![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
The 2 most common forms of inflammatory bowel disease (IBD) are distinct, immunologically mediated, idiopathic disorders termed _____________ and ___________.
|
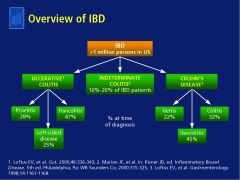
ulcerative colitis (UC) and Crohn’s disease (CD)
Because symptoms are often similar in UC and CD, a differential diagnosis is not always possible; therefore, 10% to 20% of patients with IBD are considered to have indeterminate colitis. |
|
|
Inflammatory bowel dz (IBD) can be broken down into ulcerative colitis (UC) or Crohn's dz (CD). Which is characterized by...
A. diffuse mucosal inflammation in a continuous pattern limited to the colon. It usually begins in the rectosigmoid area and proceeds proximally, but it may develop in extensive areas of the colon at the same time B. by transmural inflammation in a discontinuous pattern that can occur in any part of the gastrointestinal tract from mouth to anus. The distal ileum and colon are the most common sites of involvement. |
A. diffuse mucosal inflammation in a continuous pattern limited to the colon. It usually begins in the rectosigmoid area and proceeds proximally, but it may develop in extensive areas of the colon at the same time= ULCERATIVE COLITIS
B. by transmural inflammation in a discontinuous pattern that can occur in any part of the gastrointestinal tract from mouth to anus. The distal ileum and colon are the most common sites of involvement = CROHN'S DZ |
|
|
What is FALSE about inflammatory bowel dz?
A. Both Ulcerative colitis and Crohn's dz have a bimodal distribution (dip in 40s) B. Tends to run in families so there are genetic and environmental triggers C. IBD is more prevalent among higher economic classes and white-collar rather than blue-collar workers D. cigarette smoking has an exacerbating effect in CD and a protective effect in UC E. All are true |
E. All are true!
|
|
|
[ Crohn's dz / Ulcerative colitis ] starts in the sigmoid rectum area and then proceeds proximally.
|
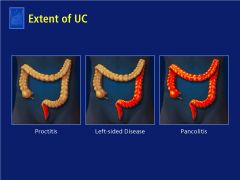
Ulcerative colitis!
|
|
|
In Crohn’s dz, inflammation can extend anywhere between the mouth to anus. Most patients have involvement of what areas? Chron’s dz is divied up into three phenotypes: what are they?
|

AREA: Most patients have involvement of R colon and terminal ileum.
Three phenotypes: inflammatory, strictures, or penetrating/fistula Chron’s dz. Patients with stricturing and fistulas tend to have more aggressive and advanced dz playouts. |
|
|
In Chron’s dz can extend anywhere between the mouth to anus! Most patients have involvement of R colon and terminal ileum. Chron’s dz is divied up into three phenotypes: inflammatoroy, strictures, or penetrating/fistula Chron’s dz. Patients with which phenotypes tend to have more aggressive and advanced dz playouts.
|
stricturing and fistulas
|
|
|
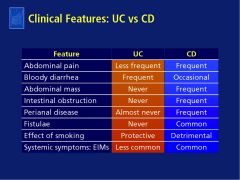
Compare ulcerative colitis to crohn's dz with regards to...
A. abdominal pain (less frequent, frequent) B. bloody diarrhea (frequent, occasional) C. abdominal mass (frequent, never) D. intestinal obstruction (frequent, never) E. perianal dz (almost never, frequent) F. Fistulae (Common, Never) G. Effect of smoking (detrimental, protective) |
|
|
|
What is the number one cause of bloody diarrhea?
A. Infectious colitis B. Inflammatory bowel dz C. Irritable bowel syndrome D. Ischemic colitis |
A. Infectious colitis
SO, need to rule out infection! |
|
|
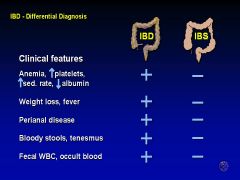
What are the differences between irritable bowel syndrome and inflammatory bowel dz? (5)
|
|
|
|
True or False:
Irritable bowel syndrome can yield weight loss, fever, bloody stools, and tenesmus. |
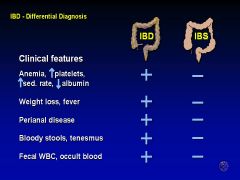
FALSE!
|
|
|
What is the role of radiology in inflammatory bowel dz?
