 82%. |
|
|
A 46-year-old woman had two different SPECT radionuclide liver studies (A and B). Comparable selected transaxial
slices are shown for the two studies. 1. Name the two radiopharmaceuticals used. 2. What are the scintigraphic findings? 3. What is the differential diagnosis of scan B alone? 4. What is the diagnosis in this patient? |
Hepatobiliary System: Cavernous Hemangioma
of the Liver 1. A, 99mTc-labeled RBC liver study. B, »Tc sulfur colloid study. 2. Increased uptake on the 99mTc-labeled RBC study in the same region where a defect (photopenic region) is seen on the 99mTc sulfur colloid study. 3. Any benign or malignant mass lesion of rhe liver. 4. Cavernous hemangioma of the liver. |
|
|
This patient has a history of idiopathic thrombocytopenic purpura and prior splenectomy, and now has clinical evidence
of recurrent disease. Anterior, posterior (A), and left lateral view of a radionuclide scan (B) with the intensity set high. 1. What is the radiopharmaceutical? 2. What is the likely purpose of the study? 3. Could other studies be used to make the same diagnosis? 4. How would you interpret the study? |
Hepatobiliary System: Splenic Remnant
1. 99raTc sulfur colloid. 2. To detect a splenic remnant, splenosis, or accessory splenic tissue. 3. Heat or chemically damaged 99mTc RBC study. 4. Positive for the presence of a splenic remnant. |
|
|
Bright red blood per rectum. No prior history.
1. What radionuclide study is this? Describe the scintigraphic findings. 2. Provide an accurate location for the findings. 3. Name another method of image review that should be used. 4. Provide the differential diagnosis. |
Gastrointestinal System: Gastrointestinal
Bleeding as a Result of Angiodysplasia 1. 99mTc-Iabeled erythrocyte study. Abnormal focal uptake appearing simultaneously at two sites in the right abdo men, increasing in intensity and changing in pattern with time. 2. Cecum and ascending colon. 3. Review images on a computer monitor in cinematic mode. 4. Acute bleeding due to angiodysplasia, diverticula, neoplasm, inflammatory bowel disease, and ischemia. |
|
|
Recent bright red blood per rectum and low hematocrit.
1. Based on the history, what nuclear scans would be appropriate? 2. What information from the history is critical to determine the appropriate time to perform the examination? 3. Name the radiopharmaceutical used for this examination. 4. Describe the scintigraphic findings (first six images are blood flow, last two are delayed statics). |
Gastrointestinal System: 99mTc RBC Scan— Axillobifemoral Bypass Craft
1. 99mTc-labeled red blood cells or 99mTc sulfur colloid. 2. Evidence of current or recent gastrointestinal bleeding. 3. 99mTc-labeled RBCs. 4. The vascular flow and delayed static images show no active gastrointestinal bleeding. Labeled red cells are shown in a tubular shape in the right abdomen that connects after a Y bifurcation to the two iliac vessels as a result of an axillobifemoral vascular bypass graft. The patient has prominent splenomegaly. |
|
|
Two patients (A and B) were referred for a radionuclide gastrointestinal bleeding study.
1. What is the radiopharmaceutical used in these studies? 2. Describe the image findings in both studies. 3. Interpret the two studies. 4. Which method of radiolabeling of RBCs has the highest labeling efficiency? |
Gastrointestinal System: 99mTc RBC-Free
Pertechnetate versus Gastric Bleeding 1. 99raTc pertechnetate labeled to RBCs. 2. In both studies the stomach visualizes promptly. The chest and neck image shows thyroid and salivary uptake in study A (15-minute image) but not in study B (120-minute image). 3. A, Free 99mTc pertechnetate. Negative for gastrointestinal bleeding. B, Active bleeding originating from the stomach. 4. In vitro. |
|
|
A patient has a seizure disorder unresponsive to medical therapy and is being considered for surgical treatment.
1. Describe the image finding on these coronal 18F FDG-PET slices. 2. What is the differential diagnosis of this image finding if no history was available? 3. What is the probable seizure focus site? 4. What is the utility of PET or SPECT in seizure disorders? |
Central Nervous System: Seizure Disorder
1. Decreased metabolism in the left temporal lobe. 2. Temporal lobe infarct, benign mass or low-grade tumor, postradiation therapy changes, interictal left temporal lobe seizure focus. 3. Interictal seizure focus in the left temporal lobe. 4. Confirmation of the location of the seizure focus in a can didate for temporal lobectomy. Study is an alternative to surgical depth electrode placement. |
|
|
A 55-year-old man has had worsening dementia over 10 months.
1. Give a clinical differential diagnosis for dementia. 2. How can SPECT or PET aid in this differential diagnosis? 3. Describe the 18F FDG-PET findings on the reconstructed three-dimensional volume display. 4. What is the diagnosis and with what degree of certainty? |
Central Nervous System: Alzheimer's Disease
1. Multiinfarct, Alzheimer's disease, AIDS-related, substance abuse, alcoholism, Parkinson's, Pick's, Creutzfeldt-Jacob disease, depression, metabolic. 2. Diagnostic patterns using 9>mTc HM-PAO/ECD SPECT and FDG-PET: multiinfarct dementia, Alzheimer's disease, frontal lobe dementias, e.g., Pick's disease. 3. Hypometabolism (decreased FDG uptake) of the posterior parietal and temporal lobes bilaterally and to a lesser extent the frontal lobes. Note persistent metabolism of sensorimotor cortex. 4. Alzheimer's disease; greater than 80% certainly. |
|
|
A 55-year-old man has increasing dementia. Recently he had a normal MRI. Sagittal SPECT sections are submitted.
