![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
2 most common western causes large bowel obstruction
|
colorectal ca
inflammatory stricture (esp second to diverticular disease) colonic volvulus (also: faecal impaction in elderly) |
|
|
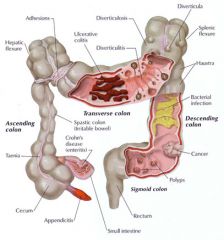
differentiate between diverticulosis, diverticular disease and diverticulitis
|
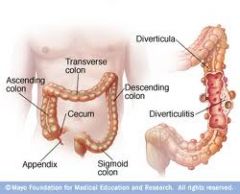
diverticulOSIS- diverticular are present
divertivular DISEASE- symptomatic diverticuLITIS- inflammation |
|
|
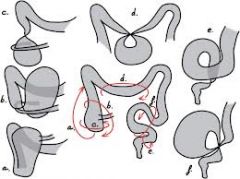
pathology of divertucular disease:
- loc - cause - process - age |
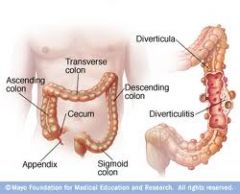
SIGMOID, right
low fibre = mucosal herniation through wall 33% have by 60yrs |
|
|
clinical features S&Ss of diverticulITIS
|
LIF pain/ tenderness (colicky- relieved by defaecation)
septic/ feverish (↑WCC, ↑ESR/CRP) altered BOWEL habit (dia/const, BLOOD) 3 F's: Fever, Fast pulse, Flushed |
|
|
Dx by Ix's of diverticulitis/ diverticular disease (3)
|

PR examination (abscess, colorectal ca)
SIGMOISOSCOPY Ba ENEMA |
|
|
treatment/ management for diverticular disease (3)
- which abx's indivated in inflammation |
IV fluids & NBM (bowel rest)
IV abx's (-itis)....metranidazole high FIBRE diet |
|
|
some complications of diverticular disease/ -itis that may require surgery
|
abscess
perforation haemorrhage fistula stricture |
|
|
2 surgical ops fro diverticular disease
|
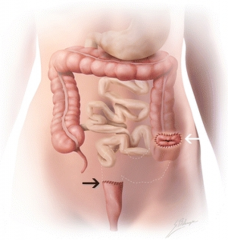
1) artmann's procedure- 2 step: resection & colostomy....later closure.
2) primary resection & anastomosis (elective) |
|
|
syptoms of acute & chronic colitis
|
diarrhoea +/- BLOOD....dehydration
abdo cramps sepsis (3F's: Fever, Fast pulse, Flushed) wt loss, anaemia |
|
|
Dx by Ix's of acute/chronic colitis (inflammatory, ischaemia & infective)
|
(basics: FBC, CRP, coeliac, coagulation, U&E's...)
STOOL.....?infection ★SigmoidoSCOPY + BIOPSY★ AXR..... (ischaemic- "thumb printing") Ba enema |
|
|
3 types of acute and chronic colitis beginning with I
|
Inflammatory (IBD: Crohn's & UC)
Ischaemic Infective |
|
|
general treatment of inflammatory colitis (Crohn's & UC)
|
IV fluids
steroids NBM- bowel rest ?surgery |
|
|
AF/emboli/ vasculitis/ atherosclerosis with abdo pain suggests what
which area commonly affected & why |

ischaemic colitis....'mesenteric angina'
- splenic flexure & rectum (points of less blood supply) |
|
|
what classical AXR/ Ba enema sign found in ischaemic colitis due to submucosal swelling
|

"thumb-printing"
|
|
|
what's angiodysplasia:
- where in wall affected - where in colon - man sym - age |
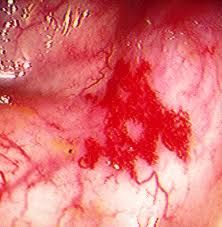
submucosal arteriovenous malformations
RIGHT colon (or anywhere) fresh BLOOD PR elderly unknown aetiology |
|
|
Dx by Ix of colonic angiodysplasia
treatment |

