![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
16 Cards in this Set
- Front
- Back
|
The plasma membrane of the heart is termed the ________. Beneath that is a rich serpentine network of intracelular tubules termed the _____________.
|
sarcolemma; sarcoplasmic reticulum
|
|
|
Which of the following is FALSE?
A. The function of the sarcolemma and sarcoplasmic reticulum is to maintain and regulate calcium flux in the cardiac muscle. B. The heart has a rich supply of mitochondria which might compose up to 33% of the weight of the myocyte. C. The sarcomere is composed of Z lines, the A band, and the I band. D. Tropomyosin functions to turn on and off cross-bridge formation. |
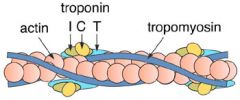
The false thing is: D. Tropomyosin functions to turn on and off cross-bridge formation. It is actually TROPONIN that turns on and off cross-bridge formation! Tropomyosin lends structural rigidity to the sarcomere. Troponin itself has three components: Troponin C which is responsible for the binding of Calcium; Troponin I which predominates during diastole and inhibits cross-bridge formation in the absence of the binding of calcium; Troponin T which acts as a structural unit in binding to the protein actin to lend structural rigidity to the thick filament.
|
|
|
What does excitation-contraction coupling refer to? Describe the process.
|
The process of converting and electrical signal in cardiac muscle into active shortening and tension development is termed excitation-contraction coupling.
- an AP is propagated along the sarcolemma and into the T-tubule system of the cell - depolarization of that sarcolemmand T-tube system --> small release of calcium from subsarcolemmal basement membrane which induces a large release of calcium from the SR. - free [calcium] increases and is preferentially bound by the calcium binding protein troponin - since calcium is bound to troponin, Troponin I (which is normally inhibiting cross-bridge formation) is removed and actomyosin cross-bridges form - formation of the actomyosin cross-bridges activates the ATPase activity of heavy myosin and splits ATP, resulting in the production of energy and further cross-bridge formation - active shortening of the muscle ensues - relaxation ensues by the ACTIVE pumping of the calcium from the troponin binding site back into the sarcoplasmic reticulum, reducing systolic free calcium concentrationa dn tereby inhibiting cross-bridge formation. |
|
|
Greater force of contraction (positive ionotropic effect) is manifested with norepinephrine, epinephrine, isoproterenol. At the fundamental excitation-contraction coupling level, greater force of contraction is associated with greater....
|
greatercalcium availability. The SR is well stocked with Calcium.
|
|
|
The electrical system of the heart is a self-contained unit. It doesn't require CNS activity. The inherent pacemaker of the heart is the SA node. From there, conduction travels along the intra-atrial pathways adn converge on the AV node. From the AV node the AP is slowed and propagated into the His-Purkinje system which is then propagated to each individual cardiac muscle cell. What is the importance of the slowed conduction through the AV node?
|
The AV node doesn't have fast Na channels. The slowing allows for mechanical coupling of atrium and ventricle.
|
|
|
State what ECG marking equates to the described event:
1. depolarization of ventricles 2. depolarization of atria 3. time it takes for AP to traveres the intra-atrial pathways --> AV -> His purkinje 4. ventricular repolarization |
1. depolarization of ventricles : QRS complex
2. depolarization of atria : P wave 3. time it takes for AP to traveres the intra-atrial pathways --> AV -> His purkinje: PR interval 4. ventricular repolarization: T wave |
|
|
Which of the following would be an effect of increased parasympathetic tone in the heart, via ECG reading?
A. More P waves in a given time period B. Longer PR intervals in a given time period C. Wider QRS complexes D. Elevated S-T segments |
B. Longer PR intervals in a given time period
this signals decreased AV conduction |
|
|
Flow, pressure and resistance. How are these related?
(hint: Ohm's law) |
Flow = change in pressure / resistance
Note that resistance is inversely proportional to radius^4 such that if the radius of a given tube, say, narrows. It does so to the power of the fourth! And resistance will increase substantially! |
|
|
What are the normal parameters of pressure in each of the areas of the heart listed below?
A. R atrium B. R ventricle C. pulmonary artery D. L atrium E. L ventricle F. aorta |
A. R atrium: 5 mmHg
B. R ventricle: 20/0-5 C. pulmonary artery: 20/10 D. L atrium: 5-10 mmHg E. L ventricle: 120/5-10 F. aorta: 120/80 |
|
|
Regarding the cardiac cycle, just prior to the onset of the inscription of the P wave, left ventricular pressure ranges from __________ mmHg. With active contraction of the atria, the volume of the left ventricle increases and the pressure slightly increases with this volume too, eventually reaching the end diastolic pressure of _____ mmHg. During isovolumetric contraction phase, the pressure increases to about _______ mm Hg.
|
just prior to the onset of the inscription of the P wave, left ventricular pressure ranges from: 0-5 mm Hg
end diastolic pressure of 5-10 mmHg isovolumetric contraction phase to about 80 mm Hg |
|
|
Just prior to the onset of ventricular systole, there is relatively little flow into the L ventricle and the volume present is called ________ and yields a pressure actually called the _________ of the heart and is responsible for setting the resting tension of the intact myocardium. In normal humans, the [first blank] is ~ _________ mL.
|
just prior to the onset of ventricular systole, the volume in the L ventricle is called the END DIASTOLIC VOLUME, and it's pressure is called the PRELOAD. End diastolic volume usually amounts to ~ 140 mL in the average person.
|
|
|
Describe the cause for S2, S2, S3 and S4.
|
Normal
S1: Closing of the mitral and tricuspid valves S2: Closing of the aortic and pulmonic valves Usually abnormal: S3: normal in young individuals. otherwise, pathalogic when present. indicates a decreased compliance of the L ventricle. S4: sound immediately before the first heart sound. indicates decreased L ventricular compliance. |
|
|
The heart is capable of functioning independently of the central nervous system but the CNS can modulate the rate and contractility of the heart. The sympathetic nervous system from C___ to C___ innervates both atria and ventricle.
|
C3-C5
|
|
|
True or False:
The vagus, CN X, innervates the atria, especially the SA node and AV node, but has little vagal innervation of the ventricle. |
True
|
|
|
Interventions that influence ventricular preload do so by affecting the relative or absolute change in ___________ ; the two principle determinants of afterload are _______ and ________.
|
Preload interventions target the INTRAVASCULAR VOLUME.
Afterload is determined by SYSTOLIC PRESSURE and VENTRICULAR RADIUS. |
|
|
ATP is consumed more during...
A. isometric contraction of the myocardium B. isotonic contraction of the myocardium |
A. isometric contraction of the myocardium
2-3 times more ATP is consumed during isovolumetric contraction! |