1. List the most common causes of dementia in the elderly. 2. Describe the mechanism of uptake of the radiopharmaceutical used. 3. What causes of dementia are associated with characteristic SPECT perfusion patterns? 4. Describe the findings and the most likely diagnosis. |
Central Nervous System: Pick's Disease
1. Alzheimer's disease, multiinfarct, late-stage Parkinson's dis ease, metabolic, drug-related, depression. 2. The lipophilic 99mTc HM-PAO or ECD agents cross the intact blood-brain barrier and have rapid intracellular uptake in proportion to cerebral blood flow. They are fixed intracellularly. Subsequent imaging provide a "snapshot" of the blood flow pattern at the time of the injection. 3. Alzheimer's, multiinfarct dementia, Pick's disease. 4. Decreased blood flow in the frontal cortex bilaterally as a result of frontal lobe dementia, e.g., Pick's disease. |
|
|
A 25-year-old woman had a kidney transplant 7 days earlier.
1. What are the scintigraphic findings of this 99mTc MAG3 study? 2. What is the most likely diagnosis? 3. What are the usual associated clinical symptoms and findings? 4. How is the final diagnosis established? |
Genitourinary System: Acute Renal Transplant
Rejection 1. Very decreased and delayed blood flow and poor trans plant function. 2. Acute rejection. 3. Fever, transplant tenderness and enlargement, decreased urinary output, and rising serum creatinine level. 4. Biopsy. |
|
|
A 59-year-old man admitted to the hospital with pneumonia, elevated serum creatinine level, and no known renal
disease. 1. In what projection are renal studies acquired? Name the structures seen on the flow study (A). 2. What are the findings on the postflow dynamic 30-minute study (B)? What is the diagnosis? 3. What three general causes of renal failure can the radionuclide study help diagnose? 4. Name the appropriate radiopharmaceutical in this clinical setting? |
Genitourinary System: Renal Insufficiency—Small Kidneys, Poor Function
1. Posterior. Right ventricle, lungs, left ventricle, aorta, spleen (not left kidney). The kidneys are very poorly visualized on this flow study, consistent with poor blood flow. 2. Bilaterally small kidneys. Extremely poor renal function. Clearance into the bladder. Diagnosis of chronic renal insufficiency secondary to parenchymal disease. 3. The radionuclide renogram can differentiate prerenal, intrarenal (parenchymal), and postrenal causes. 4. 9')mTcMAG3. |
|
|
A 30-year-old man has poorly controlled and accelerating hypertension. Baseline study without captopril (A) and
99mTc MAG3 renal studies with captopril (B) are shown. 1. What is the rationale and physiological mechanism for the captopril renal study? 2. What are the scintigraphic and time-activity curve findings and diagnosis? 3. Could 13II hippuran or 99mTc DPTA have been used instead? 4. What is the accuracy of captopril renography? |
Genitourinary System: Captopril Renography
1. With renal artery stenosis, glomerular perfusion decreases and glomerular filtration rate (GFR) drops. Renin released from the juxtaglomemlar apparatus converts angiotensin I to angiotensin II. Angiotensin II causes vasoconstriction of the glomerular efferent arterioles, raising filtration pressure and maintaining GFR. An angiotensin-converting enzyme (ACE) inhibitor, e.g., captopril, blocks conversion of angiotensin I to II, resulting in a decrease in GFR. 2. The right kidney is small but with good function. With captopril cortical retention persists, consistent with renindependent renovascular hypertension of the right kidney. This is confirmed by the renal cortical time-activity curves. 3. Yes. The accuracy of 13II hippuran, 99mTc DTPA, and 99mTc MAG3 are similar. 4. Sensitivity, 90%; specificity, 95%. Sensitivity is less for detection of renin-dependent hypertension if the patient has been taking an ACE inhibitor chronically or has renal insufficiency. |
|
|
A 7-year-old with hydronephrosis demonstrated on ultrasound examination. No prior history.
1. Based on the history, list the preferred radiopharmaceutical(s) for this study. 2. Would a renal cortical agent be appropriate? 3. Describe the initial findings (A) and following diuretic administration (B and C). 4. List the differential diagnosis and most likely diagnosis. |
Primary Megaureter
1. 99raTc MAG3 or 99mTc DTPA. 2. No, both 99mTc dimercaptosuccinic acid (DMSA) or 99mTc glucoheptonate fix to the renal cortex. 3. Left kidney excretes promptly into collecting system with retention in prominent pelvis and ureter. Prominent dila tion distally. After diuretic: prompt clearance of the left collecting system by visual and quantitative assessment. Normal right kidney. 4. Dilated nonobstructed left ureter. Possible causes: vesicoureteral reflux, corrected ureteral vesicle junction obstruc tion, and primary megaureter; the latter is more likely based on the prominent dilatation of the distal ureter. |
|
|
A 6-year-old girl has recurrent and recent urinary tract infections. A, 99mTc DMSA SPECT renal study. B, A repeat
study 6 months later (comparable coronal slices). 1. What is the mechanism of uptake of 99mTc DMSA? 2. What are the most common indications for a 99mTc DMSA study? 3. What are the scintigraphic SPECT findings and what is the diagnosis? What would have been the diagnosis if the second study (B) looked similar to the first study (A)? 4. What is the clinical importance of differentiating upper and lower tract infection? |
Genitourinary System: Pyelonephritis and
99mTc DMSA 1. Forty percent of 99mTc DMSA binds and fixes to function ing proximal cortical renal tubules. 2. Diagnosis of pyelonephritis or cortical scarring. 3. Decreased uptake in the lower half of the right kidney on initial imaging (A). Repeat SPECT show normalization of uptake. A, Pyelonephritis; B, renal cortical scarring. 4. "'"Tc DMSA in the early stages of infection is the best predictor of renal sequelae. Identification of pyelonephritis will increase the duration of antibiotic therapy. |
|
|
A 39-year-old woman has a 3-year history of hyperthyroidism. 123I thyroid scans were performed each year, shown
from left to right. 1. Describe the scintigraphic findings. 2. Give the diagnosis. 3. What treatment options are appropriate for this patient? 4. What would you expect the radioactive iodine thyroid uptake to be? |
Endocrine System: Toxic Autonomous Thyroid Nodule
1. Hot nodule in the mid-right lobe of the thyroid, with increasing suppression of the remaining gland at each successive year. 2. Toxic autonomous thyroid nodule. 3. Surgery and radioactive I3II are the usual methods of treat ment. Therapy with propylthiouracil (PTU) or methimazole (Tapazole) sometimes is used as initial treatment. 4. The radioactive iodine uptake may be moderately elevated, but it often is in the normal range. Normal 24-hour uptake is 10% to 30%. |
|
|
99mTc pertechnetate scan in a 3-year-old child with a subiingual mass. Patient is euthyroid.