★angiography★
colonoscopy INJECTION- embolisation Endoscopic ABLATION SURGICAL resection |
|
|
S&Ss large bowel obstruction
|
colicy abdo pain
distention N&V high-pitched tinkling or NO BS! constipation |
|
|
how to differentiate between small and large bowel obstruction on AXR
|

small- plicae circularis completely ENCIRCLE lumen
large- haustra DON't cover lumen width |
|
|
treatment of a sigmoid volvulus
|

flatus tube (sigy)
resection |
|
|
what's the likely type of colinic obstruction;
- elderly, debilitated, - malignancy, low electrolytes, recent surgery - nausea, post-prandial abdo pain - may have wt loss |

PSEUDO-obstruction (no cause found)
|
|
|
2 types of microscopic colitis
|
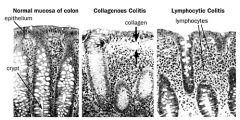
changes in walls --- cause diarrhoea
|
|
|
pathology on appearance and histology of abx-induced colitis / "pseudomembranous" colitis
|
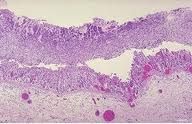
psuedomembrane
extra FIBROPURULENT exudate surface layer....volcano lesions (fibrin, pus, neutrophils, debris) |
|
|
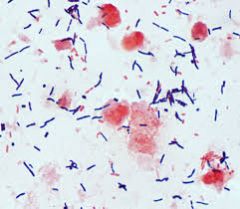
what's the cause of pseudomembranous colitis
- gram stain |

broad spectrum abx allow overgrowth of Cl.DIFF
toxin A & B = massive diarrhoea & BLOOD - gram +ve aerobic bacilli |
|
|
treatment of pseudomembranous abx-induced colitis
|
IV fluids
metranidazole/ vancomycin (colectomy if fatal) |
|
|
biospy & pathology of microscopi collagenous colitis
|

thickening of basement membrane with submucosal collagen
patchy intra-epithelial inflammatory cells no chronic architectural change |
|
|
what change does microscopic lymphocytic colitis show on histopathology
|
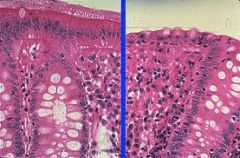
increased INTRAEPITHELIAL lymphocytes
no thickening of basement membrane |
|
|
why is microscopic colitis (collagenous or lymphocytic) hard to dx without histopathology (biopsy)
|
endoscopy looks normal
|
|

which likely type of colitis?
- telangectasia (pic). hx of cervical/ rectal ca & radiotherapy - diarrhoea - acutely inflamed mucosa, cryptitis, but no architectural abnormality |

radiation colitis
|
|
|
2nd most common cause cancer deaths UK ?
56% over what age |
colorectal cancer
>70yrs (screening >50yrs) |
|
|
aetiology/ predisposing factors to colorectal cancer
- lifestyle - medical conditions (OMH/ FH) |
neoplastic polyps (benign)
UC/ Chron's FAP & HNPCC prev ca low fibre, ↑red/processed meat, smoking, alcohol, obesity |
|

FAP has a mutation in which gene
|

APC
|
|
|
differentiate an adenoma from an adenocarcinoma
|
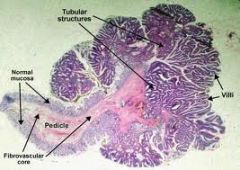
ADENOMA (pic): glandular, tubular, villous, benign, well differentiated, DYSPLASTIC
ADENOCARCINOMA: variable differentiation, INVASIVE |
|
|
Duke's staging of colorectal carcinoma
|
A- confined to bowel wall
B- through wall C- regional lymph nodes D- mets |
|
|
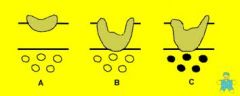
what are the different 'T' stages for histological TNM staging of cancer
|
Tumour SIZE:
T1- submucosa T2- muscle T3- through muscle T4- adjacent structures (adventita/ peritoneum) |
|
|
2 common sites for colorectal carcinoma spread
|

liver
lungs |
|
|
clinical presentation, S&Ss of colorectal carcinoma
- LEFT - RIGHT - both |
LEFT: BLOOD pr, altered BOWEL habit, tenesmus, pr MASS
RIGHT: ↓wt, anaemia, abdo pain (lower) - distention (obstruction), mass, hepatomegaly, lymphadenopathy, |
|
|
Dx by Ix of colorectal cancer
|