What is the role of endoscopy in IBD? |
RADIOLOGY: Helpful to assess extent of small bowel inflammation (CTE or MRE), look for intra-abdominal abscess, stricture, malignancy, or toxic megacolon.
ENDOSCOPY: confirm diagnosis, differentiate UC from CD, obtain histologic confirmation of severity and extent, surveillance for neoplasia. |
|
|
What is FALSE about endoscopic appearances/findings for inflammatory bowel dz?
A. Ulcerative colitis can be defined in part via endoscopy as mild, moderate or severe whereas Crohn's does not have those distinctions B. Crohn's dz yield irregular "punched out" ulcers C. Crohn's dz yields macroulcerations and pseudopolyps, unlike ulcerative colitis D. mild UC will reveal erythematous-looking rectal mucosa with a “sandpaper” appearance and loss of vascularity |
FALSE: C. Crohn's dz yields macroulcerations and pseudopolyps, unlike ulcerative colitis
This happens in BOTH UC and CD! Is also called "cobblestoning" |
|
|
TRUE OR FALSE:
Irritable bowel syndrome never has blood in stool or fecal leukocytes. |
TRUE
|
|
|
What is FALSE about extraintestinal manifestations of IBD?
A. Occur in 1/3 of patients with IBD B. are immune-mediated changes of the joints, spine, eye, skin, and hepatobiliary tract. C. in pediatric population, at diagnosis, EIMs freqeuntly predominate over GI symptoms D. can demonstrate gender preference. Men: erythema nodosum, Women: anklyosing spondylitis |
NOT WHOLLY TRUE: D. can demonstrate gender preference. Men: erythema nodosum, Women: anklyosing spondylitis
Yes, EIMs can demonstrate gender predilection, but it is MEN: PSC, anklyosing sondylitis WOMEN: iritis/uveitis, erythema nodosum |
|
|
True or False:
For ulcerative colitis and crohn's dz, we use the SAME meds. |
TRUE!
The only time it makes a big difference is when you start thinking about whether patient needs to go to surgery for treatment of complication and/or lack of response to meds. Sulfasalazine, Mesalamine: best results with colonic disease. Immunomodulators: 6-MP/Imuran, Methotrexate: good and cheap but take 3-4 months to really kick in Antibiotics (especially those aimed at enteric flora: Cipro, Flagyl, etc.)Use even in absence of infection because good for IBD flares. Downside is metallic taste with these meds and CI with any alcohol at all. With prolonged use, risk of peripheral neuropathy SURGERY DOES NOT CURE!! |
|
|
True or False:
Surgery is not a curative treatment for inflammatory bowel diseases. |
HALF FALSE!
Surgery can't cure Crohn's but it can cure UC. |
|
|
Regarding risk of serious infections while being on certain IBD medications, patients currently using corticosteroids or narcotic analgesics had a significantly [ higher / lower ] risk of developing a serious infection whereas current use of infliximab or immunomodulators (6MP/AZA/MTX) yielded a significantly [ higher / lower ] risk of developing a serious infection.
|
HIGHER : corticosteroids or narcotic analgesics
LOWER: infliximab or immunmodulators |
|
|
DEXA screening is suggested for postmenopausal women or men:
- over the age of 50 - in patients with prolonged coorticosteroid use (greater than ____ consecutive months or recurrent courses) - patients with a personal history of a low trauma fracture - patients with hypogonadism |
3 consecutive months
|
|
|
TRUE OR FALSE:
People with inflammatory bowel dz have an increased risk of developing colon cancer. |
TRUE
so, begin surveillance colonoscopy: after 8-10 yrs of pan colitis --> screen Q 2 yrs after 15 yrs of left-sided colitis --> screen Q 2 yrs after 20 yrs of any colitis --> Q 1 yr |
|
|
What is the functional unit of the small bowel?