1. What is the mechanism of 99mTc pertechnetate and 123I sodium iodide uptake? 2. What is the advantage of 99mTc pertechnetate over 123I in this patient? 3. Describe the scintigraphic findings. 4. What is the diagnosis? |
Endocrine System: Lingual Thyroid
1. 99mTc pertechnetate is taken up (trapped) by thyroid follicular cells like iodine but not organified. I23I is taken up and organified. 2. Lower radiation exposure to the pediatric patient. 3. Focal uptake at the base of the tongue. Normal in submandibular glands and mouth. No thyroid in neck. 4. Lingual thyroid. |
|
|
99mTc pertechnetate thyroid scan in a patient with clinical hyperthyroidism.
1. Describe the scintigraphic findings. 2. Describe the scan evidence that supports the reported hyperthyroidism. 3. What is the differential diagnosis regarding the left lobe? 4. The right lobe is two times normal size by examination. The left lobe is not palpable, no nodules are felt, and no scars are present. What is the most likely diagnosis? |
Endocrine System: Thyroid Left Lobe
Agenesis—Craves' Disease 1. Uniform uptake in a bulbous-appearing right lobe, with out focal areas of increased or decreased uptake. No activity in the expected location of the left lobe or elsewhere in the neck or upper chest. 2. The uniform activity in the right lobe is more intense than in the salivary glands, indirect evidence of an elevated uptake in the absence of intrinsic salivary gland disease. 3. Surgical excision, replacement by hypofunctioning adenoma or carcinoma, suppression by autonomously functioning adenoma on the right, agenesis of the left lobe with Graves' disease of the solitary right lobe. 4. Graves' disease with agenesis of the left lobe. |
|
|
A 45-year-old man had surgery for hyperparathyroidism that has persisted postoperatively.
1. What is the radiopharmaceutical and study? 2. Describe the scintigraphic findings. 3. What is the differential diagnosis for these findings? 4. What is the likely diagnosis in this clinical setting? |
Endocrine System: Mediastinal Parathyroid Adenoma
1. Parathyroid scan with 99mTc sestamibi or 99mTc tetrofosmin. (Image quality would be inferior with 201Tl.) 2. Focal persistent uptake in the mediastinum, normal salivary, liver, cardiac uptake. Apparent axillary uptake resolves with arms elevated, thus is caused by skin folds. 3. Various benign or malignant neoplasms. 4. Mediastinal parathyroid adenoma. |
|
|
A 47-year-old woman with recent onset of severe hypertension and elevated catecholamine levels.
1. What is the radiopharmaceutical? 2. What is the radiopharmaceutical's mechanism of uptake? 3. What is the accuracy of this study for locating the site of disease? What is the disease? 4. What other diseases take up this radiopharmaceutical? |
Endocrine System: MIBG—Pheochromocytoma
1. 131I meta-iodo-benzyl-guanidine (MIBG). 2. Localization occurs through the norepinephrine reuptake mechanism. It localizes in catecholamine storage vesicles in presynaptic adrenergic nerve endings and the cells of the adrenal medulla. 3. Sensitivity, 90%; specificity, 95% for detection of pheochromocytomas. 4. Various neuroendocrine tumors take up the radiopharmaceutical: neuroblastoma (90%), carcinoid (50%), and medullary carcinoma of the thyroid (25%). |
|

Bone scans A, B, and C.
1. Describe the bone scan findings. 2. Interpret the studies. 3. Name the physical principle that is involved in C. 4. Name the most likely type of material involved in C. |
Skeletal System: Arterial Injection, Boot Artifact, Photopenic Attenuation Artifact
1. A, Increased uptake in the right upper extremity from elbow through hands. B, Uptake outside bone in both feet and ankles, right greater than left. Urinary contamination of scrotum. C, Photopenia of a portion of the right midhumerus on the posterior view only. Lumbar scoliosis. Left hip prosthesis. 2. A, Intraarterial injection. B, Urinary contamination of socks (boot artifact). C, Attenuation artifact of right humerus. 3. Attenuation of photons. 4. Metal. |
|
|
Three-view format of selected coronal, sagittal slices, and transaxial images from SPECT bone scans of two patients
with cancer and low back pain. The bottom right images are the posterior projection preprocessed raw images. 1. Describe the scintigraphic SPECT findings in studies A and B. 2. Give the likely diagnosis in both patients. 3. Why is accuracy of lumbar spine SPECT higher than for planar imaging? 4. How can bone SPECT be clinically helpful in diagnosing disease in a patient with recurrent pain 1 year after spinal surgery? |
Skeletal System: Improved Specificity with Bone Scan Lumbar SPECT
1. A, Uptake in the region of the L4 right pedicle, extending to the vertebral body. B, Uptake in the region of the L2 facet joints bilaterally, right greater than left. 2. A, Metastatic tumor. B, Articular facet osteoarthritis. 3. SPECT improves the target-to-background ratio by removing overlying activity from adjacent slices and allows for three-dimensional display. 4. One year after surgery a healed fusion has no more than minimally increased activity, whereas a pseudoarthrosis shows active bony repair with increased activity. |
|
|
A patient was referred for bone scan because of joint pain.