FBC (↓Hb), LFTs (mets?) FOB (screening)
★★COLONOSCOPY + biopsy★★ ba enema CT/ MRI/ liver USS - staging |
|
|
imaging to stage colorectal ca
|

CT/ MRI
liver USS CXR |
|
|
S&S of colorectal polyp (1)
|

blood/ mucus PR
(maybe- diarrhoea/constipation, abdo pain) |
|
|
types of surgery of colorectal cancer (only curative option)
|
colostomy
resection + colostomy stenting |
|
|
how is treatment for colon and rectal cancer different
|
COLON- (5-FU)Chemo adjuvant for advanced
- colectomy RECTAL- radiotherapy adjuvant and palliative - abdomino-pelvic perineal excision - anterior resection |
|
|
compare FAP & HNPCC:
- onset - inheritance pattern - what's the defect - which FAP gene |
FAP: early onset, autosomal DOMinant, defective tumour supression- APC gene.
HNPCC: late onset, autosomal DOMinant, defect in DNA mismatch repair |
|
|
how & where is entry into the large bowel
|
ileocaecal valve via gastro-ileal reflex
|
|
|
what are pugatives used for
how do they work when are they indicated |
used for constipation:
- ↑peristalsis +/- soften stool - when 'straining' dangerous (angina) - painful defaecation (haemorrhoids) - pre-op - drug-induced/ bedridden constipation |
|
|
4 types of pugatives
|
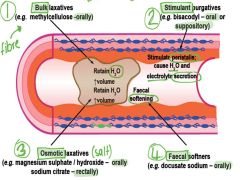
BULK/ OSMOTIC, STIMULANT, SOFTENERS
|
|
|
SE's of diarrhoea (3)
|
dehydration
metabolic acidosis (HCO3- loss) hypokalaemia (K+ loss) |
|
|
3 treatments of severe acute diarrhoea
|
maintain fluid & electrolytes
anti-infective (if applicable) non-antimicrobial anti-diarrhoeal agents (symptomatic) |
|
|
4 types of diarrhoea
|
OSMOTIC
HYPERMOTILITY (↓transit) INFLAMMATORY (↑ permeability) SECRETORY (CFTR stimulation) |
|
|
how does cholera cause diarrhoea
|
produces toxins → stimulates Gs → ↑adenylyl cyclase → ↑cAMP → ↑CFTR stimulation → ↑Cl- + Na+ secretion
|
|
|
how do oral rehydration salts reduce diarrhoea
- which transport protein is exploited |

Na+ allosterically increases affinity for GLUCOSE on SGLT1
↑Na+ absorbtion = ↑H2O absorption |
|
|
why do morphine-like/ opiates cause constipation
|
have anti-diarrhoeal-like effects
- inhibit enteric nerones - decrease peristalsis, ↑segmentation - ↑fluid absorption - sphincter constriction |
|
|
3 anti-motility / antidiarrhoeals
|
coedine
loperamide (↑gastric motility) diphenoxylate |
|
|
in a screening test what are these 4 main validity factors;
- sensitivity - specificity - positive predictive value - negative predictive value |
SENSITIVITY: % with disease correctly identified +ve
SPECIFICITY: % w/o disease correctly identified -ve +ve PREDICTIVE: % +ve who actually have the disease -ve PREDICTIVE: % -ve who actually don't have disease |
|
|
7 key criterias for a screening prog
|
common/serious condition
latent periods (w/o screening) available effective Rx available early detection minimal risk!!!!!!! cost effective £££ |
|
|
what test is used for colorectal ca screening
- what Ix's offered fro +ve result |
FOB
+ve = sigmoidoscopy/ colonoscopy +/- biopsy |