A. Plicae circulares B. Villi C.Microvilli |
B. Villi
|
|
|
On average, the luminal fluid load of the gut is approximately 9 L per day, composed of oral intake and endogenous secretions. Of this volume, approximately 8.8 L per day or more is absorbed. This process represents a highly efficient rate of absorption of greater than 98%, most of which occurs in the _____________ .
|
small intestine
|
|
|
Where and how are Na, Cl, and water absorbed in the small intestine?
|
ALong the entire length of the small intestine, no one particular area. While Na is absorpbed by both active & passive mechanisms, water follows passively. A variety of transport proteins are required for intestinal transport of water and electrolytes and are grouped into three major classes: pumps, channels, and carriers.
|
|
|
What is FALSE about nutrient absorption?
A. Monosaccharides, amino acids and small peptides are transported passively and actively B. For fats, after lipolysis to fatty acids and glycerol, and emulsficiation with bile salts, there is active transmembrane transport C. medium chain TG are absorbed directly and don't need bile salts D. The first part of the small intestine, the duodenum, absorbs iron and folic acid. |
FALSE IS: D. The first part of the small intestine, the duodenum, absorbs iron and folic acid.
The small intestine absorbs CALCIUM and iron. Folic acid is absorbed primarily in the jejunum. |
|
|
Where is each nutrient absorbed in the small intestine?
A. B12 B. bile salts C. Calcium D. Fat E. Iron |
A. B12 and B. bile salts - ileum
C. Calcium and E. Iron - duodenum D. Fat - jejunum and ileum |
|
|
Detail Vitamin B12 absorption.
|
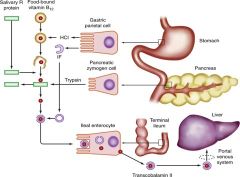
Food-bound B12 is released by gastric acid and pepsin and binds preferentially by salivary R protein in the stomach. Proteolysis of R protein by trypsin releases B12 for binding to IF (intrinsic factor, secreted by gastric parietal cells). The sub-sequent binding and uptake of the IF-B12 complex occurs through a specific receptor-mediated process on the brush border membrane of ileal enterocytes. Vitamin B12 is released at an intracellular site, transported across the basolateral membrane, and taken up by transcobalamin II for transport to the portal circulation.
|
|
|
Define diarrhea. (# bowel movements per day or fecal weight, acute v chronic delineation, 3 more types
|
Diarrhea is 3+ bowel movements of liquid stool per day and/or fecal weight > 200 gms/day.
Acute < 4 weeks, Chronic > 4 weeks • Inflammatory (mucoid/bloody stools with fecal leucocytes, tenesmus, abdominal pain, fever) , non-inflammatory (watery stools, frequently large volume, no blood or mucous), or fatty (oily, bulky, foul smelling difficult to flush and float on water) Additionally there is osmotic diarrhea and secretory diarrhea. |
|
|
[ Osmotic / Secretory ] diarrhea leads to increased luminal osmolarity and water influx into lumen. This type of diarrhea stops upon fasting.
|
Osmotic diarrhea.
Stool osmotic gap > 50 Secretory diarrhea is excessive secretion of electrolytes and water. Watery stool that typically continues on fasting. Enterotoxins and secretory tumors and bile salt excess are causes. |
|
|
The following cause what type of diarrhea?
Enterotoxins: Vibrio cholerae, E coli, Staph aureus, Bacillus cereus, Norwalk virus, etc. Secretory tumors: VIP, serotonin, calcitonin, gastrin, histamine Others : Bile salts A. Osmotic diarrhea B. Secretory diarrhea C. Inflammatory diarrhea |
B. Secretory diarrhea
Inflammatory diarrhea is caused by: Infectious: Shigella, campylobacter, EHEC, salmonella, yersinia, T.B, amoebae, C diff IBD: Crohn’s disease, ulcerative colitis Bowel ischemia, radiation injury |
|
|
The following cause what type of diarrhea?
Infectious: Shigella, campylobacter, EHEC, salmonella, yersinia, T.B, amoebae, C diff IBD: Crohn’s disease, ulcerative colitis Bowel ischemia, radiation injury A. Osmotic diarrhea B. Secretory diarrhea C. Inflammatory diarrhea |
C. Inflammatory diarrhea
Intestinal mucosa inflamed and ulcerated Mucoid/bloody stools, + fecal leucocytes Tenesmus, abdominal pain, fever |
|
|
For Giardiasis, what is the treatment?