1. Describe the scintigraphic bone findings. 2. Describe any soft tissue findings. What is the likely cause? 3. What other imaging study should be ordered? 4. What is the diagnosis and most likely common cause for this scan pattern? |
Skeletal System: Pulmonary Hypertrophic Osteoarthropathy
1. Diffuse increased uptake in the upper and lower extremi ties and periarticular regions of the elbow, wrist, and ankle joint. Uptake in the seventh right rib anteriorly. 2. Diffuse uptake in the right thorax. The most common cause is malignant pleural effusion. 3. Chest x-ray. 4. Hypertrophic pulmonary osteoarthropathy. Bronchogenic cancer of the lung. |
|
|
A patient with diabetes was referred with cellulitis of the right lower leg to rule out osteomyelitis.
1. Discuss the advantage of a three-phase bone scan compared with the delayed phase only. 2. Describe the scintigraphic bone scan findings. Flow (A), blood pool (B), delayed (C), D, Radiograph. 3. Provide the differential diagnosis. 4. What is the most likely diagnosis? |
Skeletal System: Gangrene of Toes
1. The flow and blood pool phases increase the specificity of the diagnosis and narrow the differential diagnosis. 2. Diffuse increased blood flow and blood pool to the foot and ankle of the right lower extremity. No blood flow, pool, or uptake of the right third and fourth toes, mild increase in all bones on the delayed image, slightly worse at the first metatarsophalangeal (MTP) joint. 3. Vascular insufficiency, prior surgery, acute osteomyelitis, frostbite, replacement by tumor, artifact. 4. Arterial insufficiency and gangrene of the third and fourth toes; cellulitis; mild arthritis of first MTP joint. |
|
|
1. Describe the bone scan abnormality. A, Flow. B, Immediate and delayed plantar images.
2. Provide the differential diagnosis. 3. Given the radiograph (C), name the entity. List at least three other sites that are subject to the same process. 4. List at least three conditions associated with this entity |
Skeletal System: Avascular Necrosis of
Metatarsal Head (Freiberg's Disease) 1. The three-phase bone scan demonstrates abnormal increased blood flow and blood pool activity in the region of the second and third metatarsal heads. The delayed bone phase demonstrates increased activity in the bones in the same distribution. 2. Fracture, osteotomy, osteomyelitis, primary or secondary neoplasm, avascular necrosis. 3. Avascular necrosis. Tarsal navicular, carpal lunate, femoral head, humeral head, ring apophyses of the spine, tibial tubercle. 4. Trauma, hypercortisolism, collagen vascular disease, chronic renal disease, aspirin, sickle cell disease, alcoholism, dysbaric conditions. |
|
|
A bone scan was requested for evaluation of hip pain and low-grade fever in an 11-year-old. The hip radiograph was
normal. 1. What imaging instructions should be given to the technologist? 2. Describe the scintigraphic findings {above, blood flow; below left, blood pool; below middle and right, delayed images). 3. Provide the differential diagnosis. 4. Bone biopsy: neuroblastoma. Name another radiopharmaceutical used in this disease. |
Skeletal System: Neuroblastoma Mimicking
Osteomyelitis 1. Three-phase bone scan with attention to the hips because of the acute nature of the symptoms and infection is a clinical consideration. 2. Moderately increased flow, blood pool, and delayed uptake in the proximal right femur metaphysis. 3. Osteomyelitis, fracture, primary or secondary malignant tumor (monostotic), fibrous dysplasia. 4. I31I metabenzylguanidine (MIBG) and '"In pentetreotide, a somatostatin receptor radiotracer. |
|
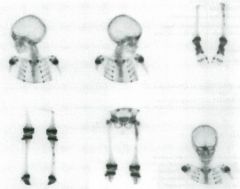
A 5-year-old with precocious puberty.
1. Name two findings that might be seen when examining this patient. 2. Describe the scan findings. 3. What bone lesion is most likely? 4. Name the syndrome that this patient has. |
Skeletal System: Fibrous Dysplasia,
McCune-Albright Syndrome 1. Pigmented "cafe-au-lait" skin lesions, gynecomastia. 2. Abnormal uptake is seen in the frontal bone, left femur, left tibia, with a nonuniform pattern of uptake in the long bones. 3. Polyostotic fibrous dysplasia. 4. McCune-Albright syndrome. |
|
|
1. Describe the bone scan skeletal abnormalities.
2. Provide the differential diagnoses for the bone abnormalities. 3. Describe the ancillary nonbone abnormalities. 4. Given the presence of nonbone and bone abnormalities, provide the most likely diagnosis. |
Bone: Renal Osteodystrophy
1. Increased cortical radiotracer activity in the long bones of the upper and lower extremities. "Railroad tracking" and bowing of the femurs. Bilateral hip prostheses. 2. Hypertrophic osteoarthropathy, vitamin A intoxication, fluorosis, renal osteodystrophy, thyroid acropachy, melorheostosis. 3. High bone-to-soft tissue uptake ratio. Renal nonvisualization. Minimal bladder activity. Additional history: patient is undergoing dialysis following a failed kidney transplant. 4. The scan is characteristic of renal osteodystrophy. Prior hip replacements for avascular necrosis caused by steroid therapy related to the kidney transplant. |
|
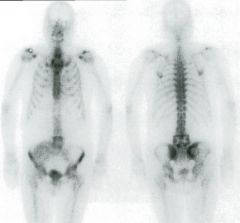
Newly diagnosed prostate cancer.
1. List the abnormalities demonstrated in the bones. 2. Provide the most likely diagnosis. 3. List any other abnormalities. 4. What is most likely diagnosis? |
Skeletal System: Lumbar Spinal Fusion, Renal
Transplant 1. Abnormal contour at the L4 and L5 level, with relative increase in the diameter of the apparent vertebrae, central photopenia in a well-defined geometrical pattern sur rounded by increased activity. Abnormal increased uptake in a crescent pattern in the right sacral ala. 2. Posterior fusion with bone graft material seen lateral to the expected contour of the vertebra. The photopenia is caused by orthopedic hardware (pedicle screws and plates). The right iliac crest is the bone graft donor sice. 3. Nonvisualization of kidneys in the expected location; tracer excretion is present in the bladder. Faint soft tissue uptake overlying and extending superior to the right ilium. 4. Lumbar spinal fusion. Renal transplant in the right iliac fossa. |
|
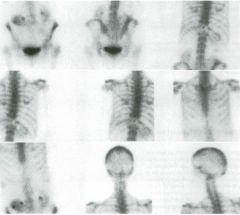
1. The patient was referred for back pain. Describe the bone findings.
2. Describe any other nonosseous findings. 3. Provide the differential diagnosis for the bone abnormality. 4. List three possible primary neoplasms. |
Skeletal System: Metastases to Bone (Cold)
and Adrenal Gland 1. Photopenia of a low thoracic vertebra, probably Til. 2. Ptotic kidneys, abnormal soft tissue uptake seen between the posterior right eleventh and twelfth ribs. 3. Primary or metastatic neoplasm, attenuation from external or internal source, e.g., buckle on back of clothing, metal lic orthopedic hardware, or prior vertebroplasty. 4. Breast, colon, lung; neuroblastoma in a child, but clearly this patient is an adult. |
|
|
Limited bone scan (left) in patient with left distal femur osteosarcoma. A different type of nuclear study was done
before (middle) and after chemotherapy (right). 1. Describe the bone scan findings. 2. Is a whole-body bone scan warranted? 3. What is the second radiopharmaceutical used? 4. Describe the findings of the second study. What is the clinical significance of the scan findings before and after chemotherapy? |
Bone: Osteosarcoma and 201TI
1. Increased uptake in the lateral margin of the distal metaphysis compatible with the known osteosarcoma. Relative photopenia medial to this uptake. 2. Yes, for staging to detect other sites of tumor. 3. 201Tl. 99mTc sestamibi can be used for the same purpose. 4. Prechemotherapy: very increased uptake in the osteosar coma. Postchemotherapy: resolution of the uptake. The degree of decrease in 2O1T1 uptake after therapy correlates with tumor response to chemotherapy and tumor necrosis. |
|
|
Previously resected chondrosarcoma. Evaluate for metastases.
1. Describe the bone scan findings. 2. Provide the differential diagnoses. 3. List at least three conditions that predispose patients to this condition. 4. List two other sites that are subject to the same process. |
Skeletal System: Avascular Necrosis
of Femoral Heads 1. Nonvisualization of the left ilium; leg length discrepancy as a result of high-riding left hip; and increased uptake both femoral heads, left worse than right. 2. The ilium has been surgically resected. Femoral heads: avascular necrosis, fractures, osteotomies; slipped capital femoral epiphyses in the appropriate age group. 3. Trauma, steroid administration, sickle cell disease, collagen vascular disease, chronic renal disease, aspirin, alcoholism, dysbaric conditions. 4. Humeral head, tarsal navicular. |
|
|
Patient ,4 is a 50-year-old woman with recurrent cellulitis and chronic edema of the left lower extremity. Patient B is a
60-year-old man with swelling in the left upper thigh for several months after femoral artery surgery. Radionuclide lymphoscintigraphy was performed for both patients. 1. What radiopharmaceutical is most commonly used in the United States for lymphoscintigraphy? 2. What is the differential diagnosis of chronic lower extremity edema if systemic disease, e.g., cardiac, hepatic, renal, have been excluded? 3. Describe the lymphoscintigraphic pattern in these two patients. 4. What are the diagnoses? |
Musculoskeletal System: Lymphoscintigraphy
of the Lower Extremities 1. Filtered 99nTc sulfur colloid. 2. Chronic venous insufficiency and lymphedema, primary or secondary. 3. A, Normal deep lymphatic flow to femoral and inguinal nodes on the right. Dermal backflow pattern on the distal left lower extremity. B, Abnormal focal accumulation in the medial left thigh. One superficial collateral lymphatic vessel on the right. 4. A, Lymphatic obstruction (left). B, Extravasation into a lymphocele (left). Right, Asymptomatic; normal. |
|
|
A 48-year-old patient with COPD and ciaudication. She has asthma. SPECT perfusion images (A, short-axis; B, verti
cal long-axis; and C, select gated poststress SPECT images). The left ventricular ejection fraction (LVEF) is 20%. 1. What is the appropriate stress technique for this patient? In what other patients is this the stress method of choice? 2. Why is this considered a second-line pharmacological stress agent? 3. Describe the SPECT image findings in this case. 4. What is the mechanism of cardiac uptake for 99mTc sestamibi and 99mTc tetrofosmin? |
Cardiovascular System: Dobutamine Stress
1. Dobutamine stress. Patients who are not candidates for either exercise, e.g., claudication, or vasodilator stress, e.g., patients with asthma. 2. The common occurrence of side effects including angina and the inability of a significant number of patients to tol erate the required dose. 3. Mild fixed anteroseptal perfusion defect with decreased wall thickening. Severe fixed inferior defect with absent wall thickening. Dilated left ventricular cavity. No reversibility. Myocardial thickening and wall motion signify functioning viable myocardium. 4. 99mTc sestamibi, an isonitrile monovalent cation, diffuses passively from the blood into myocardial cells because of its lipophilicity, then localizes in the mitochondria. 99mTc tetrofosmin, a diphosphene, has a similar uptake mechanism. |
|
|
A, Exercise myocardial SPECT perfusion studies. The patient's initial stress study acquisition (above) and repeat acquisition