A. Flagyl B. Oral vancomycin C. Tetracycline |
Flagyl 250 mg PO thrice daily for 5 days
Alternatives: Nitazoxanide, tinidazole (2 g PO 1 dose), quinacrine, furazolidone, or paromomycin |
|
|
Pseudomembranous colitis is the most common cause of in-hospital diarrhea and is strongly associated with C dificile infection, usually after antibiotic therapy.
What is the treatment? A. Flagyl B. Oral vancomycin C. Tetracycline |
BOTH
A. Flagyl B. Oral vancomycin Note: Diagnose pseudomembranous colitis by stool for endotoxin A & B. |
|
|
If factitious diarrhea (due to use of laxatives), check the .....
|
pH as it will be more acidic than usual stool.
|
|
|
What is celiac dz?
|
Allergy to "gluten" portion of wheat, rye and barley. It is a gluten induced immune mediated process. Genetic susceptibility in HLA-DR3, DQ2, DQ8. Immune response causes villus atrophy!
Symptoms: diarrhea, steatorrhea, flatulence, weight loss. Extra-intestinal features: Fe deficiency anemia, osteopenia, bleeding tendency, vitamin deficiencies, neuropathy, ataxia. |
|
|
What are the symptoms of Celiac dz? How do you diagnose it?
|
Symptoms: GI (Diarrhea, steatorrhea, flatulence, & weight loss. Diarrhea often episodic, upto10 stools per day) and extra-intestinal (Fe deficiency anemia, osteopenia, bleeding tendency, vitamin deficiencies, neuropathy, ataxia etc)
Diagnosis: SEROLOGY. IgA. Histology is highly suggestive but not diagnostic. From 3 biopsies from distal duodenum showing: Decreased villous height to crypt depth, Decreased epithelial surface cell height, Increased lymphocytic infiltration of the mucosa. On endoscopy, see scalloped duodenal folds. |
|
|
This condition is common in tropical residences, soldiers deputed in tropical areas. GI symptoms include diarrhea, steatorrhea, weight loss. Macrocytic anemia can occur since the distal small bowel (where B12 and folic acid are normally absorbed) is affected or
malnutrition is at play. What is the treatment? |
Tropical Sprue
Improve with tetracycline and folic acid. |
|
|
What is described:
Central abdominal pain after eating. Atherosclerosis/stenosis of the SMA. Mild postprandial discomfort to incapacitating pain, vomiting, diarrhea & weight loss, to infarction/gangrene of the bowel. A. Chronic intestinal angina B. Acute mesenteric ischemia C. Small intestine bacterial overgrowth D. Short Bowel Syndrome |
A. Chronic intestinal angina
|
|
|
What are the precipitating disorders of acute mesenteric ischemia (AMI)?
|
Symptom is abdominal pain.
Precipitating disorders include: Patient older than 50 years old, long standing CHF, cardiac arrhythmias, recent myocardial infarction, hypotension, recent cardiopulmonary resuscitation |
|
|
In patients who are survivors of CPR with unexplained bacteremia or sepsis, suspect...
A. Mesenteric artery embolus B. Non occlusive mesenteric ischemia C. Mesenteric venous thrombosis D. Focal segmental ischemia |
B. Non occlusive mesenteric ischemia
|
|
|
_____________ is common in people who have had multiple abdominal surgeries.
A. Small intestine bacterial overgrowth B. Acute mesenteric ischemia C. Short bowel syndrome |
A. Small intestine bacterial overgrowth
|
|
|
Infectious diarrhea is the most common cause of acute diarrhea and is further subdivided into invasive and non-invasive. Which belongs to each group?
A. Cryptosporidia, GIardia, toxigenic E.coli B. Shigella, Salmonella, invasive E.coli and C.difficile |
INVASIVE: B. Shigella, Salmonella, invasive E.coli and C.difficile
NON-INVASIVE: A. Cryptosporidia, GIardia, toxigenic E.coli |