(below), B, Sinograms for the first (left) and second (right) scans. 1. Describe the findings based on the SPECT images and sinograms. 2. Describe the purpose of the sinogram. 3. List other techniques in addition to the sinogram that can be used similarly. 4. Provide the diagnosis. |
Cardiovascular System: Patient Movement
Artifact 1. A, The first study (above) shows an abnormal configura tion of the anterior wall; the repeat study (below) is nor mal. B, The initial sinogram shows a discontinuity or break; the second is normal. 2. To visually present the raw unprocessed projection images to evaluate for patient motion. 3. Review SPECT projection data, image by image, or in cinematic display. 4. Artifact caused by patient motion. |
|
|
Stress and rest SPECT myocardial perfusion images and a single projection of unprocessed acquisition data from a cine
loop (right) are provided. 1. What radiopharmaceuticals can be used for this stress study? 2. Describe the SPECT findings and any additional information available from the cine loop stress and rest projection images. 3. List the differential diagnosis. 4. List the advantages of adding ECG-synchronization (gating) to SPECT myocardial perfusion imaging. |
Cardiovascular System: Breast Attenuation
1. 99mTc sestamibi (Cardiolite), tetrofosmin (Myoview), and not 201Tl because the gall bladder is seen. 2. Mild fixed defect in the anterior wall. Projection images: decreased uptake in the upper half of the heart at stress and rest in a curvilinear configuration. 3. Breast attenuation, anterior wall myocardial scar (infarction). 4. Assessment of regional wall motion, wall thickening, and ejection fraction. |
|
|
Dipyridamole (Persantine) sestamibi SPECT myocardial perfusion study. Short-axis (A) and vertical long-axis images (B)
are shown. 1. List the mechanism of action of dipyridamole. List foods and medications that counteract its pharmacological effect. 2. Describe the timing of radiotracer injection with respect to dipyridamole administration and the management of dipyridamole side effects. 3. Describe the SPECT image findings. 4. List maneuvers to deal with the problem of abdominal (liver and intestinal) activity. |
Cardiovascular System: Dipyridamole, Inferior
Ischemia, Overlying Bowel Activity 1. Dipyridamole inhibits the action of adenosine deaminase, thus increasing endogenous adenosine, a potent coronary artery vasodilator. Coffee, tea, caffeine-containing soft drinks or foods such as chocolate, theophylline, and aminophylline. 2. Dipyridamole is infused for 4 minutes. Radiotracer is given 3 minutes after completion of the dipyridamole infusion. Side effects can be reversed with intravenous aminophylline. 3. Mild to moderate fixed defect of the anterior wall. Severe, mostly fixed defect involving the entire inferior wall, but a small area of reversibility in the inferoapical-apical region. Dilated left ventricle. 4. Obtain delayed SPECT to allow additional hepatic clear ance or movement of bowel activity, have the patient drink water, or both. |
|
|
A 45-year-old woman with hypercholesterolemia. A, Short-axis and B, vertical long-axis SPECT stress myocardial perfusion
images, and raw data sequential projection images from the stress (C) and rest (D) scans. 1. Describe the SPECT perfusion image findings. 2. List three reasons to review the raw data projection images. 3. Provide any information available from the acquisition projection images. 4. What is the most likely diagnosis? |
Cardiovascular System: Attenuation Caused
by Change of Breast Position 1. Partially reversible perfusion defect in the apicalantero- septal wall. Mild fixed defect in the inferolateral wall. Dilated left ventricle. 2. To detect patient motion, camera malfunction, or attenuation. 3. Decreased radiotracer in the upper portions of the myocardium that appears somewhat different in location on the stress and rest projection images. 4. Position-dependent breast artifact. Concomitant ischemia may or may not be present. |
|
|
A 62-year-old man with known CAD had fixed defects with no reversibility on a 99mTc perfusion SPECT study at
another hospital. This is a rest-rest 20lTl SPECT study. A, Short-axis, B, vertical long-axis; C, horizontal long-axis. 1. Describe the SPECT findings on the initial rest and the 4-hour delayed rest study. 2. What is the clinical significance of these findings? 3. Based on the available evidence, should revascularization be considered? 4. What is hibernating myocardium? |
Cardiovascular System: 201TI Viability Study
1. Initial rest images show extensive defects: (1) the anterior wall extending to the apex, septum, and anterolateral wall; and (2) the inferolateral wall extending to the inferior and lateral regions. Delayed rest images show some improve ment in perfusion in the anterior wall extending to the apex and septum and anterolateral region. 2. There is viable myocardium in the left anterior descending (LAD) artery distribution. 3. Yes. 4. Chronic myocardial ischemia where both blood flow and function (contractility) are reduced. Although the myocar dium is viable, the lack of wall motion mimics infarction. |
|
|
Stress (top row), 4-hour delay (middle row), and 24-hour (bottom row) planar 201Tl planar images obtained in a patient
too heavy for the SPECT table. 1. What is the mechanism for 201Tl uptake at stress and rest? 2. What is redistribution? 3. Name the three views and describe the scintigraphic findings. 4. List other circumstances in which planar imaging may be preferable to SPECT. |
Cardiovascular System: Planar 201TI
with Ischemia 1. 2O1T1 behaves like a potassium analogue using the ATPase sodium-potassium pump. Almost 90% of thallium is extracted on first pass through the coronary circulation at normal flow. Uptake is proportional to blood flow. At high flow rates, extraction is less. Five percent of the adminis tered dose localizes in the myocardium. 2. After initial cellular uptake, 201Tl undergoes redistribution throughout the body. As 201Tl clears from the myocardi um, it is replaced by circulating 201Tl. This is the basis for the stress redistribution imaging strategy. Cold defects seen on early images are the result of decreased flow and there fore decreased 201Tl delivery. Ischemic myocardium will "fill in" on 2- to 4-hour delayed imaging. No fill-in is seen with infarct. With severe ischemia, e.g., hibernating myocardium, fill-in may require a longer time, up to 24 hours. 3. Lefi: left lateral; middle: anterior; right: left anterior oblique. Reduced radiotracer in the inferolateral-inferior region, which partially normalizes on the delayed 4-hour redistribu tion images and completely redistributes by 24 hours. 4. Claustrophobia. Some patients do not tolerate the SPECT camera, particularly a multiheaded camera. |
|
|
PET cardiac study using two different radiopharmaceuticals. Short, vertical, and horizontal long-axis images are
shown. Top row of each set is 13N ammonia. The bottom images are 18F FDG. 1. What physiological parameter does the 13N ammonia distribution reflect? 2. Similar information could be obtained using what other clinically used positron radiopharmaceutical? 3. What is the rationale for the use of 18F FDG? 4. Describe the image findings and interpret the results. |
Cardiovascular System: 13N Ammonia/FDG
Cardiac Viability Study 1. Myocardial perfusion. 2. 82Rb. 3. FDG is taken up by ischemic myocardium. 4. The I3N ammonia study shows decreased perfusion in the proximal two thirds of the lateral wall extending to the anterolateral and inferolateral regions. The FDG uptake is mismatched. Increased FDG uptake indicating ischemia is seen where the 13N ammonia images show hypoperfusion. Diagnostic of myocardial viability (hibernating myocardium). |
|
|
A 40-year-old patient with malignant lymphoma was treated with doxorubicin (Adriamycin). A radionuclide ventriculogram
(RVG) performed at the time of initial diagnosis reported a 60% LVEE A, Follow-up RVG with all 16 image frames and left ventricular time-activity curves (TACs) before (B) and after (C) chemotherapy. 1. Discuss sequential images and the TACs. 2. What is the likely diagnosis? 3. List features that should be included in reporting RVG or MUGA studies. 4. List three reasons why radionuclide ventriculography is preferred to echocardiography for monitoring left ventricu lar function. |
Cardiovascular System: Doxorubicin Toxicity
1. Sequential images (A) show a LVEF within normal range. The ventricle appears mildly dilated. End-systole is image number 7. TACs show counts for each of 16 frames of the gated acquisition. B is normal. C shows deterioration from baseline with a slower, broad diastolic upslope and decreased stroke volume (ESV-EDV). The pattern is com patible with ventricular dysfunction, predominantly diastolic, and deterioration compared with the baseline study. LVEF was calculated to be 50%. 2. Doxorubicin toxicity. 3. Qualitative assessment of cardiac chambers and great ves sels in terms of size and relationships, regional wall motion based on review of cinematic display, and quantitative analysis (LVEF). 4. Echocardiography is operator dependent, relies on visual estimates of LVEF, and may not be technically feasible in up to 30% of patients because of poor acoustic window. RVG is relatively free of operator-dependent factors, is generally reproducible within an institution and across institutions, and is not limited by acoustic windows. |
|
|
A 99mTc pyrophosphate study is obtained to evaluate for myocardial infarct in a patient with equivocal ECG and bor
derline enzyme levels. 1. What information should be obtained before the injection? 2. Describe the scintigraphic SPECT (A, transverse; B, coronal) findings in this patient. 3. Give a differential diagnosis of the scan finding. 4. Name another infarct-avid radiopharmaceutical. |
Cardiac: Pyrophosphate SPECT Infarct
1. The time of the suspected event. Depending on the time of the event and whether chest pain is ongoing, a perfusion SPECT study may be more appropriate. 2. Focal abnormal uptake is seen at the left apex. 3. Focal apical myocardial infarct, severe ischemia, aneurysm, focal myocarditis, focal pericardial calcification. 4. '"In antimyosin. |
|
|
Two patients have radionuclide blood flow imaging after right upper extremity injection.
1. Describe the route of the radiotracer in patient A. Give an interpretation. 2. What are the image findings and interpretation of patient B? 3. What radiopharmaceuticals could be used for this study? 4. What is the framing rate (seconds/frame) and minimum injected dose required to obtain a good flow study? |
Cardiovascular System: Superior Vena Cava
Obstruction 1. Subclavian vein, superior vena cava, right ventricle, lungs, left ventricle, carotids, aorta. Normal flow pattern. 2. Venous occlusion at the superior vena cava with collateral flow over the anterior chest. (This patient had lung cancer.) 3. Any 99mTc radiopharmaceutical. All that is needed is enough activity for a good flow study. 99mTc DTPA often is used because it is cleared rapidly by the kidneys and can be repeated if necessary. 4. 1 to 3 seconds/frame; 5 mCi or greater. |
|
|
A 62-year-old patient with right-sided chest discomfort and shortness of breath. A, Posteroanterior chest radiograph;
B, perfusion; C, ventilation. 1. Describe the ventilation perfusion image findings. 2. Interpret the study. Give your reasoning. 3. What is the likelihood of pulmonary embolus in this patient? 4. What are the most common chest x-ray findings in patients with pulmonary emboli? |
Pulmonary System: High Probability of
Pulmonary Embolus 1. Perfusion: decreased right lower lobe except for the superior segment. Ventilation: normal except for mildly truncated right lower lobe consistent with subpulmonic effusion. 2. High probability of pulmonary embolus. Mismatch between perfusion and ventilation in the basal segments. The perfusion defect is considerably larger than the pleural effusion on the radiograph. 3. Greater than 80%. 4. Most common: normal. Next most common: atelectasis. These are also the most common x-ray findings in patients determined by angiography not to have emboli. |
|
|
A 59-year-old patient with COPD complains of right-sided chest discomfort and shortness of breath.
A, Posteroanterior chest radiograph; B, lateral chest; C, perfusion; D, ventilation. 1. Describe the ventilation-perfusion image findings. 2. Interpret the study. 3. What is a stripe sign and what is its significance? 4. What is the physiological basis of a stripe sign? |
Pulmonary System: Stripe Sign
1. Decreased perfusion in the right upper lobe (apical and anterior segments). Stripe sign of the posterior segment of the right upper lobe. Normal ventilation. 2. Two segmental mismatches. High probability of pul monary embolus. 3. Its presence signifies perfused lung tissue between a perfu sion defect and the adjacent pleural surface. Its presence can be used to classify a segment as not related to pul monary embolus, and in some cases, lower the probability of a scan from intermediate to low. 4. Usually a manifestation of airway obstruction. The sign has been correlated with CT and PET showing spared per fusion of the cortex of the lung in asthma and emphysema. |
|
|
A ventilation-perfusion lung scan is ordered for increasing shortness of breath. Chest radiograph (not shown) findings
were negative. 1. Describe the scintigraphic findings (A, perfusion, anterior and posterior only; B, 133Xe washin-washout ventilation image sequence; C, CT). 2. What pulmonary embolus probability category would you assign? 3. Provide the differential diagnosis. 4. A chest CT was performed to further evaluate for the symptoms. What is the most likely diagnosis? |
Pulmonary System: Unilateral Matched
Ventilation-Perfusion Abnormality 1. Perfusion images: global decreased perfusion to the entire left lung, more striking than the ventilation. 133Xe ventilation images: decreased and delayed ventilation of the entire left lung. Washout images show no significant air trapping. 2. Low probability. 3. Hilar mass (lung cancer or adenopathy), severe unilateral parenchymal lung disease, Swyer-James syndrome, hypoplastic pulmonary artery, prior shunt for congenital heart disease. 4. Lung cancer. |
|
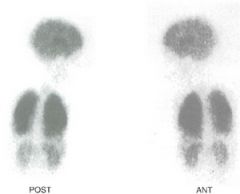
A 3-year-old child was referred for a 99mTc macroaggregated albumin (MAA) study.
1. Describe the scintigraphic findings. 2. What is the diagnosis? 3. Describe the radiopharmaceutical's mechanism of uptake. 4. What are contraindications to this study? |
Pulmonary System: Right-to-Left Shunt
Demonstrated by 99mTc MAA 1. Uptake of the radiotracer in the brain, lungs, kidneys, and liver. 2. Right-to-left shunt. 3. 99mTc MAA particles are larger than capillary size. When given intravenously, the particles occlude the first arteriolarcapillary bed they reach normally, the lungs. With a rightto- left shunt, some will bypass the lungs and be delivered systemically in proportion to the size of the shunt. 4. Relative contraindications include pregnancy, severe pul monary hypertension, and right-to-left shunt. There are no absolute contraindications. |
|
|
A 55-year-old patient with a remote history of thrombophlebitis in the left thigh has recurrent similar pain. A Foley
catheter is in place. 1. What is the radiopharmaceutical and scintigraphic study? 2. What is its mechanism of uptake? 3. What are the scintigraphic findings? 4. What are its clinical indications? |
Thrombophlebitis: AcuTect (99mTc apcitide)
1. Radionuclide venogram with AcuTect (<J9mTc apcitide). 2. AcuTect is a synthetic peptide that binds to the glycoprotein GPIIB/IIIa receptors on the surface of activated platelets. 3. Increased uptake in the left deep venous system extending from the proximal to distal thigh consistent with acute deep venous thrombophlebitis. Diffuse increased uptake is seen throughout the soft tissue of the left lower extremity. 4. To differentiate acute thrombophlebitis from old inac tive thrombophlebitis. It also can be used to diagnose acute thrombophlebitis when Doppler ultrasonography is nondiagnostic. |
|
|
A 56-year-old paraplegic patient has fever of uncertain origin. No localizing signs or symptoms are present.
1. Which radiopharmaceutical was used? What others could be used for this purpose? 2. Which organ receives the highest radiation absorbed dose? Estimate the dose. 3. What is your interpretation of this whole-body scan (A) and pelvic spot (B)? 4. What is the photopeak(s) of the radionuclide used? What is its half-life? |
Infection and Inflammation: inln Oxine
WBCs—Right lleum Osteomyelitis 1. "'In oxine or 99mTc HM-PAO leukocytes. 67Ga could also be used. The intense spleen uptake is consistent with a radiolabeled leukocyte study; "'In oxine leukocytes were used. The image resolution is poor compared with 99mTc leukocytes. 2. Spleen, approximately 15 to 20 rads. 3. Abnormal focal uptake in right groin (there has been a femoral line) and in the right ileum, indicating osteomyelitis. 4. 173, 247 keV. Physical half-life is 77 hours. |

